A Thirty-two-Year-Old Man with Neck Pain Following Extension Injury
August 19, 2015
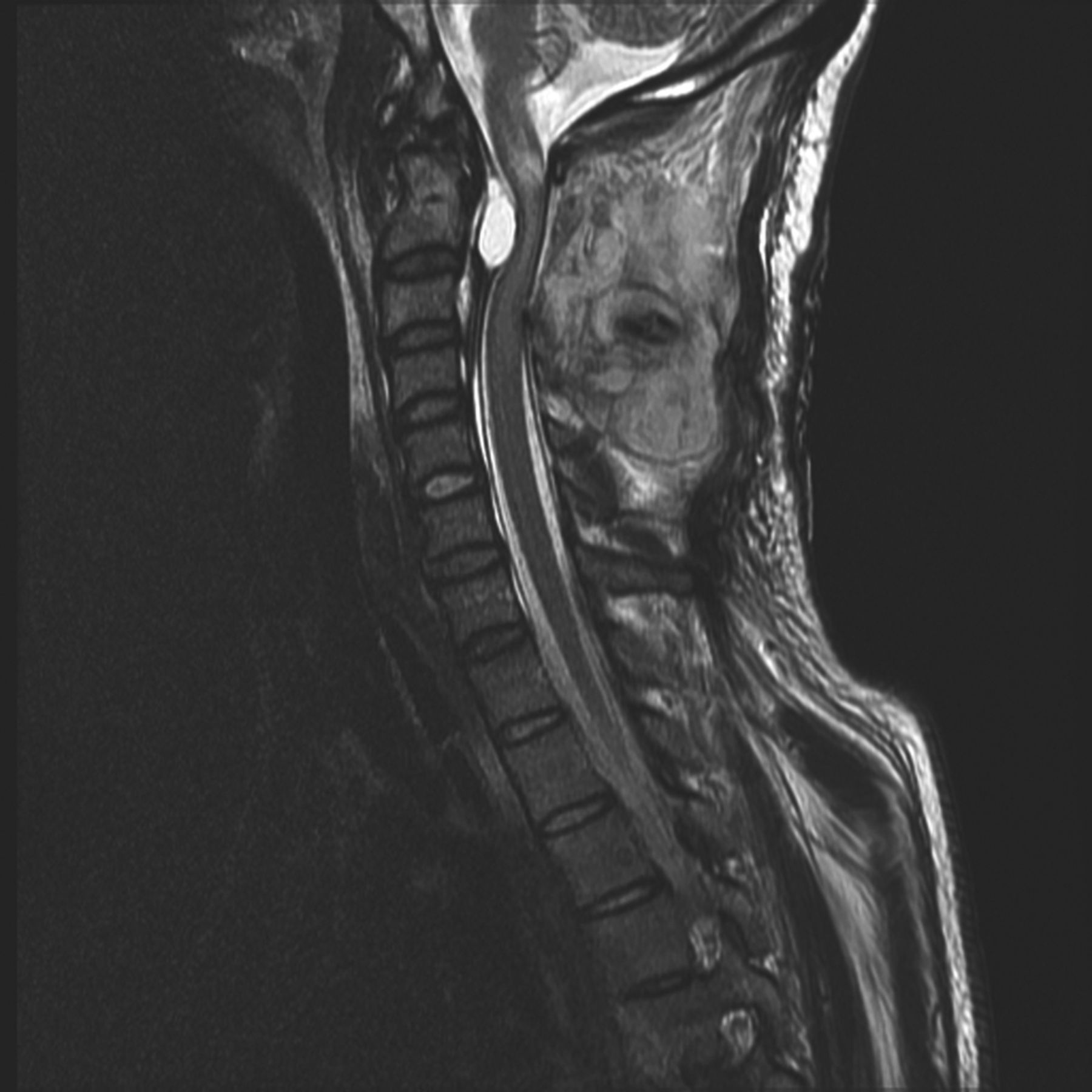
A thirty-two-year-old man was brought to the emergency department after a hyperflexion-extension injury of the neck on a roller coaster. The patient felt a pop in the neck, had involuntary loss of control of the bowel and bladder, and had onset of immediate tetraparesis. He had no previous neck pain or neurological symptoms. The patient was brought to a Level-I Trauma Center where a standard corticosteroid protocol with methylprednisolone was started within ninety minutes of the injury. The initial computed tomography (CT) scan and radiographs demonstrated an os odontoideum at the C2 level, but there were no other fractures, dislocations, or signs of cervical spine instability (Fig. 1). Examination with the American Spinal Injury Association (ASIA) protocol showed a motor strength of 4 of 5 in all muscle groups on the right side and a motor strength of 2 of 5 on the left side. Decreased anal sphincter tone was also demonstrated. The initial sensory examination showed intact light touch sensation on the right side, with impaired light touch sensation caudal to the T7 level. Pinprick sensation was impaired caudal to the C6 level on the right but was preserved on the left. A magnetic resonance imaging (MRI) study identified a 7 mm × 20 mm elliptical fluid collection in the epidural space with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images (Fig. 2). This fluid collection caused severe spinal stenosis with subsequent adjacent central edema within the spinal cord.
The fluid collection was initially interpreted as an acute epidural hematoma. In light of the clinical and radiographic findings, the patient went to the operating room for an emergency posterior decompression and fusion. The patient underwent an uncomplicated C2-C3 decompression with a laminectomy of C2 and the superior portion of C3, with C1-C3 instrumented posterior fusion, with use of a combination of lateral mass and pedicle screws. No hematoma was encountered anteriorly despite the wide C2 laminectomy and direct visualization along the medial border of the C2 pedicles bilaterally. On postoperative day two, a repeat MRI revealed a persistent fluid collection, with imaging characteristics similar to the initial MRI examination. The lesion was stable to slightly larger in size, with continued signal change within the adjacent spinal cord (Fig. 3). It was determined that the lesion most likely represented a cystic lesion, not an acute epidural hematoma. Because this cystic lesion continued to cause spinal cord compression and displacement, the patient was returned to the operating theater on postoperative day three to decompress the lesion via needle aspiration. The transoral surgical approach was considered. However, because of the large size of the lesion and recognizing that the lateral border of the mass was adjacent to the medial wall of the C2 pedicle, a repeat attempt was made at decompressing it with a posterior surgical approach. An 18-gauge spinal needle was used to create a small slit in the lateral edge of the mass, which was difficult to differentiate from the dura. Approximately 10 cc of viscous, gelatinous fluid, clinically similar to ganglion or facet cyst fluid, was successfully evacuated. Pathologic review confirmed highly viscous myxoid material with low cellularity, consistent with synovial fluid. The patient was determined to have a synovial cyst. The next day, the patient underwent repeat MRI examination, which confirmed interval decompression of the anterior cyst with improvement of the compression of the cervical cord (Fig. 4). At the one-year follow-up, the patient continued to show neurological improvement with a motor strength of 5 of 5 in muscles enervated by C5-C7 on the right side, and a motor strength of 5– of 5 in muscles enervated by C8 and T1 on the right side. On the left side, he demonstrated a motor strength of 5 of 5 in muscles enervated by C5-C6, 5– of 5 in C7 muscles, and 4+ of 5 in muscles enervated by C8 and T1. The lower-extremity motor function had improved to 5 of 5 in muscles enervated by L1-S1 bilaterally, but there was increased tone and spasticity. He was functioning independently, performing daily activities of living (including writing), and driving short distances. The gait remained slow and wide based, with a slight crouch, but he was able to walk without assistive devices. Radiographs showed good spinal alignment (Fig. 5).
Proceed to Discussion >>Reference: Schmitz MR, Jenné J. Acute tetraparesis caused by a cervical spine synovial cyst associated with an os odontoideum. A case report. JBJS Case Connect. 2012 Apr 25;2(2):e17.
The most common causes of anterior spinal compression at the C1-C2 level include meningioma, schwannoma, chordoma, and osteochondroma. Nontumor etiologies include rheumatoid arthritis pannus and hypertrophic healing of odontoid fractures. Synovial cysts of the spine are rare, most often presenting in the lumbar spine and mimicking the symptoms of a herniated nucleus pulposus. These cysts are most commonly found in patients in the fifth or sixth decades of life and present with either radicular or myelopathic findings. Cervical spine synovial cysts are especially rare, occurring usually at either the cervicothoracic junction or the C1-C2 junction. Os odontoideum is an anatomic anomaly of unclear etiology, thought to be developmental in nature, although there are case reports of acquired deformity after trauma in patients younger than three years old. The principal differential diagnosis of the os odontoideum is an ununited fracture of the dens. The rounded shape of the anterior arch of C1 is useful in distinguishing an os odontoideum fracture from a dens fracture. In an os odontoideum fracture, an abnormal articulation exists between the ossicle, which moves with C1, and the remaining portion of the dens, with a risk of atlantoaxial instability. To the best of our knowledge, only thirty-five cases of synovial cysts at the atlantoaxial junction have been identified. Only six of these cases were associated with an os odontoideum; all but one of these cases of atlantoaxial synovial cysts presented with a combination of myelopathy and/or radiculopathy. Weng et al. reported a catastrophic neurological event that occurred in an adolescent with a bipartite atlas and os odontoideum. To our knowledge, os odontoideum is rarely discussed in the literature in relation to MRI findings. In our case, a synovial cyst associated with an os odontoid led to a potentially catastrophic neurological injury in an otherwise healthy patient with no known pre-event symptoms. Understanding that our case report represents an extremely rare occurrence, it nonetheless affords the opportunity to be reminded of the potential pitfalls associated with an os odontoideum. Patients with an incidentally identified os odontoideum should undergo a thorough history, physical examination, and imaging examination, specifically looking for signs of underlying instability and subclinical myelopathy. The management of os odontoideum is controversial because there is a variable natural history course that ranges from stable over the course of many years to acute and catastrophic neurological injuries. The patient in our case report denied any preinjury signs or symptoms of myelopathy. There is currently insufficient evidence to support diagnostic and management standards and guidelines for the treatment of os odontoideum. Flexion-extension lateral cervical spine radiographs can be used for determining stability of the atlantoaxial joint. The anterior atlantodental interval (AADI) may not demonstrate abnormality if the os odontoideum translates with the anterior arch of C1. However, similar abnormal motion through the os odontoideum should warrant close follow-up or be considered an indication for surgery if the AADI is greater than 6 mm. In addition, the posterior atlantodental interval (PADI) could potentially be used as a reference for the space available for the cord. In patients with rheumatoid arthritis, Boden et al. showed that a PADI of less than 14 mm correlated with a substantial risk for neurological impairment. Additionally, in analyzing cases of os odontoideum, Spierings and Braakman reported that a minimal canal diameter of less than 13 mm was associated with a “10 to 1” risk of the patient developing permanent myelopathy. However, in their series, they found no association of the development of myelopathy with instability. A recent review by Arvin et al. suggests that surgical treatment should be offered to patients with “unstable os odontoideum or those with a fixed deformity causing compression of the upper cervical/medullary junction.” Synovial cysts of the cervical spine associated with an os odontoideum are extremely rare. To the best of our knowledge, we present the second known case of acute traumatic tetraparesis associated with a synovial cervical cyst and an os odontoideum after an innocuous traumatic insult. One should be fully aware of potential space-occupying lesions when reviewing MRI scans in the setting of trauma. Differentiating acute pathology from chronic pathology can be challenging.
Reference: Schmitz MR, Jenné J. Acute tetraparesis caused by a cervical spine synovial cyst associated with an os odontoideum. A case report. JBJS Case Connect. 2012 Apr 25;2(2):e17.
Retropharyngeal hematoma
Aneurysmal bone cyst involving the body of C2
Plasmacytoma of C2
Chordoma of C2
Synovial cyst


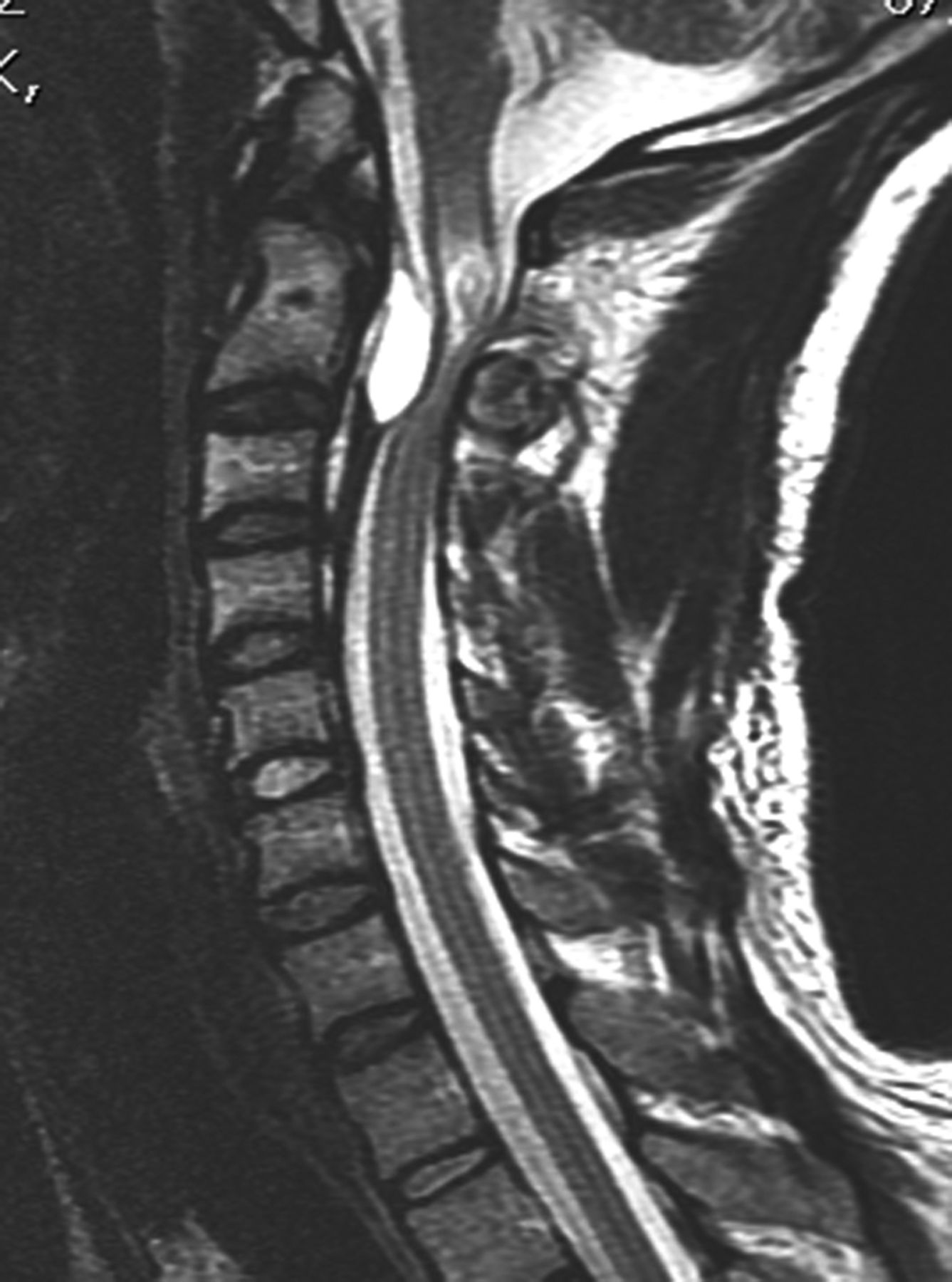
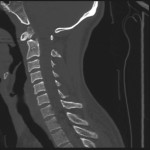 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5