A Forty-six-Year-Old Man with Increasing Left Chest Pain
December 16, 2015
A forty-six-year-old man presented with a seven-week history of left chest pain. The pain was localized to the left sternoclavicular joint (SCJ) and was described as a dull ache that had been increasing in intensity. The patient reported having sustained a penetrating injury to the area eight weeks previously when running a polishing machine at work. He stated that a piece of metal was thrown from the machine and produced a skin laceration about 1 cm in length and 2 cm in depth. Immediately after injury, he went to a township public health center for a simple wound cleansing and dressing. When he presented to us at eight weeks, he had no fever but the left SCJ was slightly swollen and tender. Motion of the left shoulder was painful. The ESR (erythrocyte sedimentation rate) was normal and the WBC (white blood-cell) count was 6.7 × 109/L, but the high-sensitivity CRP (C-reactive protein) level was elevated to 11.8 mg/L. CT (computed tomography) scans demonstrated swelling, with areas of decreased density in the left clavicle and the adjacent sternum (Fig. 1). The patient was otherwise healthy and specifically reported that he had no history of diabetes or excessive alcohol consumption.
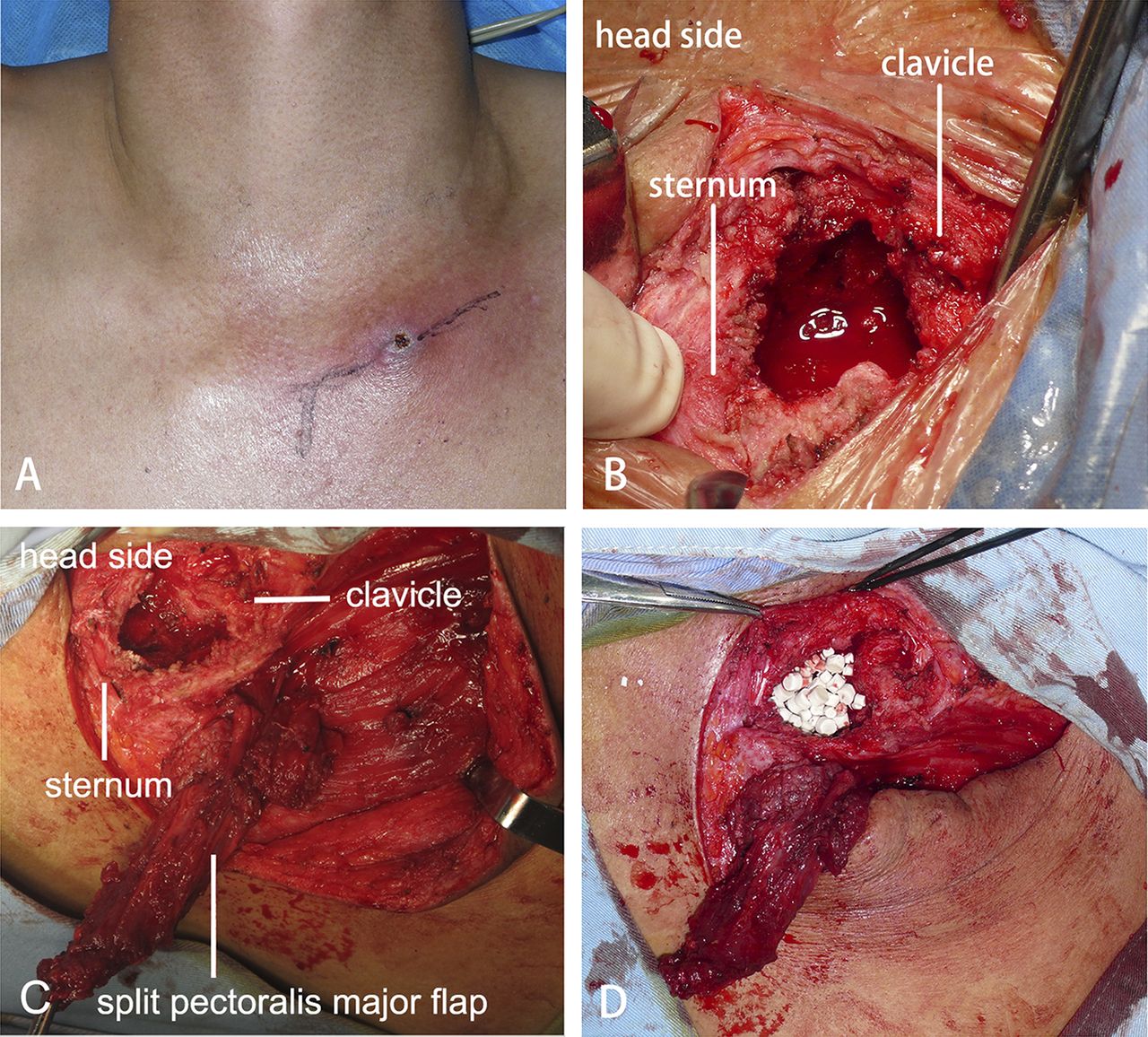
The SCJ was aspirated and bacterial cultures confirmed a Staphylococcus aureus (S. aureus) infection. Testing demonstrated methicillin, vancomycin, and levofloxacin sensitivity. Surgical debridement of the septic left SCJ was undertaken. The patient was placed in the supine position under general anesthesia. The exposure was made via a curved incision starting over the medial aspect of the clavicle and extending over the manubrium sterni. The muscle attachments to the medial aspect of the clavicle were removed, and the medial one-sixth of the clavicle was resected. After resection of the clavicular head and the intra-articular disc, a defect in the inferior aspect of the capsule was found, and an abscess extending to the retrosternal space was identified and drained. After thorough irrigation and debridement, the residual defect measured approximately 3.5 cm in width and 3 cm in depth. The superior aspect of the pectoralis major was exposed after debridement. A portion of the muscle originating from the lateral edge of the manubrium sterni was dissected from the pectoralis major. This detachment created a split pectoralis major flap, measured approximately 4 cm in width and 10 cm in length, which could be easily rotated to fill the defect superiorly. A portion of this flap was then sutured to the lateral, cancellous surface of the sternum at the base of the debridement cavity. The remaining dead space was filled with a surgical-grade calcium sulfate bone graft substitute (OSTEOSET; Wright Medical Technology) loaded with vancomycin. According to the manufacturer’s protocol, 1 g of vancomycin was added to 5 mL of calcium sulfate to produce the vancomycin-loaded calcium sulfate, which was shown in one recent study to be effective in treating tibial and calcaneal osteomyelitis. After the calcium sulfate was implanted, the rest of the pectoralis major muscle fibers were sewn superiorly to the platysma fascia and medially to the sternal periosteum (Fig. 2). A single closed suction drain was placed deep to the flap. Bacterial cultures confirmed an S. aureus infection. The patient received 0.2 g levofloxacin, to which the organism was sensitive, twice a day intravenously for two weeks after surgery. The suction drain was removed at two weeks, as three sets of bacterial cultures of the drainage were negative. The patient was discharged on postoperative day fifteen without additional antibiotics. The postoperative course was uneventful. At a one-year follow-up, the patient had full range of motion and excellent strength in his left upper extremity without any pain or tenderness in the region of the surgery (Fig. 3). MRI (magnetic resonance imaging) showed that all of the calcium sulfate placed in the left SCJ defect had been degraded, and there were no signs of recurrent infection (Fig. 4). The patient was informed that data concerning the case would be submitted for publication and provided consent.
Proceed to Discussion >>Reference: Huang K, Zhang C. Sternoclavicular joint infection treated with debridement, vancomycin-loaded calcium sulfate, and partial pectoralis muscle flap: A case report. JBJS Case Connect. 2015 Oct 14;5(4):e86.
SCJ infections are rare but, when present, often result in abscess formation. Because the joint capsule is unable to distend, the infection can spread quickly beyond the joint. Surgical treatment of this joint can be technically demanding because of its proximity to major vascular structures and a lack of substantial overlying soft tissues. Burkhart et al. proposed that asymptomatic SCJ infections could be treated conservatively with intravenous antibiotics but that symptomatic SCJ infections often required surgical intervention, especially when the patient presented with an abscess, osteomyelitis, or mediastinitis. Surgical resection combined with muscle transposition provided effective long-term outcomes. In staphylococcal infection of the SCJ, it has been recommended that intravenous antibiotic therapy be continued for six weeks followed by subsequent oral antibiotic therapy because inadequate treatment can lead to serious complications, such as empyema, mediastinitis, and chest wall abscess. However, antibiotic toxicity and the development of bacterial resistance are common problems associated with such prolonged antibiotic therapy. In a recent study, we used a local delivery system to treat traumatic osteomyelitis and found that the resulting concentration of antibiotics locally exceeded the effective therapeutic concentration as well as the minimum inhibitory concentration, whereas the blood concentration was low. These findings indicated that the local delivery system could be effective for the treatment of osteomyelitis, with fewer side effects compared with prolonged intravenous antibiotic administration. As a biocompatible and biodegradable material, calcium sulfate is an ideal carrier for the local delivery of antibiotics in bone and joint infections. It has also been recognized for its clinical performance as an osteoconductive matrix for bone repair. We therefore selected calcium sulfate as the carrier in our patient. Combining the calcium sulfate carrier with the split pectoralis major flap provided some specific advantages. The split pectoralis major muscle flap is well vascularized from the intact perforating vessels along the sternum. The flap provided good coverage of the dead space filled with the calcium sulfate granules. Our method of pectoralis major flap coverage differs from that previously described by Zehr et al. Those authors described a rotational pectoralis major flap in one case of SCJ osteomyelitis and used nearly half of the pectoralis major muscle for the reconstruction. Sacrificing this much of the muscle could result in a substantial decrease in the strength of humeral flexion, a disadvantage noted by those authors. In our case, the degradable calcium sulfate rather than the pectoralis major was used to fill the defect, and only a limited part of this muscle was transferred to cover the calcium sulfate. In this case, the combined technique had almost no influence on humeral flexion strength because most of the pectoralis major remained intact. In summary, we believe that surgical debridement followed by a split pectoralis major muscle flap transfer combined with implantation of antibiotic-loaded calcium sulfate represents an excellent option for the treatment of chronic SCJ infection. Further studies that include a greater number of cases are required to prove its effectiveness.
Reference: Huang K, Zhang C. Sternoclavicular joint infection treated with debridement, vancomycin-loaded calcium sulfate, and partial pectoralis muscle flap: A case report. JBJS Case Connect. 2015 Oct 14;5(4):e86.
Sternoclavicular joint dislocation
Inflammatory arthritis
Intra-articular medial clavicle fracture
Sternoclavicular joint bacterial infection
Pigmented villonodular synovitis of the sternoclavicular joint


 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4