A Thirty-one-Year-Old Woman with Knee and Thigh Pain
March 4, 2015
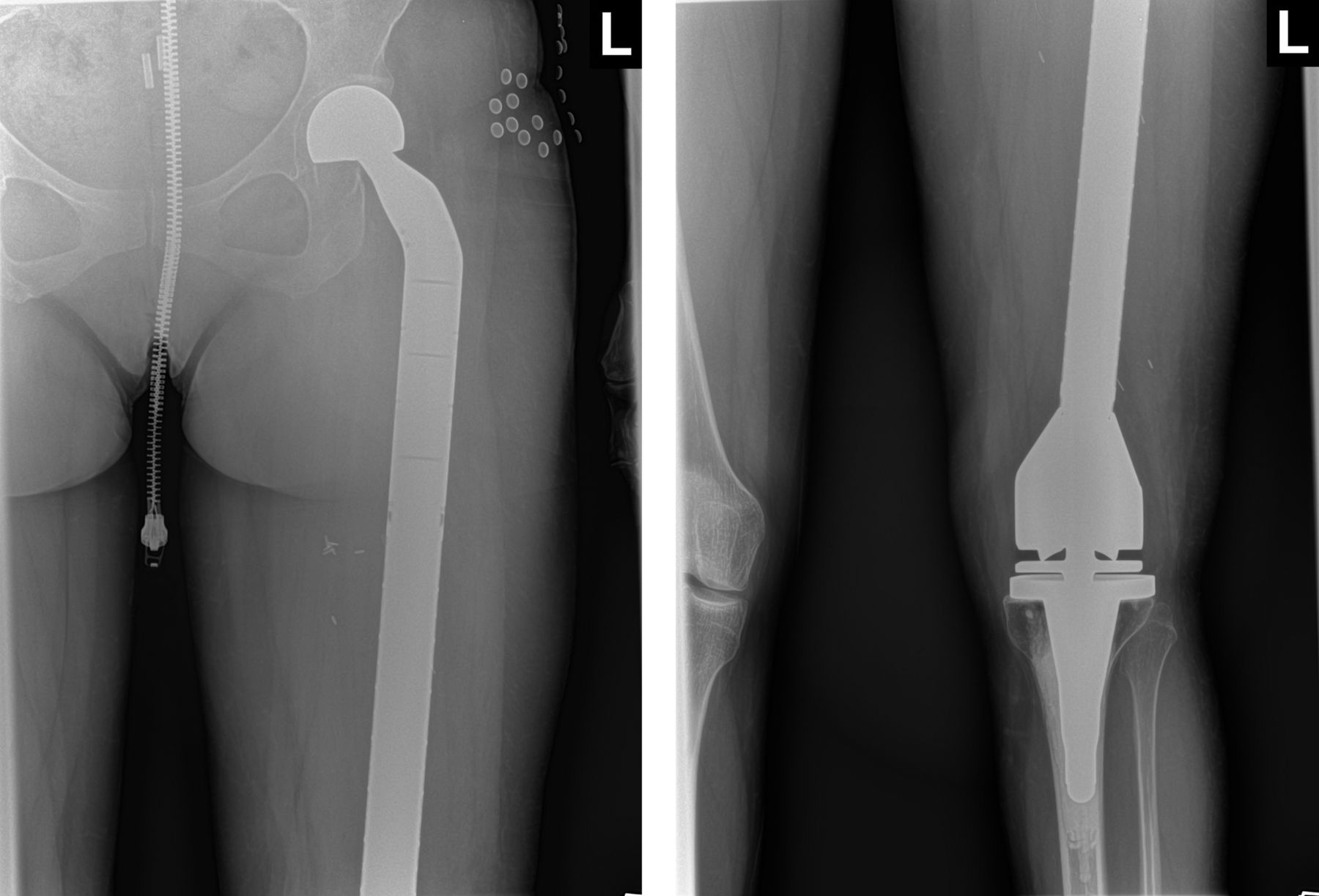
A thirty-one-year-old woman who had emigrated from Iraq eight years prior was referred to the orthopaedic oncology clinic with symptoms of left knee and thigh pain. The pain had begun six months prior with an insidious onset. It was a dull aching pain that worsened with activity; she also reported recent knee swelling. She denied night pain or constitutional symptoms. The left leg revealed diffuse thigh and knee tenderness. There was mild soft-tissue swelling, but no focal masses were present. She demonstrated full painless active range of motion of the knee. Radiographs revealed diffuse lytic changes throughout the diaphysis and distal metaphysis of the femur, with associated cortical thinning and erosion. Some sclerosis was present in the diaphysis, and the overall deformity of the bone suggested a long-standing process (Figs. 1-A, 1-B, and 1-C). Magnetic resonance imaging (MRI) of the left femur demonstrated a diffuse lesion from the greater trochanter to the distal articular region, with intense T2-weighted signal and cystic appearance. The MRI scan showed similar cortical scalloping as that seen on the radiographs. There was evidence of cortical breakthrough, and there were soft-tissue masses adjacent to the lateral diaphysis and medial metaphysis (Fig. 2). Given the wide differential and possibility of malignancy or infection, a biopsy was recommended. A core needle biopsy was performed in the region of the lateral soft-tissue mass, which revealed gross gray-white soft-tissue fragments. Frozen sections were concerning for possible malignancy. On final pathology, there were large areas of necrosis and evidence of chronic granulomatous inflammation. Uniquely, there were laminations seen on Grocott-Gomori methenamine silver (GMS) staining (Fig. 3). No intact organisms or remnants were seen.
With a diagnosis of osseous hydatid disease of the left femur, the patient was referred to an infectious disease specialist; an Echinococcus granulosus infection was confirmed via enzyme-linked immunosorbent assay (ELISA) serology. Computed tomography (CT) of the chest and abdomen was negative for hepatic cysts, which are common with E. granulosus. The patient was started on albendazole (400 mg twice daily for six months), which initially improved the symptoms. The patient returned almost one year after the original diagnosis with worsening leg pain. Given the extent of the disease within the femur, we did not believe that curettage would be successful in eradicating the disease. Also, there was concern about the possibility of anaphylaxis if the cyst contents were released. Since nearly the entire femur was involved, we felt that femoral resection and reconstruction with a total femoral prosthesis provided the best chance of cure. The patient was reluctant to have surgery, so she underwent a repeat six-month course of medical treatment. Similar to the results from the first course, the medication transiently improved the symptoms, but it did not alter the progression of the disease or the symptoms. Approximately one additional year passed before the patient was agreeable to surgical intervention because of persistent pain. Under general anesthesia, a wide resection of the left femur was performed, with care taken to maintain adequate margins of healthy tissue around the associated soft-tissue cystic components. The previous biopsy track was also excised. The defect was then reconstructed with the use of a total femoral endoprosthesis (MOST Total Femur System; Zimmer, Warsaw, Indiana). Final gross pathology showed the severity of the disease (Fig. 4). All margins were negative, and there was no evidence of cystic rupture during the resection. The patient returned for a one-year postoperative follow-up (Fig. 5). There were no signs of recurrence of infection. She continued to have some mild residual pain and some abductor weakness because of the pain, but she was able to function well without the use of assistive devices.
Proceed to Discussion >>Reference: Moore D, Baker KC, Les K. Hydatid disease of the femur treated with a total femoral replacement. A case report. JBJS Case Connect. 2015 Jan 28;5(1):e7.
Osseous hydatid disease is a rare manifestation of E. granulosus infection, occurring in less than 5% of those who are infected. It is exceedingly rare to see these infections in the United States, and of the few reported cases, most are in people who emigrated from endemic countries during the early-to-middle twentieth century. Our patient had emigrated from Iraq eight years prior to disease presentation. Since osseous hydatidosis is an indolent infection, many patients do not present with symptoms until the disease is locally extensive. Radiographs usually show evidence of lytic lesions with possible sclerosis and bone deformity, depending on the extent of the infection. Pathologic fracture is also possible. Advanced imaging such as MRI can provide additional characterization but is unlikely to be diagnostic. If the index of suspicion is high for an echinococcal infection, serologic tests (e.g., ELISA) can be helpful in confirming the diagnosis. If the diagnosis is unclear, a biopsy is recommended to look for microscopic evidence of hydatid disease. One possible complication with biopsy is that if the infection is localized to the bone, the procedure may allow it to spread to the soft tissues. Also, the cyst contents can induce anaphylaxis in some patients if released in substantial volume. Therefore, we recommend the use of needle biopsy to minimize these risks. Once the diagnosis is established, it is important to refer the patient to an infectious disease specialist to coordinate medical treatment and to look for other sites of infection, similar to staging a neoplasm, with CT of the chest and abdomen, and possibly a bone scan. Surgical resection has been shown to be the mainstay for definitive eradication. The use of certain anthelmintic agents, such as albendazole and mebendazole, has been shown to be effective. However, these agents are unlikely to resolve substantial osseous disease because of poor penetration; they serve more of an adjuvant chemotherapeutic role. In 1972, Booz published a case series of twelve patients. Seven of them had involvement of a long bone; five of these underwent curettage, and formalin was used as an adjuvant. Booz considered this treatment successful since all five went on to heal, but he did not follow them to determine rates of recurrence. In 1978, Ferrandez et al. presented a case series of nineteen patients in Spain. There was a high recurrence rate with curettage and grafting, and in later patients, they advocated radical resection with margins. In 2003, Herrera and Martínez reported on twenty-six patients. They concluded that successful eradication of infection was dependent on the ability to perform wide excisions; poor outcomes were seen when this was not possible (e.g., in the pelvis). These findings were confirmed by Loudiye et al. in 2003. Because wide excision of the infected bone and soft tissue has been shown to correlate with decreased rates of recurrence, others have applied orthopaedic oncologic principals to the treatment of echinococcal disease with success. Metcalfe and Grimer used a total humeral prosthesis in the treatment of humeral disease, and Neogi et al. used a femoral allograft in the treatment of femoral disease. Based on a literature review, we believe that our case report is the first documented use of a total femoral replacement in the treatment of echinococcal disease. In summary, osseous hydatidosis is a very rare disease, but it should be included in the differential diagnosis of patients with evidence of a destructive bone process, especially if they have had close contact with host animals or are emigrants from endemic countries. Diagnosis can be made based on serologic tests or biopsy. Because of the importance of wide excision and oncologic-type reconstructions, it is recommended that patients be referred to an orthopaedic oncologist for evaluation and treatment.
Reference: Moore D, Baker KC, Les K. Hydatid disease of the femur treated with a total femoral replacement. A case report. JBJS Case Connect. 2015 Jan 28;5(1):e7.
Malignant fibrous histiocytoma
Lymphoma of bone
Adamantinoma of bone
Hydatid disease of bone
Tuberculosis of bone

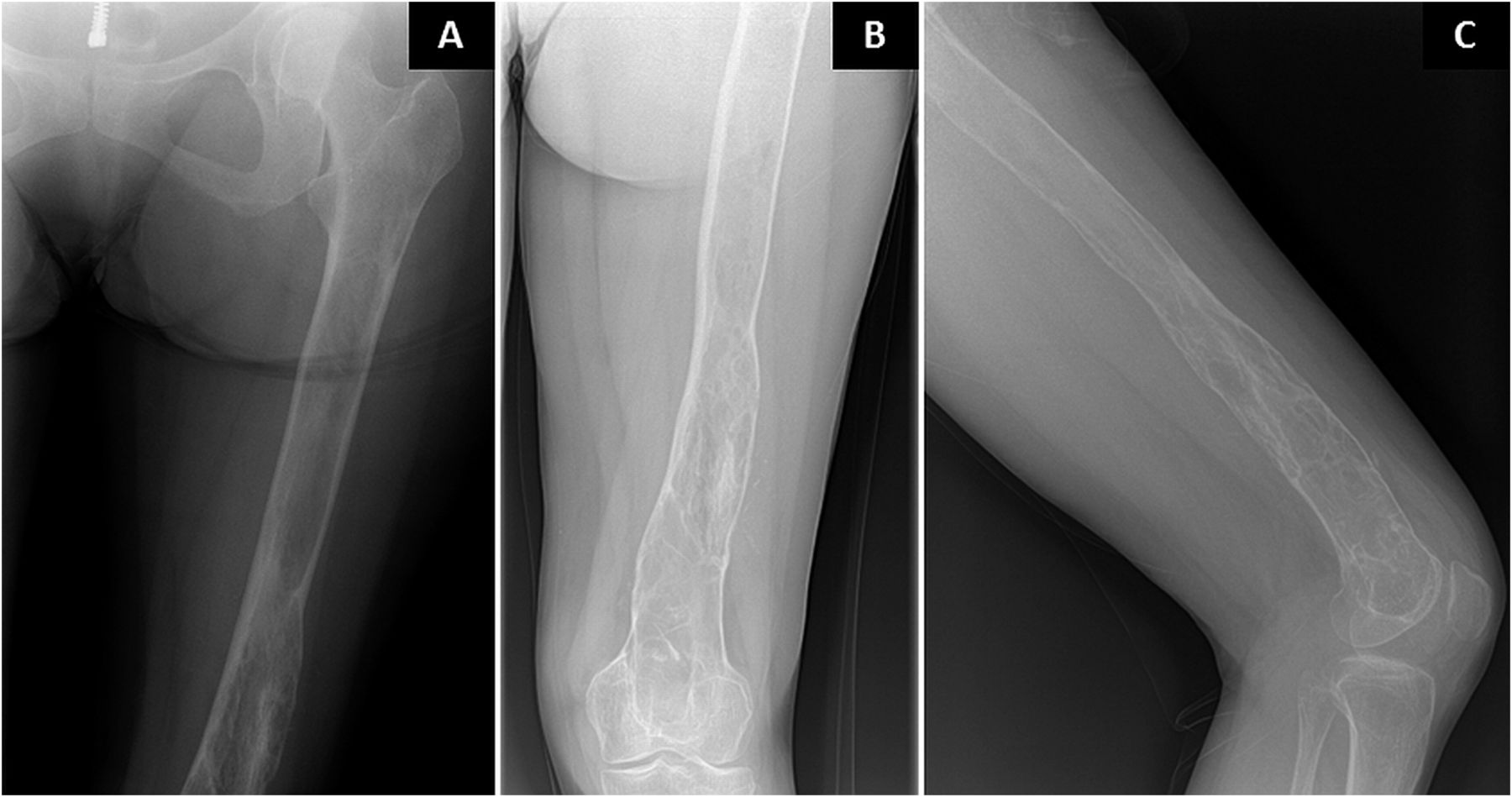
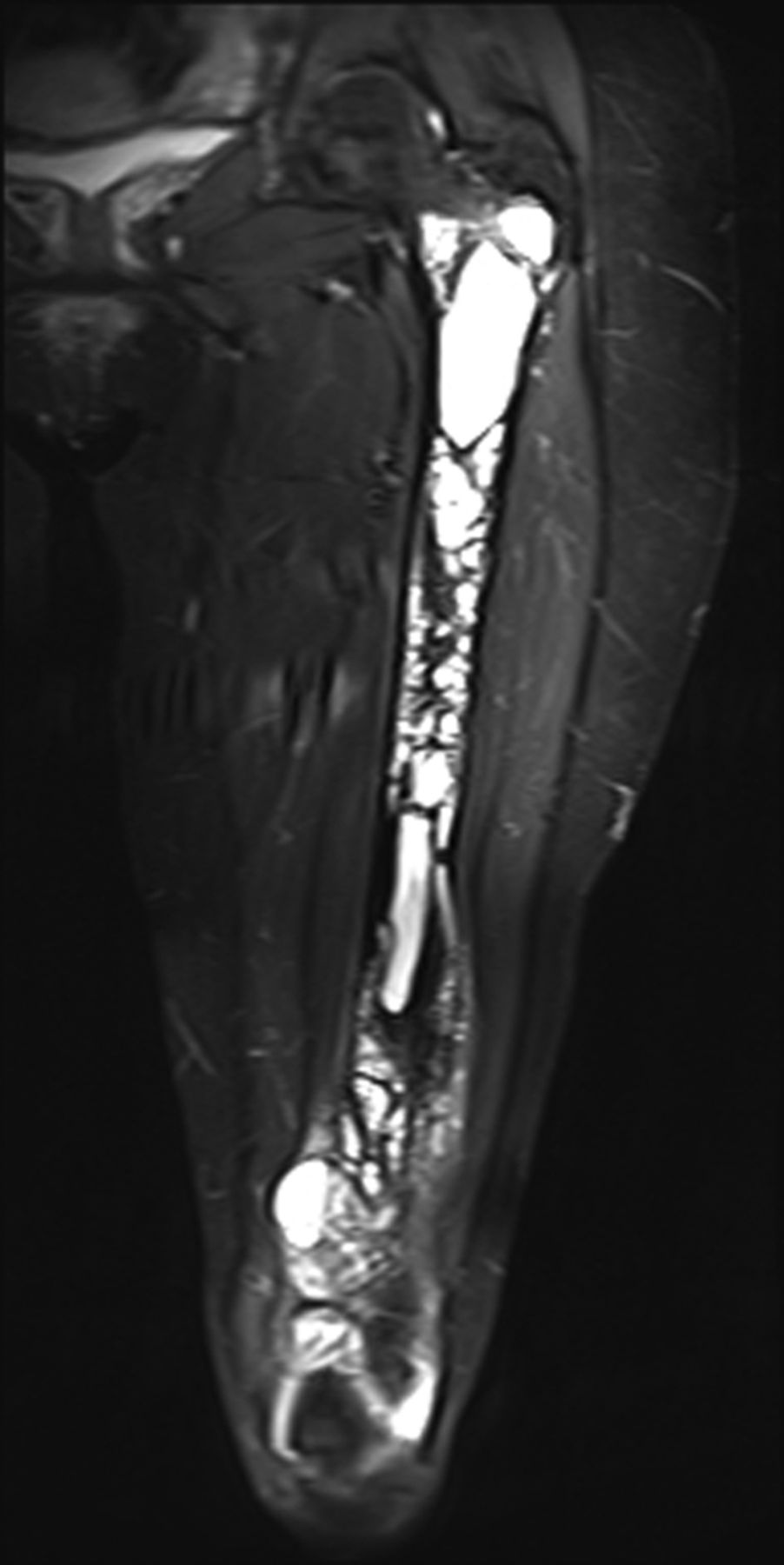
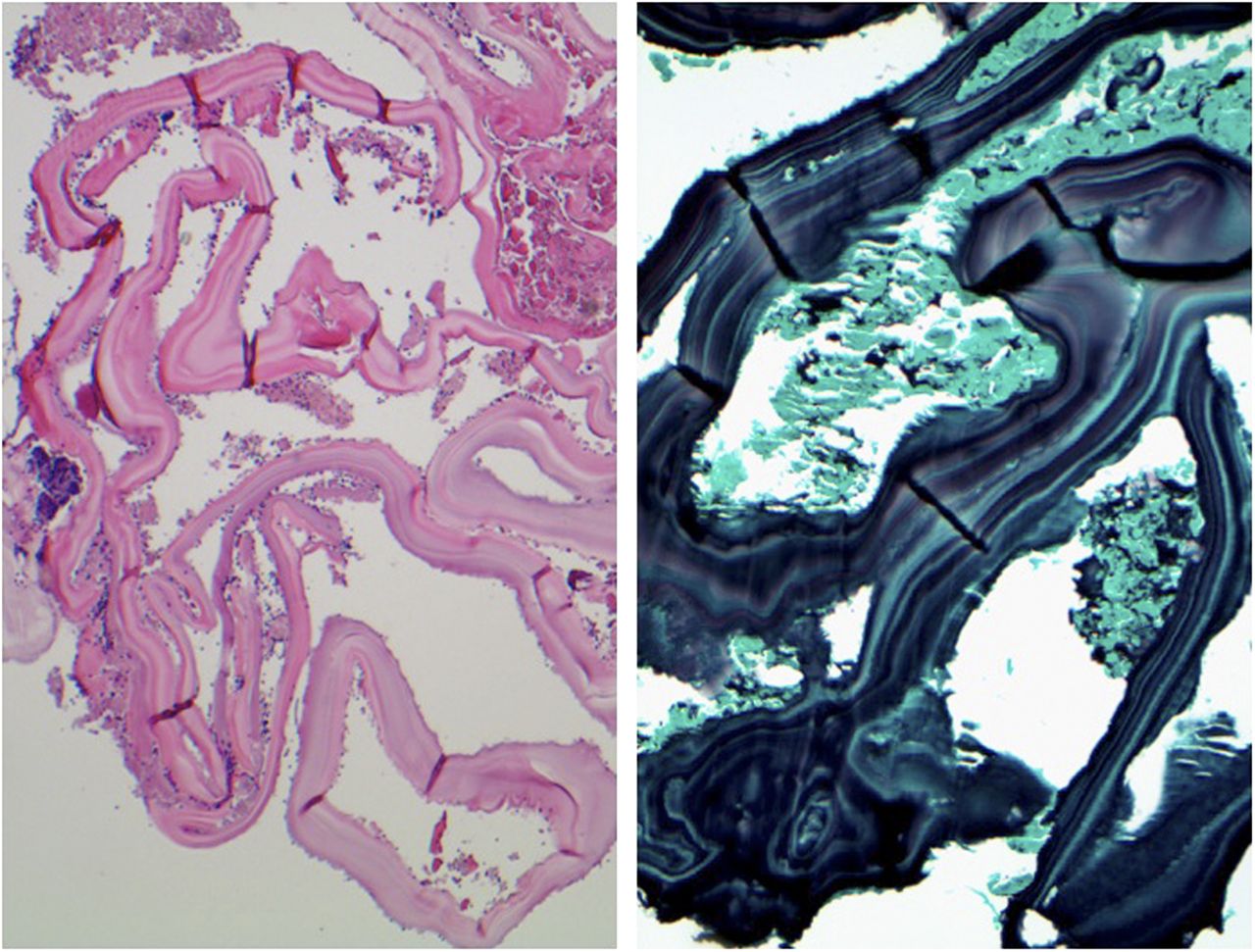
 Fig. 1
Fig. 1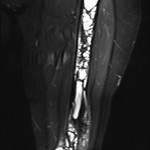 Fig. 2
Fig. 2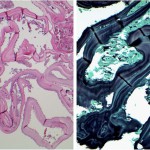 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5