A Fifty-seven-Year-Old Woman with Sudden Forefoot Pain
May 20, 2015
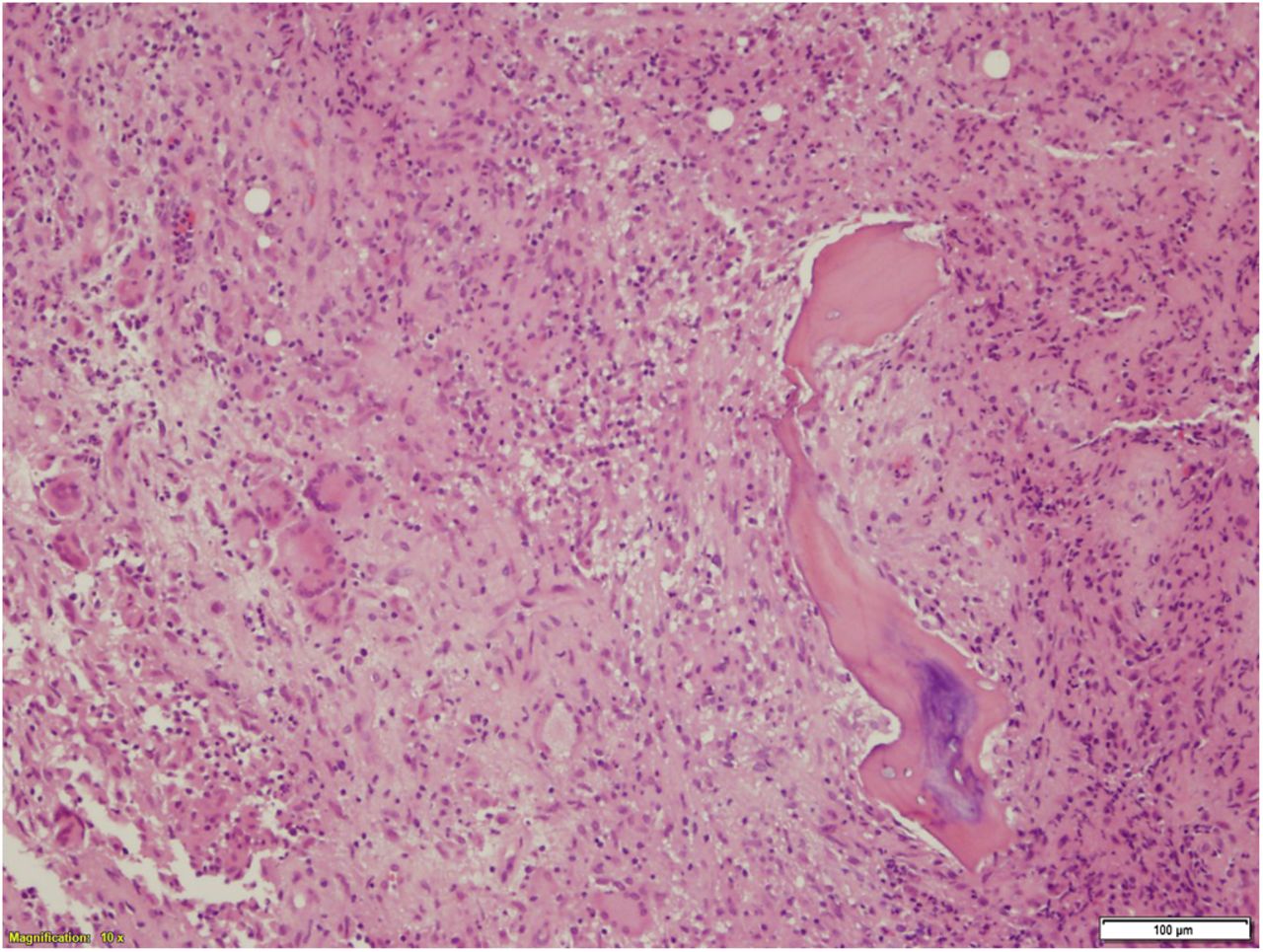
A fifty-seven-year-old white woman presented with sudden onset of pain in the left forefoot without history of trauma and no signs of inflammation. She had no history of recent travel abroad and had no tattoos; the medical records showed no evidence of chronic illness such as diabetes mellitus or immunodeficiency. A subsequent human immunodeficiency virus test was negative. As part of the initial assessment in the Emergency Department, radiographs of the foot were obtained. These radiographs were unremarkable. She was given analgesics and discharged home. Ten days later, the woman returned to the hospital with increased pain, redness, and swelling over the dorsum of the left foot (Fig. 1). The white blood-cell count was 8.6 × 10/L (normal range, 4 to 11 × 10/L), the C-reactive protein (CRP) level was 46 mg/L (normal range, 0 to 10 mg/L), the erythrocyte sedimentation rate (ESR) was 30 mm/h (normal range, 0 to 30 mm/h), and the fasting blood glucose level was 4.5 mmol/L (normal range, 3.5 to 5.5 mmol/L). Radiographs of the left foot were repeated and showed features suggestive of acute disease involving the first metatarsal (Fig. 2). Magnetic resonance imaging (MRI) of the foot was done. It showed a nonenhancing area at the base of the first metatarsal with cortical disruption (Fig. 3). The nearby tarsometatarsal joint was not involved. Debridement was performed. The metatarsal bone showed extensive destruction and had been replaced by firm yellow tissue; samples were sent for culture and histopathology (Fig 4).
Antibiotic treatment with daptomycin was then started. The bone biopsy showed chronic granulomatous inflammation composed of scattered Langhans-type multinucleated giant cells and epithelioid cells forming ill-defined noncaseating granulomata surrounding dead bone trabeculae (Fig. 4). The CRP level had dropped to 9 mg/L, and it was deemed appropriate to continue the current antibiotic treatment until a tuberculosis culture and results from a polymerase chain reaction probe were available; we acknowledged that additional debridement or first-ray amputation subsequently could be required. A molded cast was applied to allow the patient to bear weight. Two weeks later, the cultures were positive for a Mycobacterium chelonae infection, which is an atypical mycobacterial osteomyelitis; the antibiotics were modified based on the patient’s sensitivity to clarithromycin and ciprofloxacin. The antibiotics did not control the infection, the surgical debridement wound continued to discharge, and repeat radiographs showed progressive bone destruction (Fig. 5). After four months of antimicrobial therapy, first-ray amputation was performed to control the infection because the amount of metatarsal destruction was excessive and salvage was not possible. Antimicrobial treatment continued for a total of six months. A follow-up MRI excluded any additional deep-seated infection. The patient was fitted with an orthotic (insole) and was followed for eighteen months with no recurrence of infection.
Proceed to Discussion >>Reference: Tanagho A, Hatab S, Hawkins A. Atypical osteomyelitis caused by mycobacterium chelonae in a nonimmunocompromised patient: A case report. JBJS Case Connect. 2015 Feb 25;5(1):e17.
Nontuberculous mycobacterial infections are usually located in the lungs, the lymph nodes, the subcutaneous tissue, and the skin. Infections of bones and joints (particularly the spine) by nontuberculous mycobacteria are extremely rare and are usually misdiagnosed. Disease caused by M. chelonae usually occurs in immunosuppressed patients or in patients receiving corticosteroid therapy, as well as in patients with organ transplantation, rheumatoid arthritis, or autoimmune disorders. In most instances, osteomyelitis results from hematogenous spread, although direct extension from trauma and/or ulcers is also relatively common. Its incubation period lasts from one to two weeks, and the clinical manifestations are generally evident within four to six weeks. Increasing pain, absence of fever, or leukocytosis with a raised ESR are often the presenting features of these infections. In our patient, the portal of entry of the mycobacterial infection was not clear because she had developed the disease without a history of any wound or medical procedure. Diagnosis of nontuberculous mycobacterial osteomyelitis requires a high index of clinical suspicion. Laboratory tests are inconclusive most of the time. Radiographic and MRI appearances depend on the stage of the disease. In our patient, open biopsy for bacteriologic and histologic examination confirmed the diagnosis. Chemotherapy for M. chelonae infections has been problematic because of the paucity of effective oral antimicrobial agents. Fewer than 25% of the mycobacterium isolates are susceptible to doxycycline, minocycline, and ciprofloxacin. Clarithromycin is considered the drug of choice for the treatment of M. chelonae infection; however, clarithromycin should not be considered as monotherapy. The duration of treatment is not well established. Based on the in vitro susceptibility pattern of the isolate in our patient, ciprofloxacin was another antimicrobial agent used in the therapeutic regimen. In line with the literature, our experience with this case suggests that surgical intervention may be invaluable for the treatment of patients with M. chelonae infection. Surgery provides tissue specimens for accurate pathological diagnosis and antimicrobial susceptibility tests. In addition, surgical treatment is used as an adjuvant to antimicrobial chemotherapy and reduces mycobacterial load in cases of multidrug-resistant infections. In conclusion, M. chelonae infection may be manifested with primary osteomyelitis in immunocompetent individuals. Aggressive management, including the early use of invasive tests, is recommended. Combined pharmacologic and surgical treatment (ray amputation) cured our patient of this rare infection.
Reference: Tanagho A, Hatab S, Hawkins A. Atypical osteomyelitis caused by mycobacterium chelonae in a nonimmunocompromised patient: A case report. JBJS Case Connect. 2015 Feb 25;5(1):e17.
Giant cell tumor of bone
Aneurysmal bone cyst
Atypical mycobacterial osteomyelitis
Staphylococcal osteomyelitis
Osteoblastoma




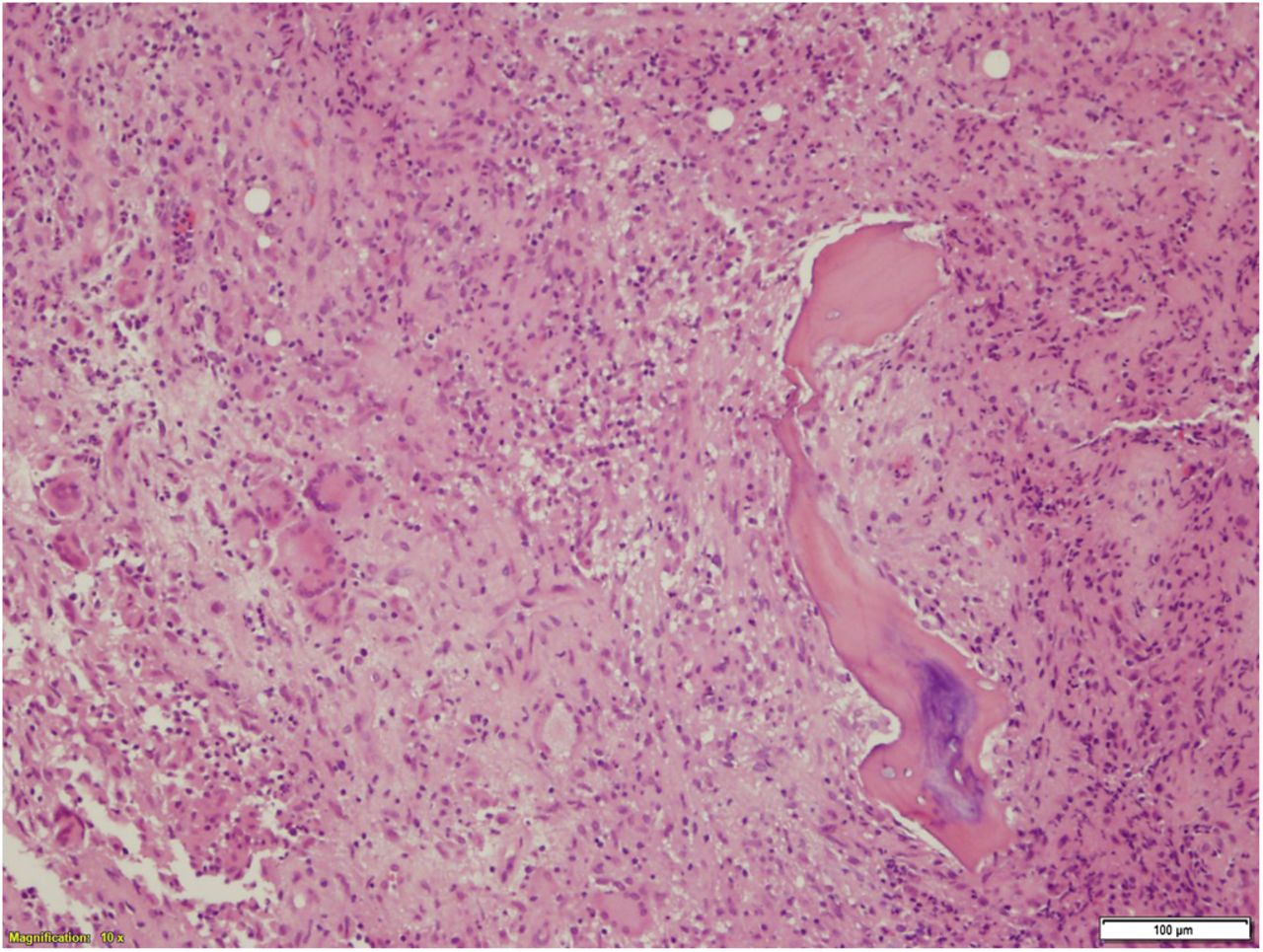
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4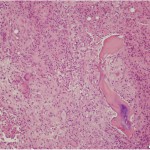 Fig. 4
Fig. 4 Fig. 5
Fig. 5