A 66-year-old otherwise healthy man presented with symptoms of severe debilitating left knee pain in 2005. The radiographs (Fig. 1) and clinical examination revealed osteoarthritis, and the patient underwent a left total knee arthroplasty in 2006 (Fig. 2). Apparently, tissue from the arthroplasty was not submitted for pathologic evaluation. The patient progressed through the postoperative recovery with continued pain despite therapy, adequate range of motion, and intra-articular corticosteroid injections. Because of the persistent symptoms, an arthroscopic synovectomy was performed in early 2009. During this procedure, the surgeon did not identify any obvious neoplastic process, and tissue specimens were not sent for pathologic evaluation. The pain persisted, and the patient described a 50-lb (22.7 kg) unintentional weight loss.
In late 2009, the patient was referred to our institution. Symptoms included severe left knee pain and an enlarging mass. The left knee was diffusely swollen, and there was a palpable mass encompassing the suprapatellar region. He had a 50-degree fixed flexion contracture.
Radiographs were limited in quality secondary to the fixed flexed position of the knee, but revealed a poorly defined lucent lesion involving the lateral femoral condyle. The total knee arthroplasty implants appeared well fixed. The suprapatellar pouch and the remainder of the intra-articular space were filled with a radiodense mass (Figs. 3 and 4).
A Tru-Cut needle biopsy was performed through the incision of the previous arthroplasty. Histology from a subsequent specimen is shown in Figures 5 and 6.
An above-the-knee amputation was performed. The specimen demonstrated a 15 × 15 × 4-cm mass that appeared to have originated in the distal part of the femur and extended through the cortex and into the periprosthetic soft tissues and joint space. Final pathology diagnosed a grade-2 (intermediate) conventional chondrosarcoma with myxoid features.
The early postoperative course was uncomplicated, but within a year, surveillance imaging revealed progressive pulmonary lesions. In 2010, the patient died as a result of widely metastatic disease.
Proceed to Discussion >>Reference: Morehouse HA, Wilson DJ, Cannon CP, Manoso MW. Conventional chondrosarcoma diagnosed after total knee arthroplasty: a case report. JBJS Case Connect. 2015 Nov 25;5(4):e104.
This case report highlights the importance of diagnostic vigilance. The diagnosis of intermediate-grade chondrosarcoma in this patient was achieved only after 3 years of failed operative and nonoperative treatment. No biopsy was obtained during this time period despite the presence of an enlarging periprosthetic mass, and apparently no tissue had been submitted to pathology at the time of primary arthroplasty or arthroscopic synovectomy more than 3 years later.
The diagnosis of chondrosarcoma often requires correlation among clinical, imaging, and histologic features, and histologic grading is necessary to determine optimal management. Most orthopaedic surgeons rely on radiographic studies to consider the differential diagnosis of cartilage tumors. Radiographic differentiation between low-grade chondrosarcomas and benign cartilage tumors is difficult and sometimes impossible, although cartilage tumors, in general, are described as having mixed lytic and sclerotic areas within the intramedullary space, often expressed as a “ring-and-arc” pattern caused by production of chondroid matrix and calcification. Because conventional radiographic findings are not reliably accurate for diagnosis and staging of these tumors, computed tomography (CT) and magnetic resonance imaging (MRI) are also recommended. CT is more sensitive for detecting matrix mineralization and can delineate both the intraosseous and extraosseous components of chondrosarcoma. MRI can be particularly useful for demonstrating features that help distinguish a chondrosarcoma from a benign chondroid lesion. Certain nuclear medicine scans, most notably bone scintigraphy, have historically been useful in diagnosing skeletal metastases. However, in a study by Douis and Saifuddin, evidence showed no change in surgical management with or without the use of bone scintigraphy.
The diagnostic challenge is increased in the postarthroplasty setting where swelling and pain are common. The use of arthroscopy has been established as an effective method of treatment for various intra-articular pathologies. However, complications have been reported when it is used without advanced preoperative imaging on patients with intra-articular malignancies, including seeding of biopsy sites and delayed diagnosis. The true etiology of joint pain symptoms can be obscured by radiographic findings of degenerative joint disease in elderly patients. Our patient had intra-articular involvement by chondrosarcoma, causing initial concern that he had synovial chondromatosis undergoing malignant transformation to synovial chondrosarcoma, which is a rare but well-documented event (1% to 5% of patients). However, review of the imaging studies and the resection specimen suggest that the chondrosarcoma most likely started in the distal part of the femur and secondarily involved soft tissue and the joint space.
The established treatment for malignant cartilage lesions is wide surgical resection. The lesion in our patient was very large (15 × 15 × 4 cm) with intra-articular extension; therefore, limb-preserving wide resection with negative margins was not feasible. In general, low and intermediate-grade chondrosarcomas are relatively resistant to radiotherapy and chemotherapy.
This case is unique because our patient had a prior total knee arthroplasty 3 years before the diagnosis of chondrosarcoma in the same knee. Total knee arthroplasty is an invasive procedure and therefore carries the risk of multiple complications, including thromboembolic events and infection; however, chondrosarcoma is not considered one of the usual complications. Neither Tharani et al. nor Brewer et al. were able to establish a causal link between malignancy and total hip or knee arthroplasty. In a case report by Alexander et al., a man with radiographic evidence of osteoarthritis actually had an intra-articular myxoid chondrosarcoma. It is possible that our patient’s intra-articular space was seeded with tumor during the total knee arthroplasty, but there was no clear evidence of radiographic changes characteristic of chondrosarcoma before the initial surgery. However, because the quality of the radiographs obtained prior to the initial surgery was poor, it was unclear if there was a preexisting tumor. Our patient had undergone an arthroscopic debridement for persistent pain, stiffness, and swelling 3 years following the total knee arthroplasty. No advanced imaging modalities were employed prior to this surgical intervention. No neoplastic process was suspected at the time of the total knee arthroplasty or subsequent arthroscopic synovectomy, but as far as we know, no tissue from either procedure was submitted for pathologic evaluation. Based on the available information, it is unknown exactly when or where this tumor initially arose. However, because of the patient’s protracted course of postoperative knee pain and the findings in the resection specimen, it seems likely that the tumor arose in the distal part of the femur and was followed by direct extension from the femoral condyles into the joint space or it seeded the joint space after the total knee arthroplasty.
The risk of seeding a joint during total knee arthroplasty or arthroscopic synovectomy is not well known, but this case raises the suspicion that seeding can occur. It also highlights the importance of considering a wide differential diagnosis and having a high index of suspicion. In our patient, early advanced imaging studies followed by a biopsy of abnormal proliferative tissue may have made a substantial impact with early detection and treatment of this aggressive malignant lesion. If a metaphyseal chondroid lesion is observed, care should be taken to avoid seeding the joint during procedures such as total knee arthroplasty; if unexpected findings are encountered during arthroplasty, interpretation of a frozen section may help clarify a diagnosis.
Reference: Morehouse HA, Wilson DJ, Cannon CP, Manoso MW. Conventional chondrosarcoma diagnosed after total knee arthroplasty: a case report. JBJS Case Connect. 2015 Nov 25;5(4):e104.
What is the diagnosis?
Chondrosarcoma
Synovial chondromatosis
Synovial sarcoma
De-differentiated parosteal osteosarcoma
Adverse local tissue reaction

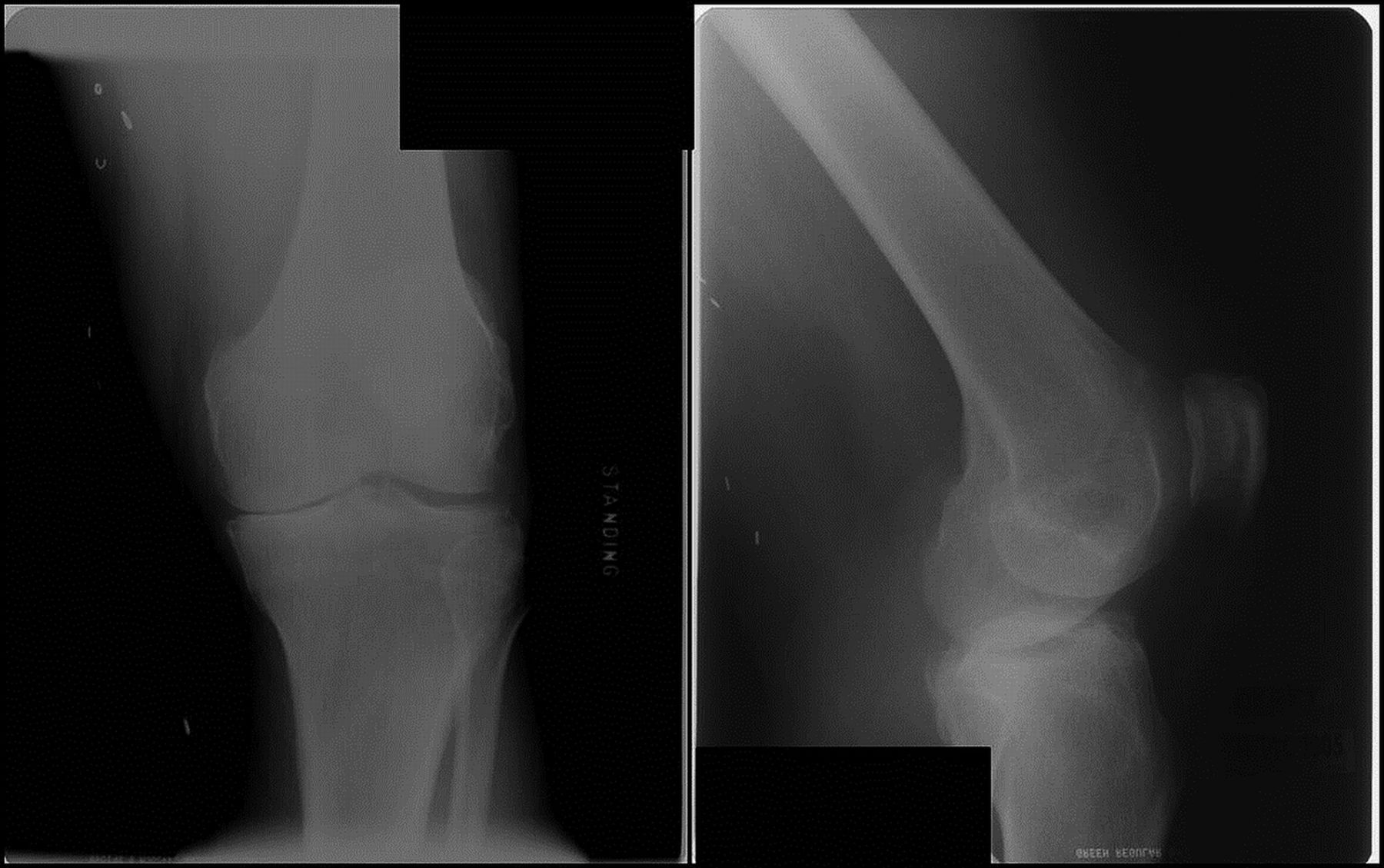

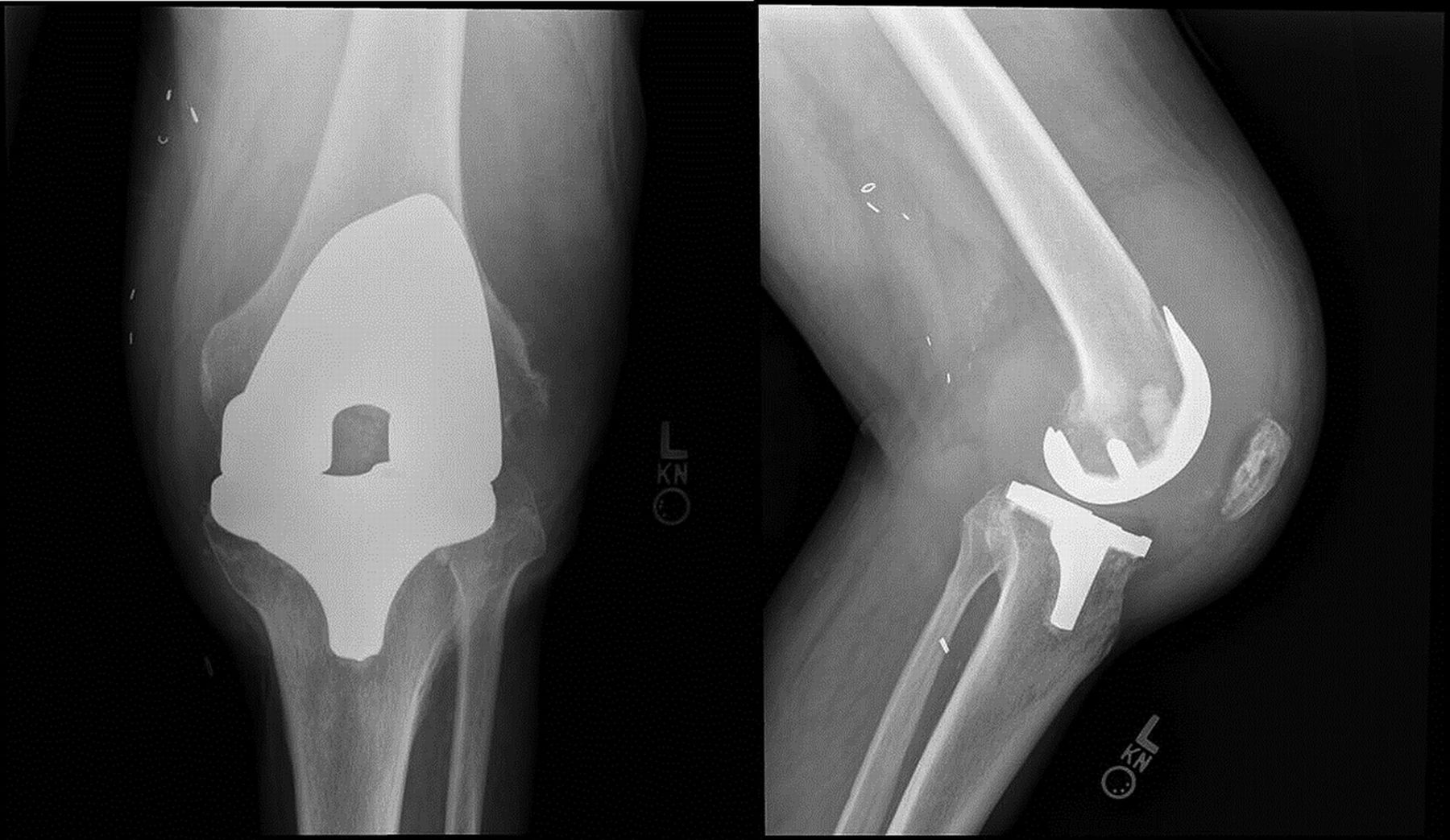

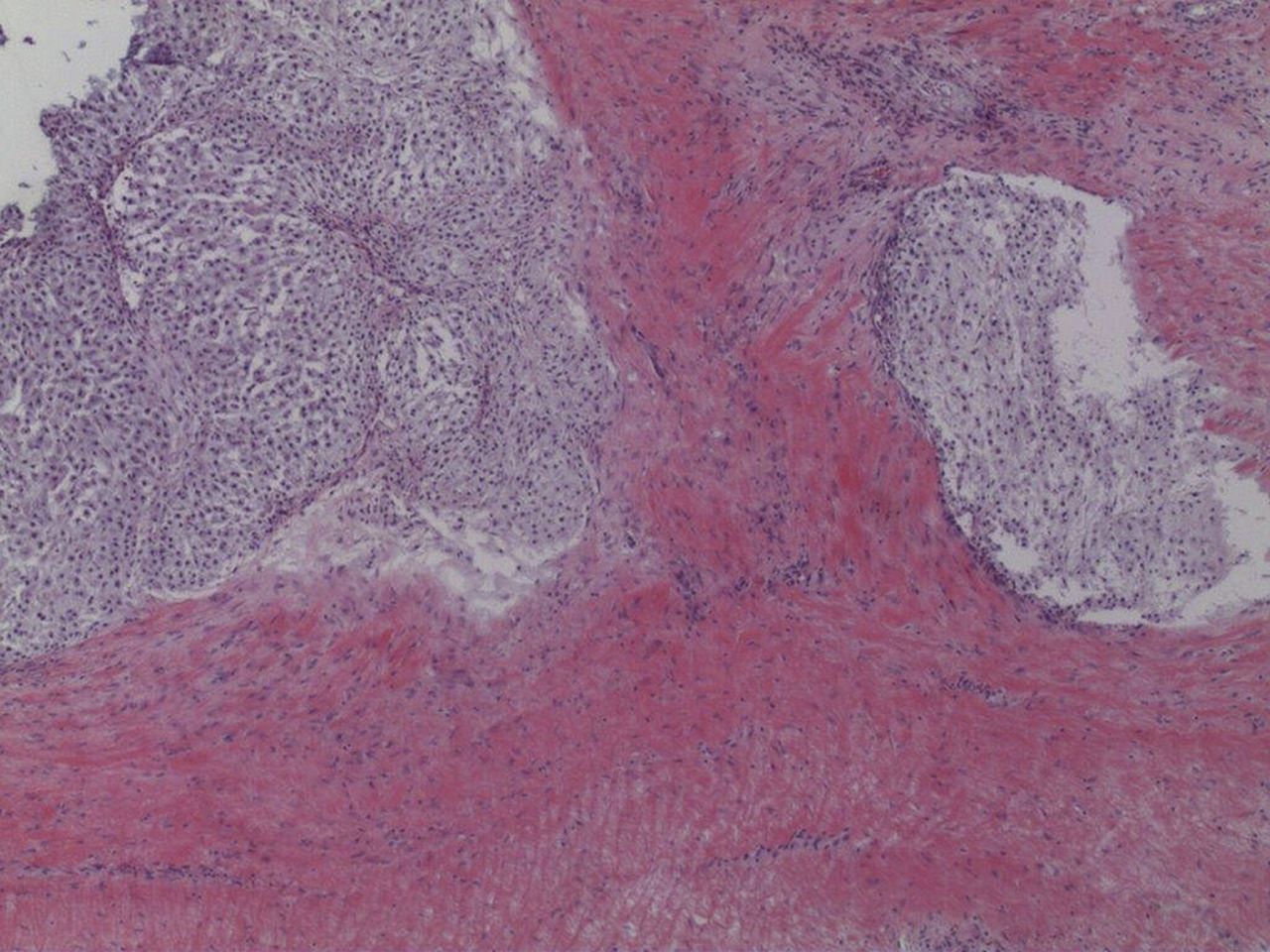
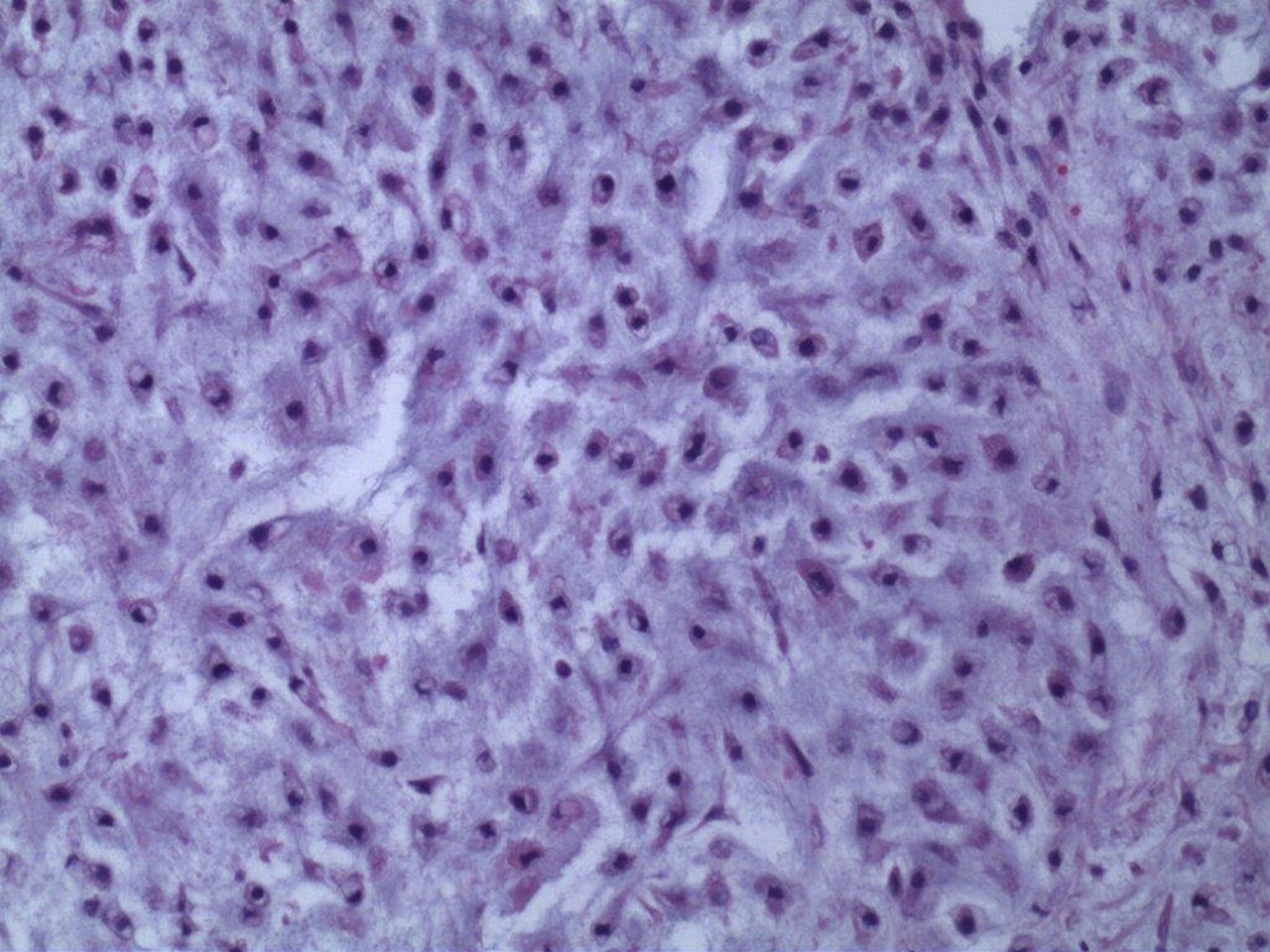
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4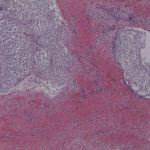 Fig. 5
Fig. 5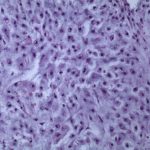 Fig. 6
Fig. 6