A 56-year-old woman presented with midback pain radiating across the left lower chest and abdomen as well as lower back pain radiating to the left hip and leg. There was no history of trauma. The physical examination was normal except for decreased sensation over the dorsum of the left foot. There were no signs of myelopathy. Magnetic resonance imaging (MRI) revealed lumbar stenosis and an expansile sclerotic lesion within the T12 vertebral body, which eroded the posterolateral cortical margins, extended into the soft tissue, and substantially compressed the spinal cord (Fig. 1). She was admitted to the hospital and scheduled for a biopsy.
Computed tomography (CT) scans prior to the biopsy revealed the same lesion and numerous other thoracic and cervical spine lesions that were contained within the vertebral body; there were no symptoms associated with the other lesions, and there was no evidence of spinal cord compression. Additionally, multiple renal lesions measuring up to 3 cm in size were noted. Histology of the biopsy was similar to that shown in Fig. 2.
Conservative treatment with bracing and epidural injections for the lumbar stenosis was initiated.
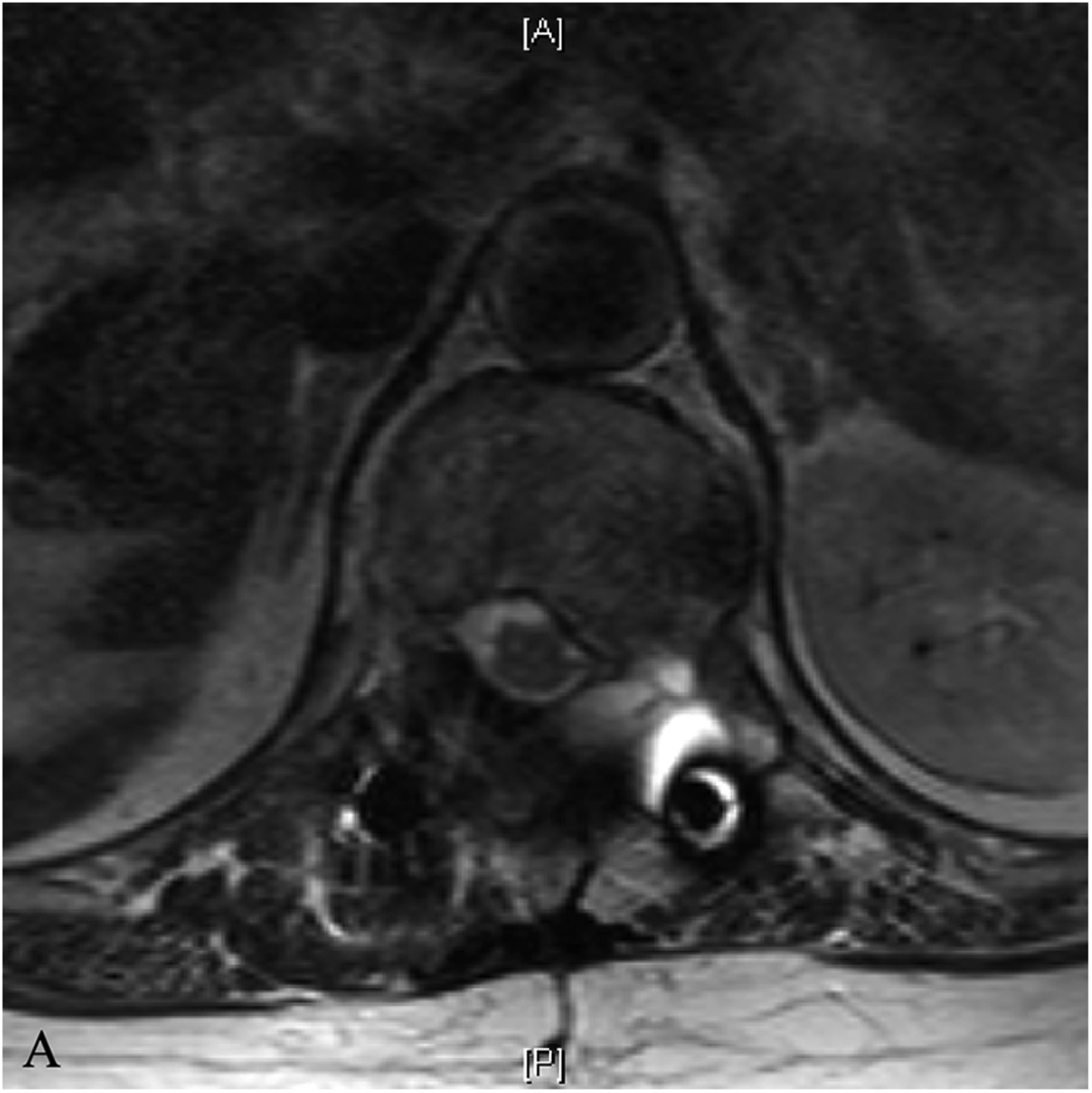
The hip and leg pain resolved with conservative treatment but the chest pain persisted, and the patient returned 2 years later. New MRI (Figs. 3-A and 3-B) revealed that the T12 lesion had grown and there was worsening cord compression. One year later, she returned after a biopsy at an outside hospital.
Although there was radiographic evidence of cord compression, the symptoms consisted of pain originating in the midthoracic spine that radiated across the left abdomen below the umbilicus, which was consistent with T12 radiculopathy. On examination, the patient did not have any focal motor deficits or signs of myelopathy, and she denied any urinary or bowel incontinence.
The original biopsy showed multiple cavernous blood vessels lined by a single layer of endothelial cells. There was no significant nuclear pleomorphism of the cells. The combination of radiograph and histologic findings are typical of a benign cystic angioma (CA), also known as a hemangioma. The patient was diagnosed with benign hemangioma (CA). We postulate that there were no clinical signs of cord compression because CA is a nonsolid lesion. Because of the unremitting thoracic pain, she underwent surgical resection of the lesion.
The patient underwent arterial embolization of the lesion 24 hours prior to surgery. A midline incision was performed to expose the posterior elements from T9 to L2. Pedicle screws were placed bilaterally at T9, T10, T11, L1, and L2. A single pedicle screw was placed on the right side at T12. A temporary rod was placed on the right side.
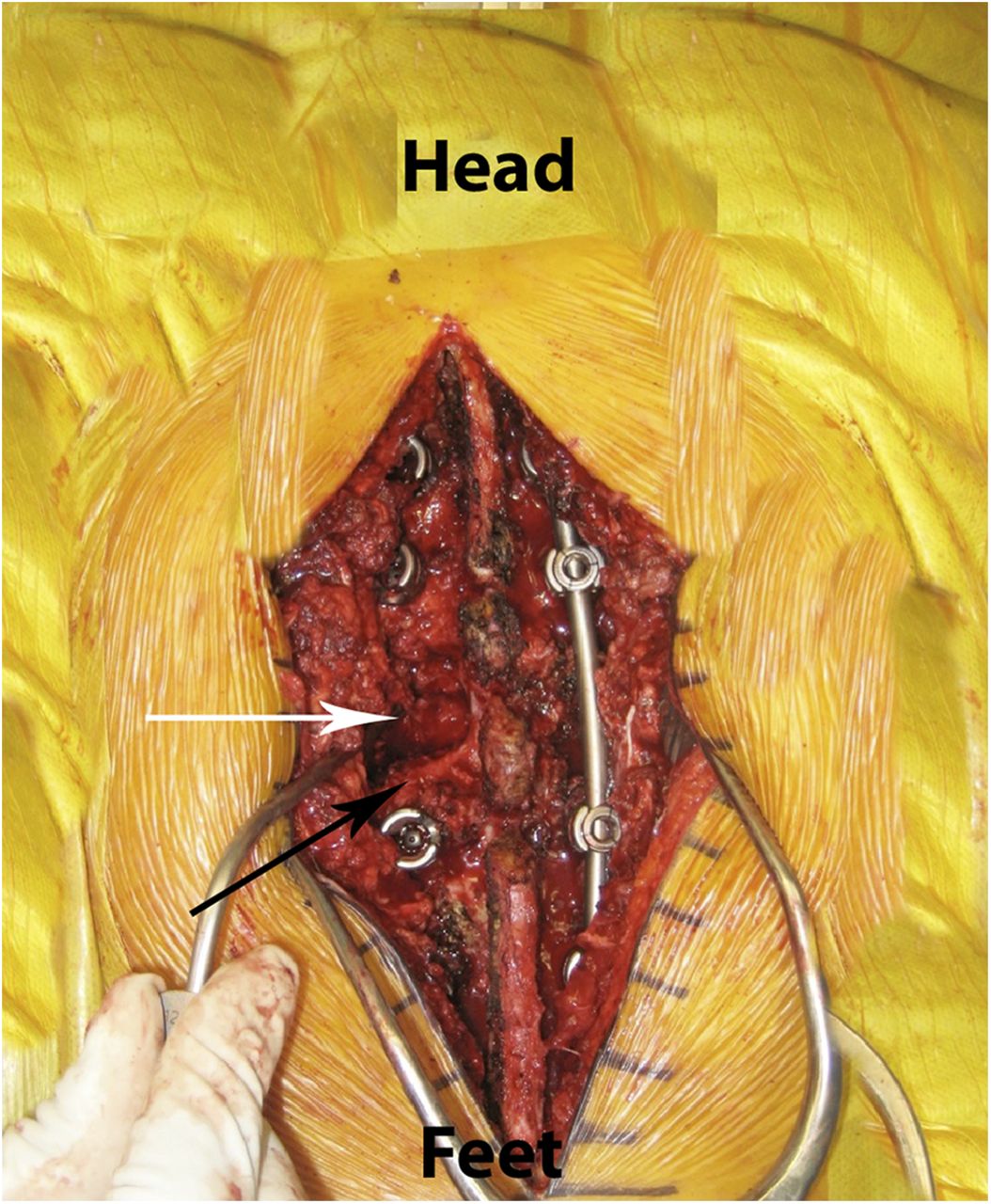
An intralesional resection was completed via a costotransversectomy approach. The spinous process of T12 was removed down to the lamina. A burr was used to perform a left hemilaminectomy. The T12 pedicle was identified, and a portion of the twelfth rib and its transverse process were removed. The T12 pedicle was entered with a high-speed burr down to the vertebral body, and a hemicorpectomy was performed. Removal of the lesion (Fig. 4) was accomplished with a high-speed diamond burr. The medial wall of the pedicle was then removed with a thin rongeur.
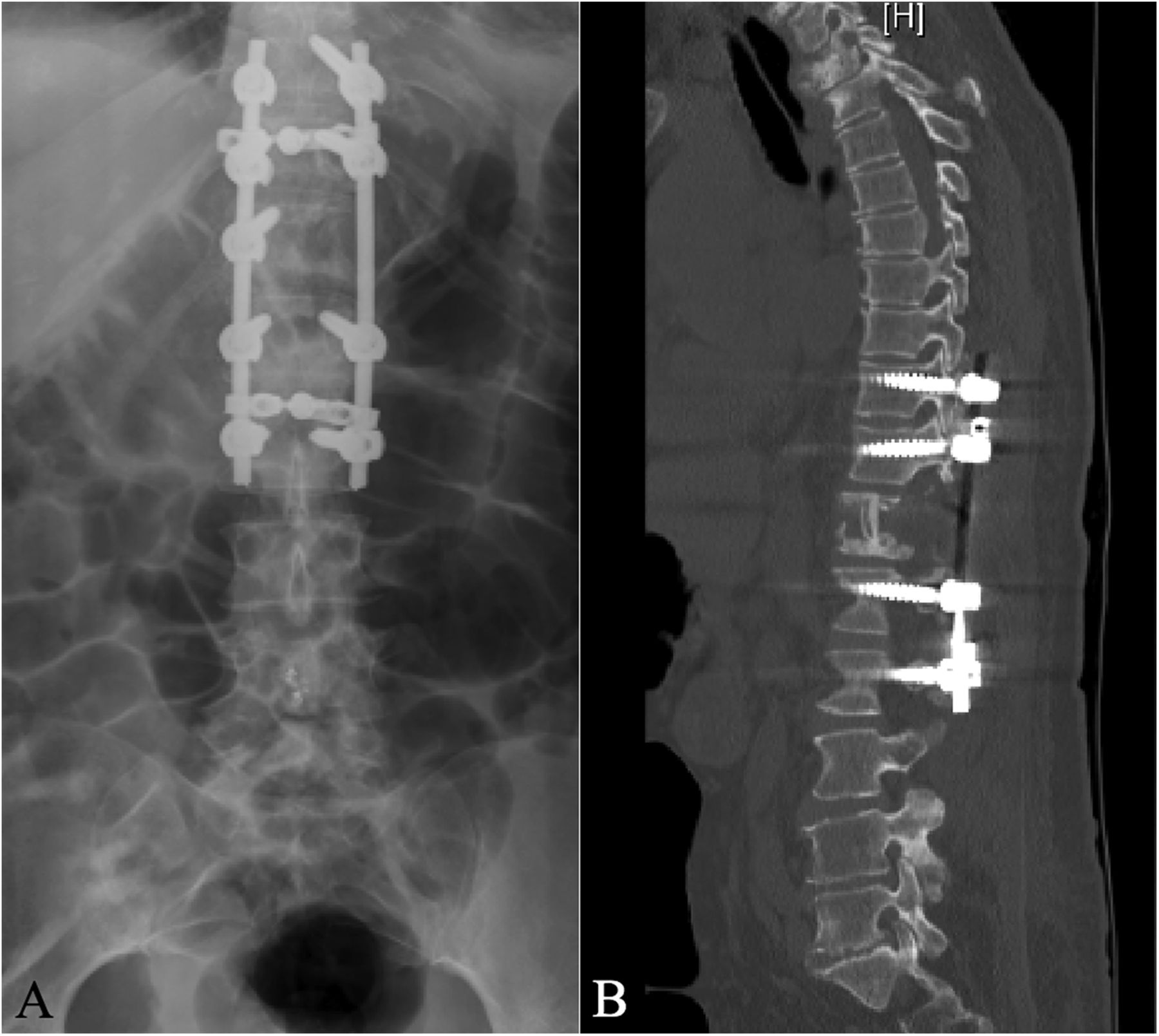
A portion of the resected rib was placed into the corpectomy defect. Rods were then placed, and decortication of the posterior elements was performed. A deep drain was placed and the wound was closed in a standard fashion. Postoperative testing revealed no neurofocal deficits; postoperative imaging demonstrated the surgical results (Figs. 5-A and 5-B).
At the 1-year postsurgical follow-up, the patient was completely asymptomatic. MRI (Figs. 6-A and 6-B) demonstrated near complete resolution of the lesion with appropriate consolidation of the rib graft. The other lesions had remained stable and asymptomatic.
Proceed to Discussion >>Reference: DePalma AAR, Shenoy K, Sharan AD. Cystic angiomatosis: a rare cause of thoracic radiculopathy: a case report. JBJS Case Connect. 2014 Jul 09;4(3):e55.
CA has been reported previously, but an extensive literature search revealed no cases of thoracic radiculopathy as the presenting symptom. The most common symptoms of CA are pathologic fracture and swelling due to skeletal and/or visceral involvement; however, many cases are discovered incidentally on chest radiograph. When the spine is affected, most reported cases of CA affect the lumbar spine; to the best of our knowledge, only 3 cases mention thoracic involvement. CA was first reported in 1953 by Jacobs and Kimmelstiel and is believed to originate from persistent lymphatic channels during early intrauterine development. The various clinical and histopathological presentations pose a terminological and diagnostic dilemma. Multiple similar terms have been applied to what is ultimately the same condition—CA.
Historically, diagnosing CA has been achieved most successfully by combining radiographic with histologic findings. Initial attempts at diagnosis depended upon simple radiographic findings showing multifocal lytic lesions, which may or may not be expansile, with cortical bone thinning with a sclerotic rim and no periosteal reaction. MRI and CT have provided superior imaging modalities that are helpful in differentiating the lytic lesions of CA from other radiographically similar lesions such as those of Langerhans cell histiocytosis and metastases. MRI has been found to produce hyperintense signals on T2-weighted images and hypointense signals on T1-weighted images with contrast enhancement, which depends on the composition of the lesion. Wunderbaldinger et al. found that pure lymphatic lesions failed to enhance after contrast administration. Soler et al. found lesions of mixed composition to enhance minimally after contrast administration. Both groups also reported that CT imaging of lesions produces low central enhancement with well-defined margins.
Pathologic diagnosis is best achieved via excisional biopsy of an involved rib (if present) because it allows the entire lesion to be removed en bloc. Biopsies from other locations tend to be inconclusive as only part of the lesion is removed. The lesions are characterized by thin-walled vascular (blood, lymphatic, or both vessels) channels lined by endothelial cells without mitoses. Communicating cysts that drain blood or a proteinaceous fluid may also be seen.
The benign nature and possible spontaneous resolution of these lesions often makes treatment unnecessary. If symptoms become progressive or nonresponsive to conservative therapy, as in our patient, treatment options are limited. Local radiation and chemotherapy, once considered first-line therapy, have shown little effect. Radiation has even been known to induce sarcomatous change of the lesion. Lesion removal, if necessary, can be pursued. Complete removal of the lesion, as in our patient, shows the viability of surgical excision in the management of refractory and progressive disease. Although we were unable to find any literature on arterial embolization of CA lesions, there are numerous reports of other cystic bone lesions being managed with preoperative embolization prior to removal. We believe that preoperative embolization of the supplying arteries decreases intraoperative bleeding.
It is important to keep multiple diagnoses in mind when dealing with a patient with this constellation of findings. Langerhans cell histiocytosis, malignancy, polyostotic fibrous dysplasia, hyperparathyroidism, and Gorham disease (also known as “disappearing bone disease” or “massive osteolysis”) all have radiographic findings similar to CA. Gorham disease presents the most confusing diagnostic challenge. It not only resembles CA radiographically, but also histologically. However, it tends to involve a single bone and causes substantially more destruction.
Reference: DePalma AAR, Shenoy K, Sharan AD. Cystic angiomatosis: a rare cause of thoracic radiculopathy: a case report. JBJS Case Connect. 2014 Jul 09;4(3):e55.
What is the diagnosis?
Vascular ectasia associated with a compression fracture
Angiosarcoma
Benign hemangioma (cystic angioma)
Paget disease
Granulation tissue consistent with previous biopsy site

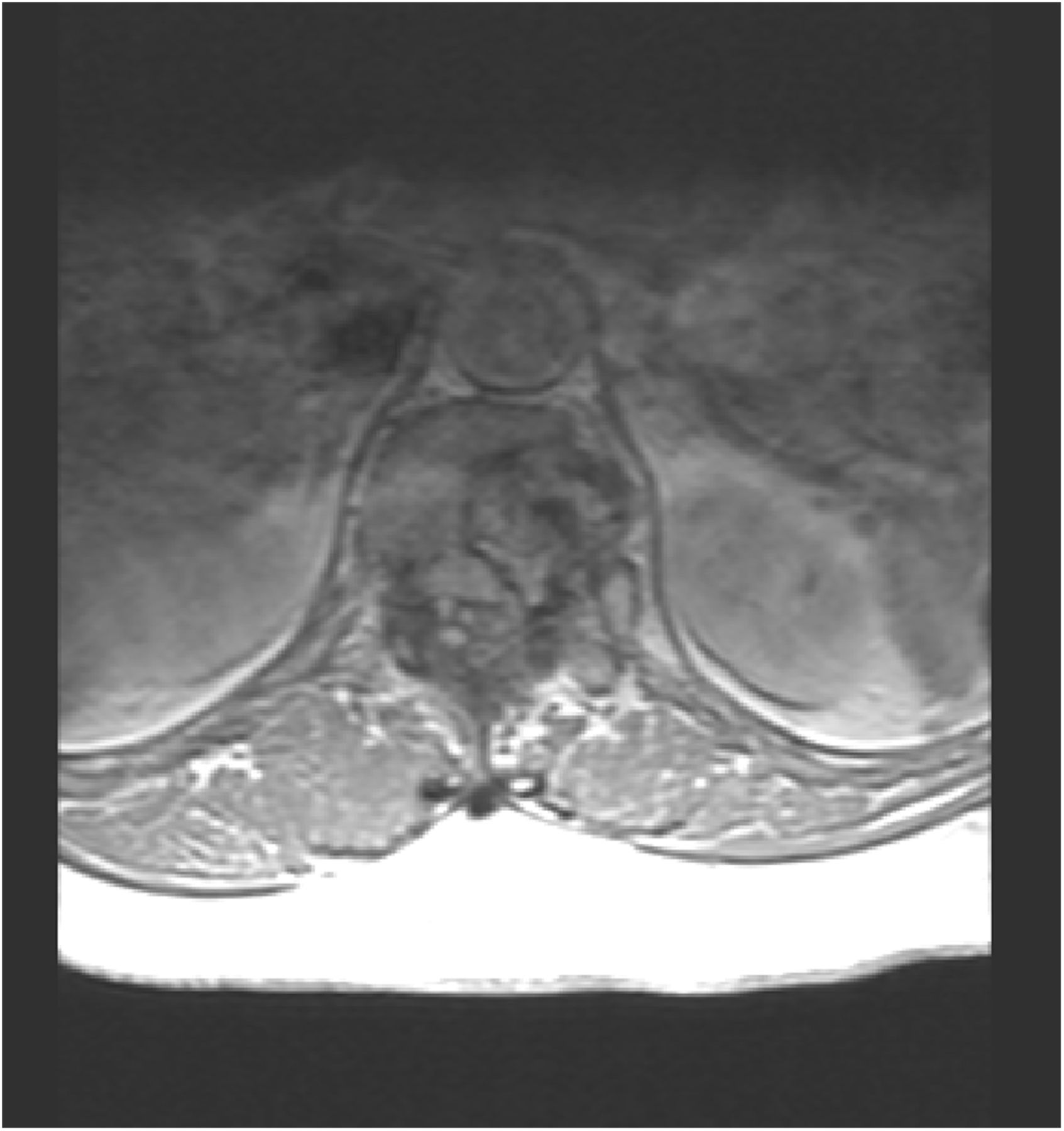
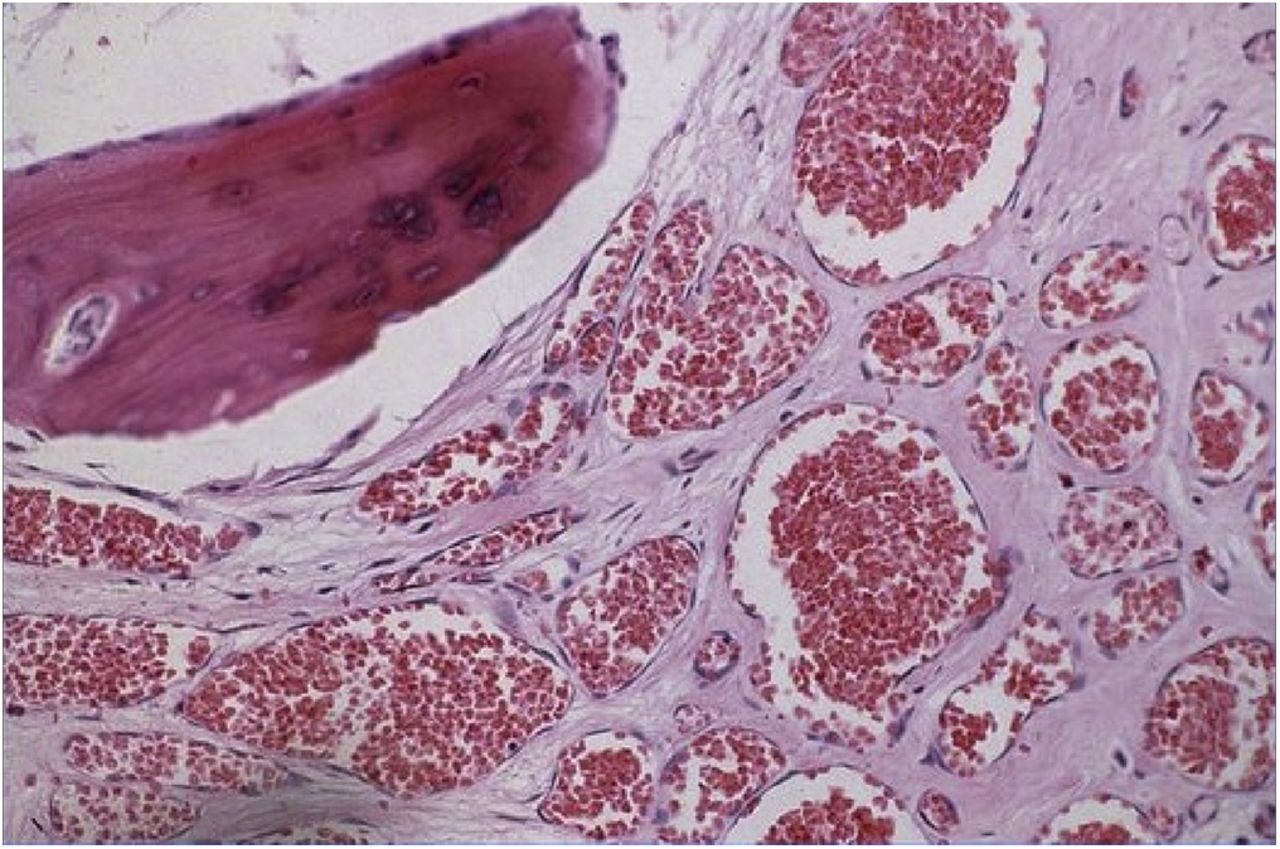
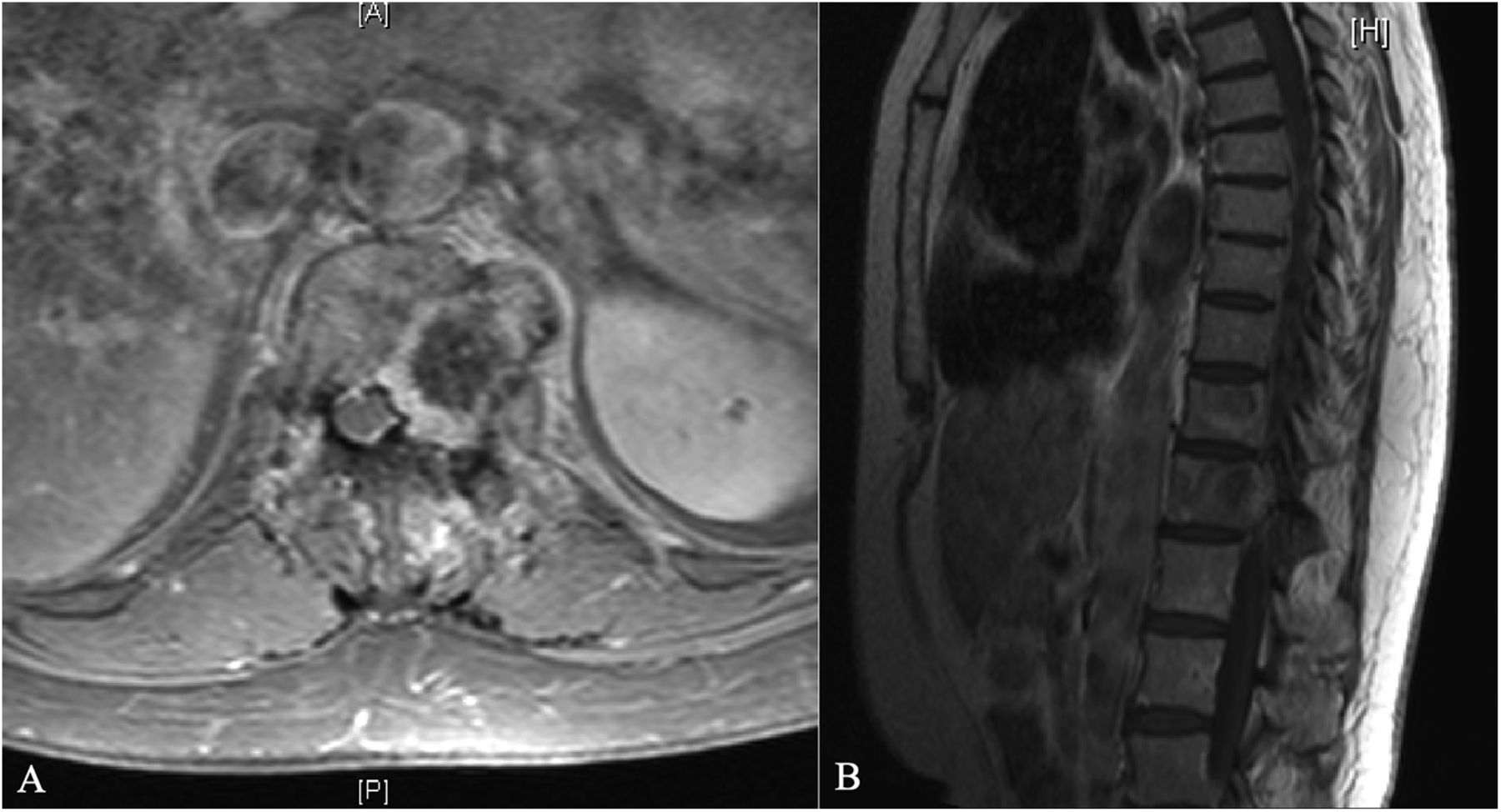
 Fig. 1
Fig. 1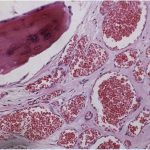 Fig. 2
Fig. 2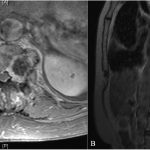 Fig. 3
Fig. 3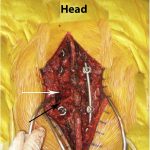 Fig. 4
Fig. 4 Fig. 5
Fig. 5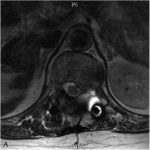 Fig. 6-A
Fig. 6-A Fig. 6-B
Fig. 6-B