An Eighteen-Year-Old Man with Ongoing, Worsening Groin Pain
July 15, 2015
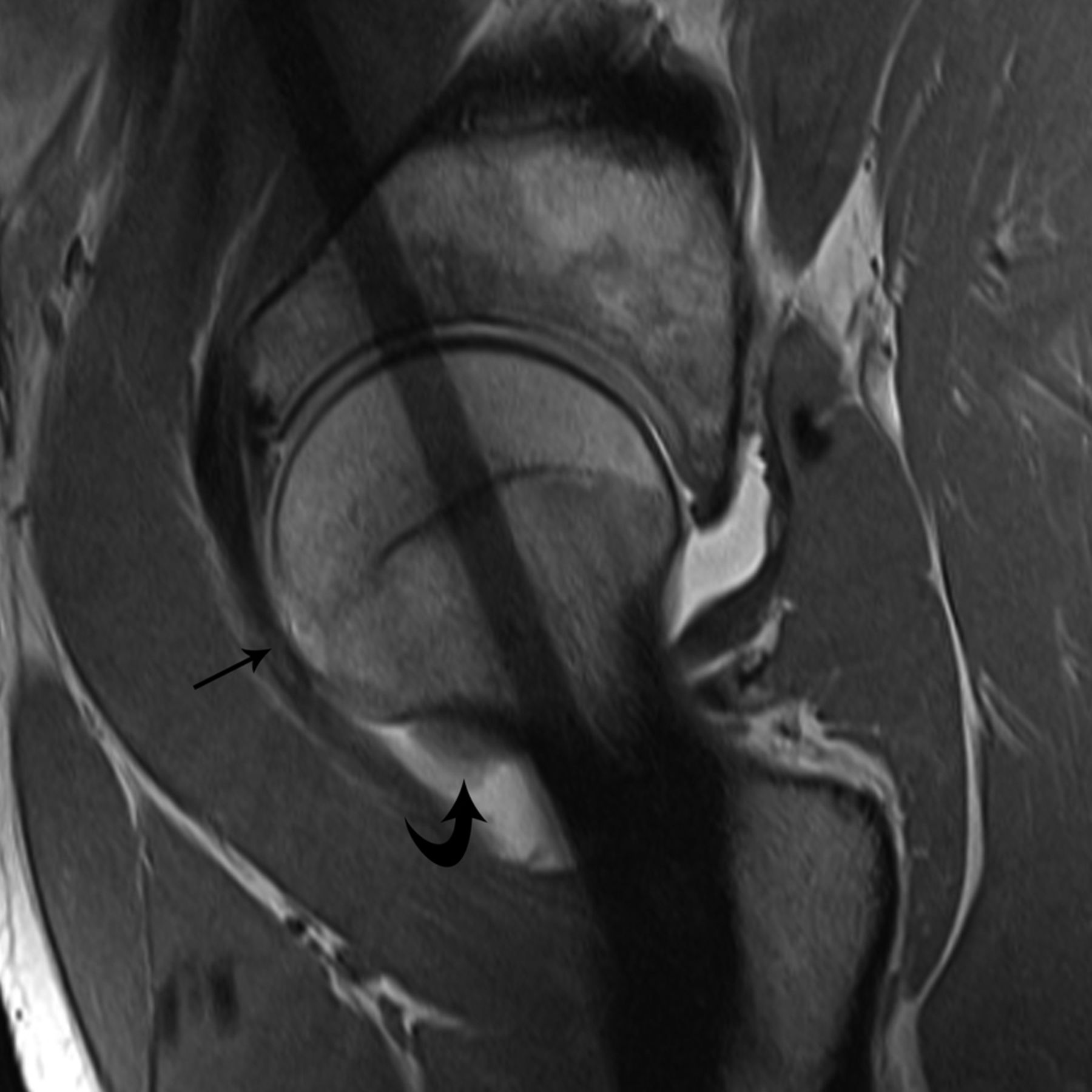
An eighteen-year-old patient presented with steadily worsening right groin pain over the course of a year. Symptoms increased when he participated in sports and, progressively, occurred at night. Most pain medications, including nonsteroidal anti-inflammatories, had little effect. Prior to referral to our clinic, the patient had a standard anteroposterior pelvic radiograph, a pelvic magnetic resonance image (MRI), and a magnetic resonance (MR) arthrogram, ostensibly demonstrating a decreased anterior femoral head-neck offset. Bone marrow edema in the femoral neck seen on the pelvic MRI was interpreted as reactive (Fig. 1). He was given the probable diagnosis of femoroacetabular impingement (FAI) and referred to our clinic for additional evaluation. On examination, the patient demonstrated a mild start-up limp that resolved quickly. Hip flexion, adduction, and internal rotation produced pain, as did palpation of the rectus femoris origin. Hip internal rotation was limited to 0° in 90° of flexion, as compared with 30° of internal rotation on the contralateral side. In all other planes, hip motion was symmetric to the left, with flexion to 90°, extension to 0°, and external rotation to 20°. A standard anteroposterior pelvic radiograph was normal except for patchy osteopenia around the right hip. A cross-table lateral radiograph demonstrated no major asphericity of the anterior femoral head. The previous MR arthrogram demonstrated massive osseous edema in the femoral neck, thickening of the joint capsule, and a substantial intra-articular effusion. Fibrous and chondral appositions surrounded the medial femoral neck at the chondral border, spreading superolaterally to the posterior femoral neck. A computed tomographic (CT) scan of the hip was obtained.
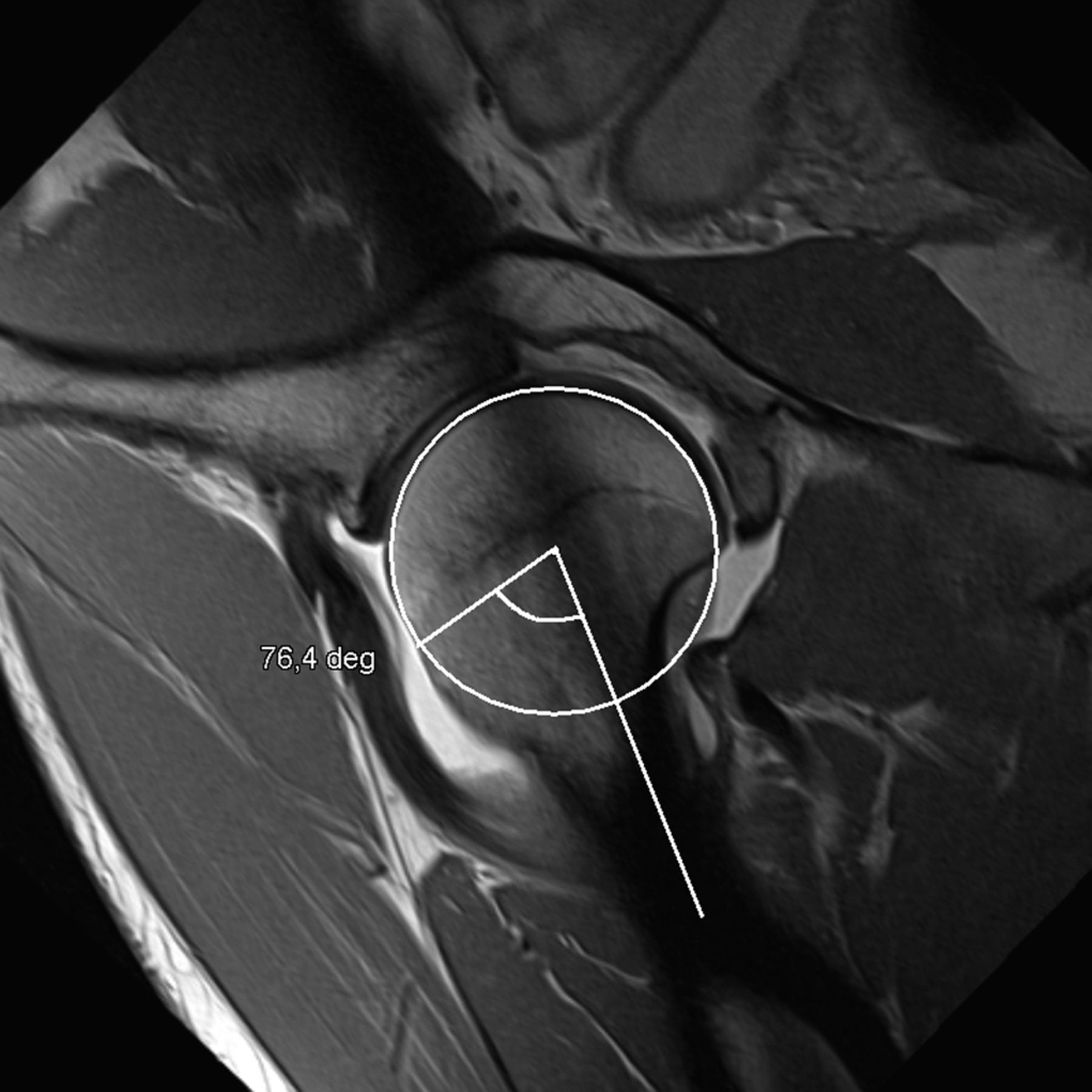
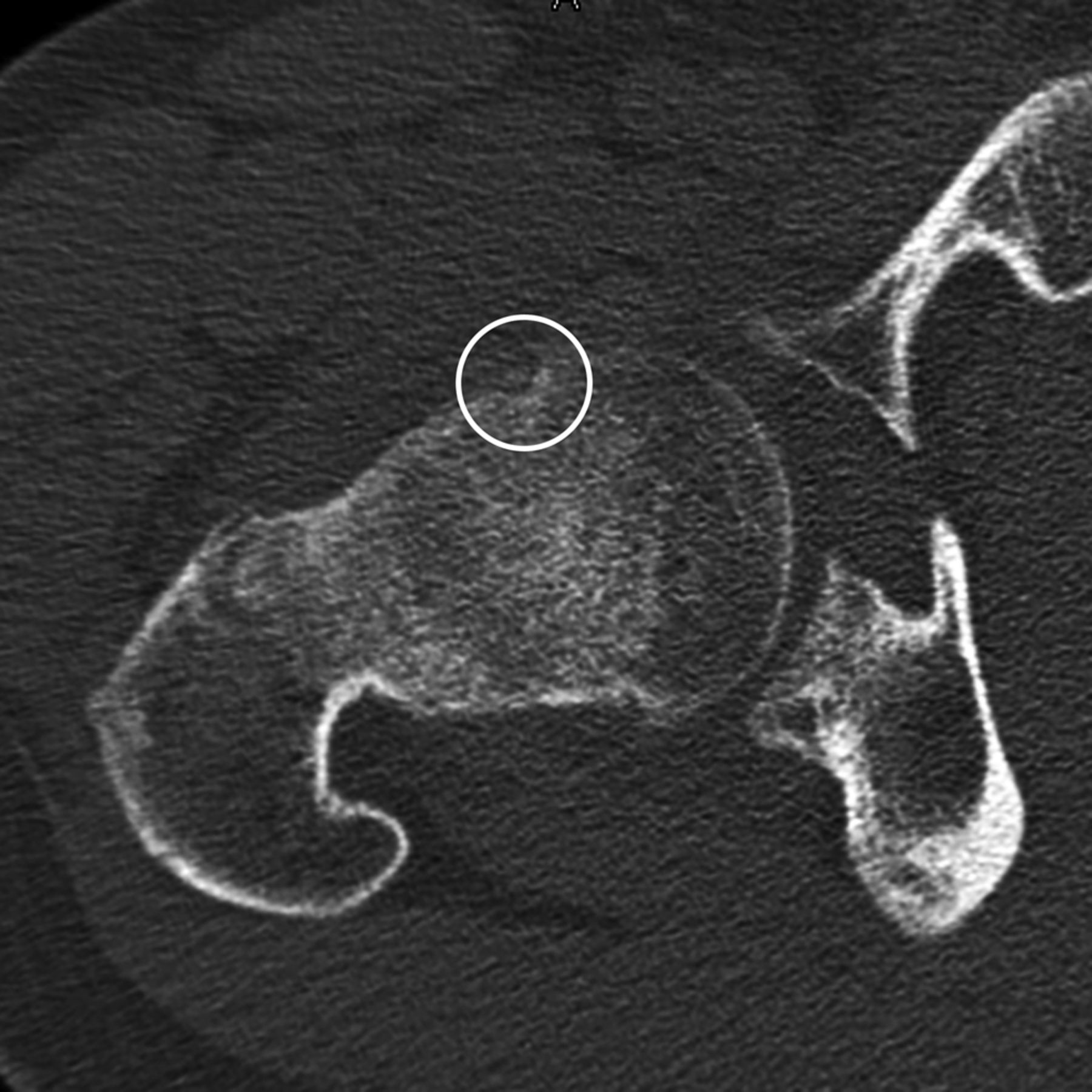
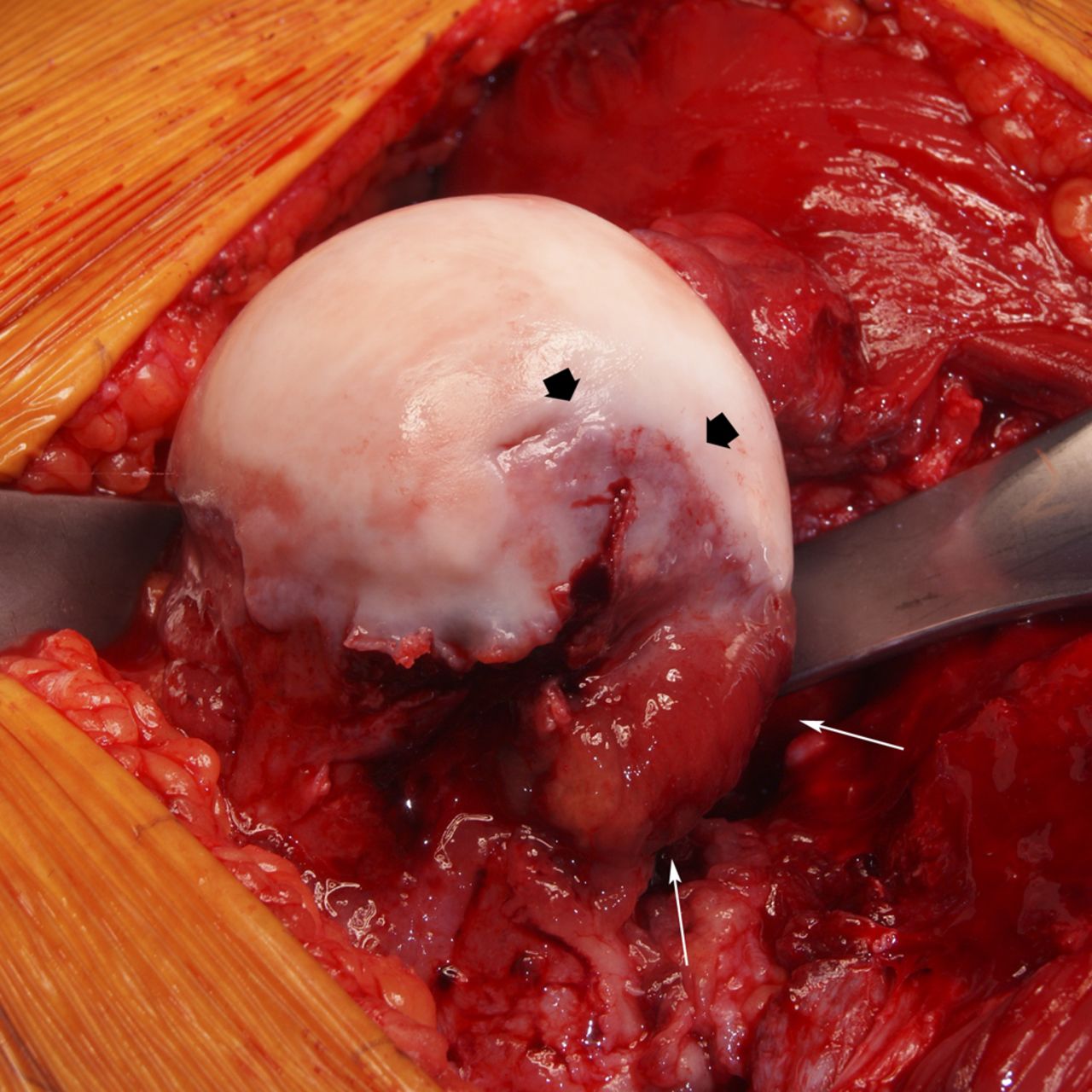
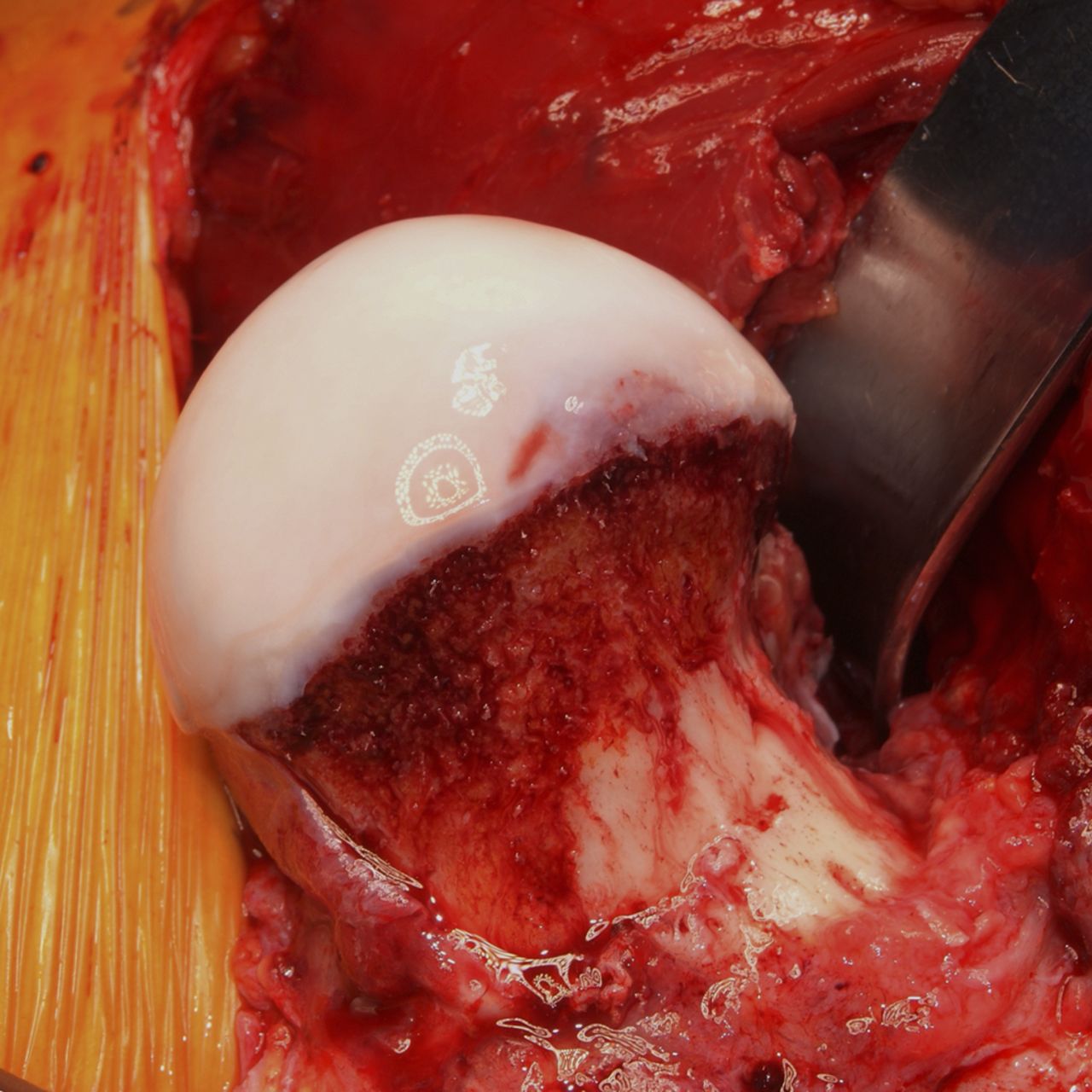
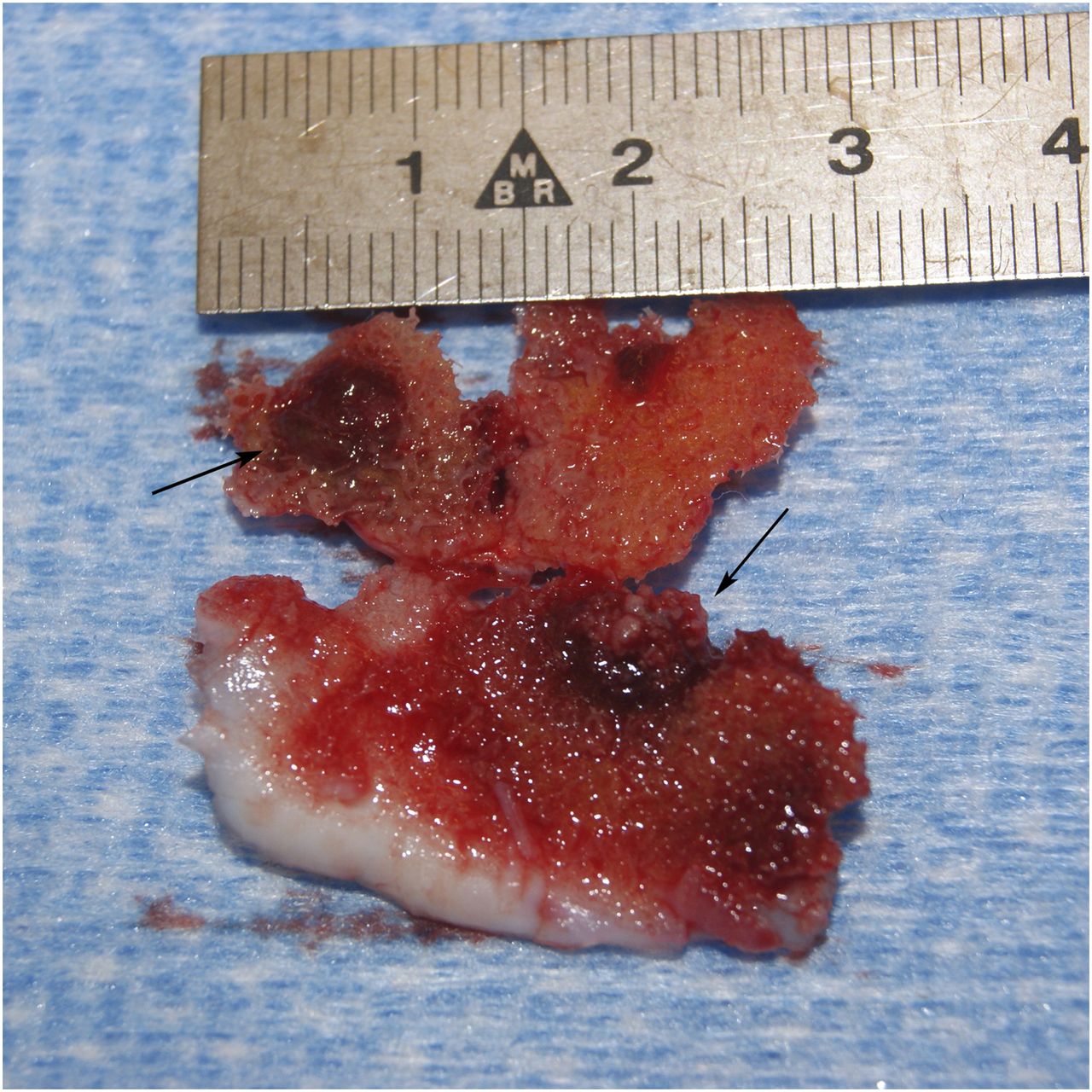
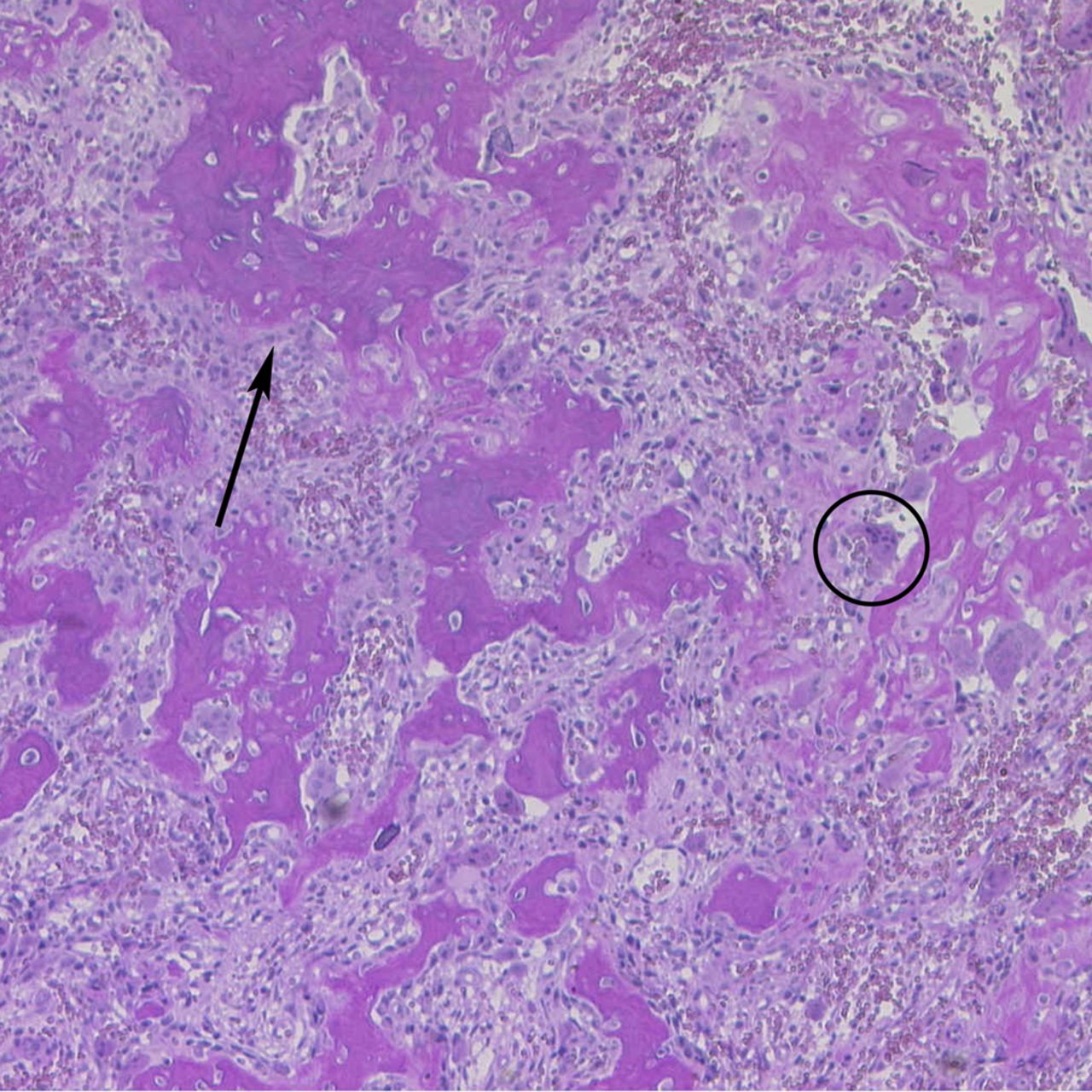
In the MR arthrogram, an anterior metaphyseal protrusion at the head-neck junction produced an increased alpha angle of 76°, which is substantially greater than the normal threshold of 55° (Figs. 2-A and 2-B). Fibrous and chondral appositions surrounded the medial femoral neck at the chondral border, spreading superolaterally to the posterior femoral neck. The combination of night pain, intense edema, and inflammatory reaction on the MR imaging was suspicious for an osteoid osteoma. The CT scan showed an intra-articular femoral neck osteoid osteoma with a nidus surrounded by mild sclerosis and fibrous tissue (Fig. 3). Clinically, a trial of aspirin substantially reduced the nocturnal pain. Given the nature and duration of the pain, the patient elected to proceed with surgical treatment. Because the reactive bone formation adjacent to the nidus had worsened a mild preexisting cam deformity and the impingement sign was positive on clinical examination, concomitant cam decompression was indicated. Arthroscopic management was briefly discussed; however, there was concern that the associated inflammatory tissue and reactive bone would impair visualization and access to both the nidus and the cam lesion. Thus, a surgical hip dislocation with a step-cut trochanteric osteotomy was performed. The joint capsule was markedly thickened, tense, and fibrotic, with adhesions and small capillary vessels in the surrounding soft tissue, consistent with chronic inflammation. On incision of the capsule, 20 mL of clear pressurized joint fluid was evacuated. The synovial membrane adjacent to the suspected osteoid osteoma was more than 10 mm thick and highly vascular. Similar changes in the synovial membrane were found cranial to the Weitbrecht ligament, at the perilabral fold of the capsule, in the acetabular fossa, and at the round ligament. Examination of the labrum revealed mild reddening without a visible or palpable tear, and the acetabular cartilage was intact. A large and uneven cortical prominence was present, beginning at the chondral border of the anterior femoral head in the area of the suspected nidus, spreading toward the distal third of the anterior femoral neck, and producing a reduced head-neck offset (Fig. 4-A). During the offset correction, a 5 × 5-mm area of brown-white tissue corresponding to the suspected nidus was excised (Fig. 5). After resection of chondral and fibrous appositions at the dorsal femoral neck, the femoral head-neck offset was restored, with complete sphericity of the femoral head (Fig. 4-B). Before closure of the capsule, impingement-free motion was verified under direct visualization. Postoperative treatment included partial weight-bearing (≤15 kg) for protection of the trochanteric osteotomy, and restriction of hip flexion to 90° for the first six weeks to minimize impingement. Daily continuous passive motion up to 90° of flexion was performed for one week postoperatively as part of our routine protocol to prevent adhesions. Histology performed on the nidus confirmed the diagnosis of an osteoid osteoma (Fig. 6), as described by Jaffe. Despite a mild immediate postoperative hematoma that caused initial pain, within one week of surgery the patient was nearly pain-free. At one month postoperatively, he had complete resolution of pain, with painless active and passive hip flexion to 90°, as well as 45° of internal and external rotation in 90° of flexion. Radiographs demonstrated healing of the trochanteric osteotomy, and full weight-bearing was allowed. Nine months postoperatively, after a physical therapy program of joint mobilization and abductor strengthening, the patient was completely symptom-free and able to play basketball without discomfort.
Proceed to Discussion >>Reference: Mainzer J, Ganz R, Tibor L, Leunig M. Not all hip pain is impingement: Femoral neck osteoid osteoma in a patient with a coexisting cam deformity: A case report. JBJS Case Connect. 2012 Jul 11;2(3):e31.
Up to 25% of osteoid osteomas are located on the proximal part of the femur, and 5% to 12% of all osteoid osteomas are intra-articular. Intra-articular osteoid osteomas remain a diagnostic challenge because of atypical symptoms and appearance on conventional radiographs. As a result, delays in diagnosis and treatment of intra-articular osteoid osteoma are common. In the hip, intra-articular osteoid osteomas are most commonly located at the medial or anteromedial femoral neck, as in our case. Aside from mild osteopenia, our patient had no obvious signs of intra-articular osteoid osteoma on the pelvic radiograph. The combination of the clinical picture with the intracapsular inflammation and intraosseous edema on the MRI was atypical for FAI and suspicious for osteoid osteoma. This prompted us to obtain a CT scan, which is the method of choice for identification of intra-articular osteoid osteoma. The nidus was visible on the CT scan, with mild surrounding sclerosis and bone apposition. Because anterior FAI is a frequent source of symptoms in the same area and intra-articular osteoid osteomas are often not visible on radiographs, misdiagnosis is possible. Although asymptomatic cam deformities are prevalent in the general population, as the awareness of FAI increases among orthopaedists, hip pain is increasingly attributed to FAI. In addition, on radiographs, a nidus might appear similar to a so-called impingement cyst, a fibrocystic lesion of the femoral neck frequently seen in hips with FAI. Nonetheless, the appearance of an osteoid osteoma on an MRI is quite different from that of FAI, with patients generally having some combination of synovitis (80%), bone marrow edema (60%), and juxta-articular soft-tissue edema (50%). As MRI protocols become more limited to those most likely to demonstrate labral tears or FAI findings, it is important to be mindful of less common diagnoses that may require additional MRI protocols for definitive diagnosis. These conditions include pigmented villonodular synovitis and synovial chondromatosis, as well as osteonecrosis, femoral neck stress fractures, and, less commonly, bone and soft-tissue sarcomas. The success rate of open surgery for osteoid osteomas ranges from 88% to 100%. Arthroscopy has also been used for the treatment of osteoid osteoma in the hip. In our case, the extensive synovitis as well as the substantial osseous and soft-tissue appositions extending from the anterior to the posterior head-neck junction prompted us to proceed with an open surgical approach. Although the cam deformity may have been asymptomatic before the development of the osteoid osteoma, the patient had a positive impingement sign and limited internal rotation compared with the contralateral hip. This was consistent with secondary impingement at the head-neck junction caused by the reactive bone and chondral tissue around the nidus. Open management also allowed better access and enabled complete resection of the cam deformity. It is not clear why up to 50% of the patients with intra-articular osteoid osteoma develop early osteoarthritis. Prostaglandin production and the extent of the subsequent intra-articular inflammation may be one causative factor. Conversely, in the hip, reactive osseous or chondral apposition, particularly at the femoral head-neck junction, can lead to a secondary FAI, resulting in mechanical damage to the cartilage and labrum. As awareness of FAI grows, it is tempting to diagnose impingement in young patients with symptoms around the hip. Asymptomatic cam and pincer morphology, however, is quite prevalent in the general population. Thus, the presence of FAI morphology does not necessarily mean that FAI is the primary cause of a painful hip. The correlation of history, clinical examination, and radiographic findings is important, and less common causes of hip pain should be considered.
Reference: Mainzer J, Ganz R, Tibor L, Leunig M. Not all hip pain is impingement: Femoral neck osteoid osteoma in a patient with a coexisting cam deformity: A case report. JBJS Case Connect. 2012 Jul 11;2(3):e31.
Cam deformity of the femoral neck
Anterior-superior labral tear
Lymphoma of bone
Osteoid osteoma
Hemangioma of femoral neck

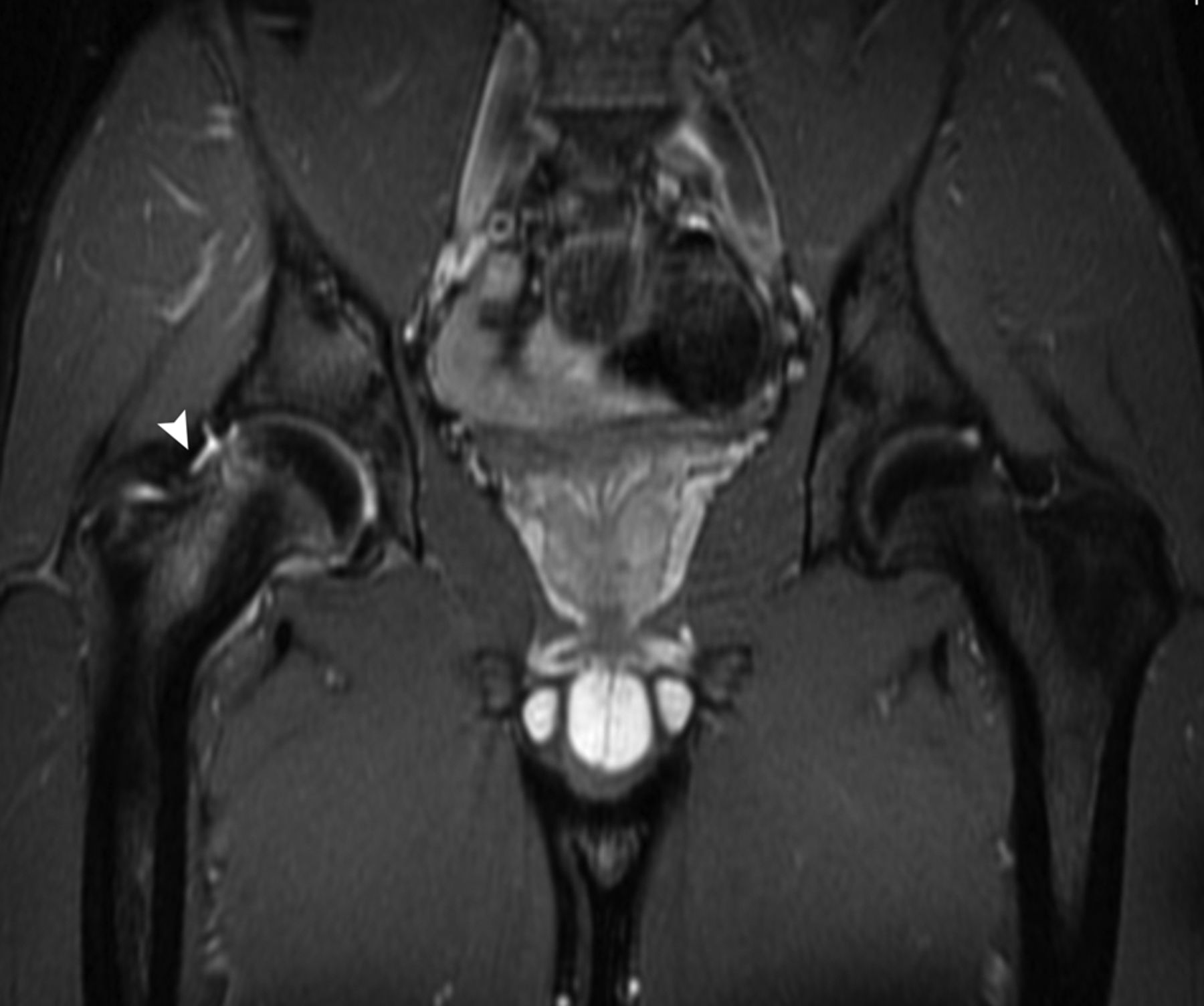
 Fig. 1
Fig. 1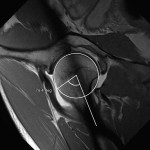 Fig. 2-A
Fig. 2-A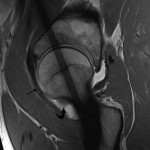 Fig. 2-B
Fig. 2-B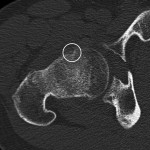 Fig. 3
Fig. 3 Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B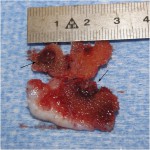 Fig. 5
Fig. 5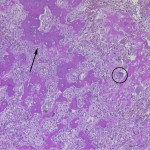 Fig. 6
Fig. 6