A Seventy-three-Year-Old Woman with a Four-Month History of Knee Pain
January 21, 2015
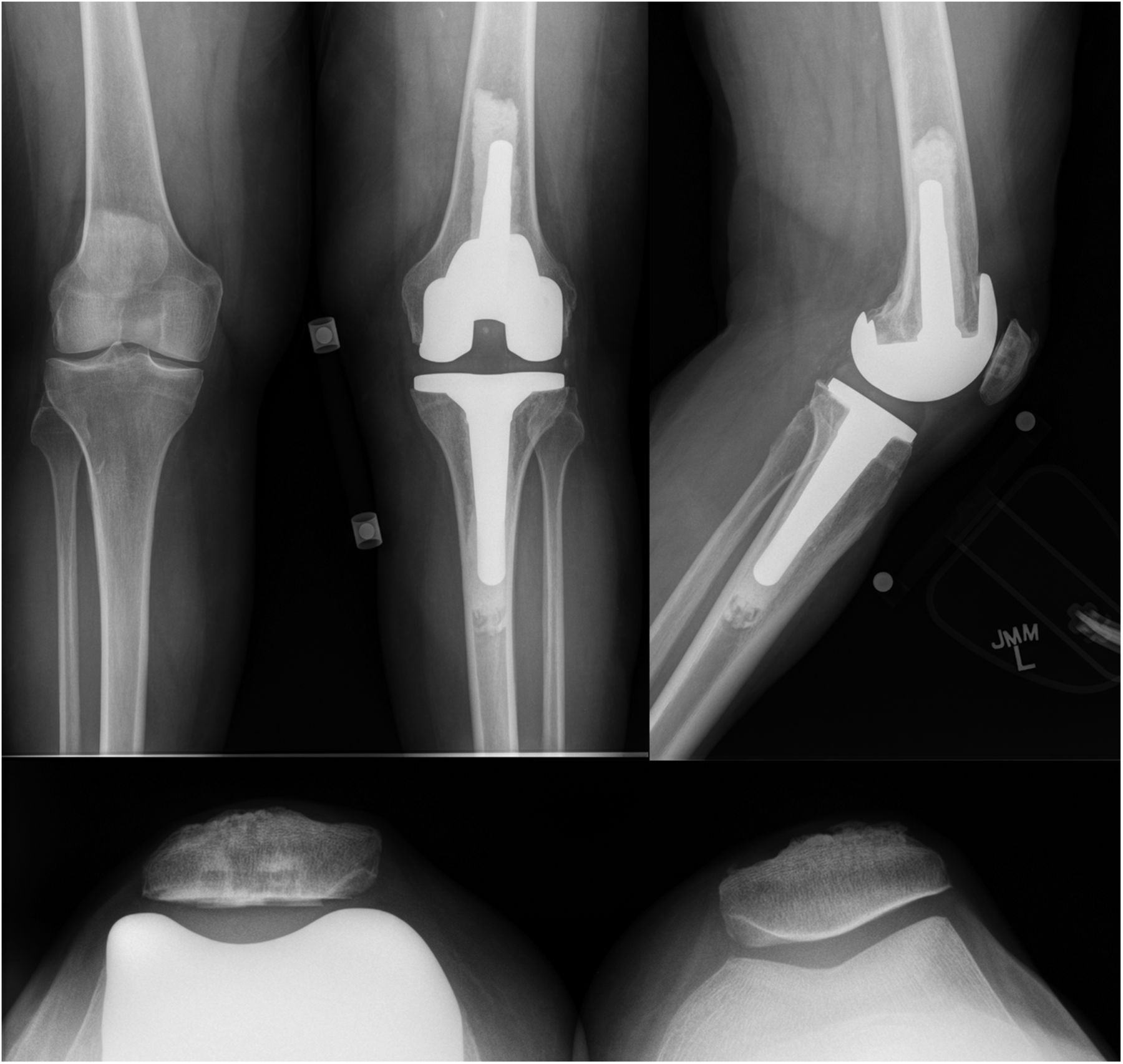
A seventy-three-year-old white woman presented to our clinic with a four-month history of knee pain. She had been evaluated at an outside facility and had been given the diagnoses of a medial meniscus tear and spontaneous osteonecrosis of the medial femoral condyle. She then presented to our clinic for a second opinion with regards to surgical intervention. The review of systems was unremarkable. The patient’s medical/surgical history was noteworthy for a remote twenty pack-year smoking history, cystic lung disease of unknown etiology, and numerous prior benign skin lesions. Examination for strength, sensation, and pulses of the affected limb was normal. The patient possessed full extension to 120° of flexion. She had 1+ medial pseudolaxity with a firm end point to valgus stress, with tenderness to palpation over the medial joint line, and a mild effusion. She had a normal hip examination. Radiographs were repeated and compared with those obtained two months earlier at the outside facility (Fig. 1). The radiographs suggested expansion in the size of the lesion. There were concerning features on the initial magnetic resonance imaging (MRI) as well (Fig. 1). Insufficiency fractures characteristically show decreased T1-weighted signal just beneath the cortex, with the presence of deeper residual marrow fat; the lesion in question demonstrated uniform replacement of the marrow on T1-weighted imaging with loss of deeper residual marrow fat. Based on this finding, a repeat MRI evaluation was conducted; given the low T1-weighted, high T2-weighted signal intensity nature of the lesion, combined with the marked marrow edema and the above-mentioned features (Fig. 2). The patient underwent computed tomography (CT)-guided biopsy of the lesion (Fig. 3).
The findings were interpreted to be metastatic adenocarcinoma, compatible with estrogen receptor/progesterone receptor positive primary breast cancer (Figs. 4-A through 4-D). The results were equivocal for HER2 protein expression on initial staining studies, and later fluorescence in situ hybridization (FISH) analysis also revealed this to be positive. Staging and a bone scan demonstrated no evidence of any other skeletal metastases. Both mammography and ultrasound detected a mass in the right breast. Anastrozole therapy was initiated, and she received a course of radiation. Because of continued knee pain, and no relief with a corticosteroid injection, she was felt to be an appropriate candidate for knee replacement surgery (Fig. 5). The patient was taken to the operating room for a total knee arthroplasty. She was found to have subchondral collapse of the medial femoral condyle (Fig. 6). Pathology of the lesion revealed no presence of viable metastatic tumor. Given concerns for bone quality and adequacy of osseous support, the patient was treated with a cemented posterior-stabilized rotating-platform total knee arthroplasty with cemented stem extensions. The patient was administered routine perioperative antibiotics and received six weeks of thromboprophylaxis with warfarin. Despite the prior radiation, the incision healed in pristine fashion. She was weaned off narcotics and gait aids early during recovery. At the two-year postoperative mark, radiographs demonstrated excellent appearance of the total knee arthroplasty, with no evidence of any wear, loosening, or recurrence (Fig. 7). With no pain or instability, she possessed full extension to 110° of flexion. She was not limited by the knee in any way and was very satisfied with the outcome. As for the overall cancer status, she had experienced slow progression of the metastatic disease, and alterations had been made to the chemotherapy regimen. She had developed brain metastases, which were treated with various courses of radiosurgery. Because one of the lesions involved the cerebellum, she required the use of a cane for balance purposes.
Proceed to Discussion >>Reference: Born TR, Rose PS, Mabry TM. Distal femoral subchondral metastasis mistaken for an insufficiency fracture and treated with total knee arthroplasty: a case report. JBJS Case Connect. 2014 Oct 08;4(4):e91.
We have described a case of a subchondral metastatic lesion of the distal medial femoral condyle that initially had been diagnosed as spontaneous osteonecrosis. Spontaneous osteonecrosis of the knee is more common in women than in men (3:1); it is unilateral in approximately 95% of cases. A misnomer, it actually represents a sequela of subchondral insufficiency fractures, which can collapse and induce areas of bone necrosis. Typically, this occurs in the setting of radial meniscal tears, due to loss of hoop stresses, and can be accompanied by meniscal root injuries in up to 80% of cases. Our patient’s history of injury with a concomitant medial meniscal posterior horn tear may have lent credence to the initial diagnosis of spontaneous osteonecrosis by the other physicians. However, certain aspects of the disease course and imaging characteristics (i.e., increased size of the lesion in a relatively short period of time and the MRI findings) demanded additional investigation. This led to the biopsy and the final diagnosis. Metastases to bone are very common in the setting of breast cancer. Periarticular metastases to the knee are exceedingly rare, and those to the subchondral region are even rarer. With the most common presentation being a well-circumscribed lytic lesion on radiographs, an epiphyseal metastasis can often be mistaken for other entities, including a cyst, a giant cell tumor, an infection, crystalline or inflammatory arthropathy, or ischemic necrosis. In contrast to our patient, the identity of the primary malignancy is often known in many of these cases. Additionally, case reports exist regarding patellar and synovial metastases to the knee joint, with primary lung cancer being the most common to metastasize to articular surfaces. Periarticular metastases have even been documented as the cause of pain after a total knee arthroplasty. One-tenth of patients with breast cancer develop symptomatic bone metastases, and one-fifth require surgical intervention. Metastatic disease is most commonly seen in the spine and pelvis; however, surgical treatment of pathologic sequelae from breast cancer is most common for the proximal part of the femur. There are very few reports in the literature regarding the use of total knee replacement to treat periarticular metastatic disease. There are more data describing treatment around periacetabular and proximal femoral lesions with total hip arthroplasty and proximal femoral replacement. Ghert et al. and Sarahrudi et al. found that patients with breast cancer as the primary malignancy had improved mean survival following surgical treatment of metastatic disease of the acetabulum and femur, respectively, when compared with other primary malignancies. Additionally, Koizumi et al. demonstrated that a solitary metastatic bone lesion was an independent favorable prognostic factor in breast cancer patients with skeletal metastasis. In a survival analysis of patients with femoral metastases by Mavrogenis et al., thirteen patients underwent a distal femoral replacement, but none underwent a total knee arthroplasty, most likely because of the rarity of an isolated subchondral metastasis. Hattori et al. performed resection and modular megaprosthetic reconstruction in twenty-two patients with femoral bone metastases. Total knee arthroplasty was utilized in only one of their patients. The main principles that were followed with our patient were meticulous care of the soft tissues, the use of antibiotic-impregnated bone cement, utilization of cemented stemmed fixation, and careful postoperative rehabilitation with extended thromboprophylaxis because of the elevated risks of venous thromboembolism (VTE) in the setting of malignancy. Approximately 1% of breast cancer patients develop VTE within two years, with the risk of VTE being the highest in the first six months following diagnosis. The use of radiation therapy is known to increase the risk of subsequent infection and prosthetic failure. Antibiotic-impregnated cement is routinely used at our institution in the treatment of patients with metastatic bone disease because of the increased risk of infection in this population. This case highlights the recognition of a periarticular metastatic lesion that simulated a subchondral insufficiency fracture, and the successful use of knee arthroplasty to restore function. Orthopaedic surgeons treating patients with degenerative conditions about the knee should be aware of the remote possibility of a periarticular metastasis. Axial imaging such as CT or MRI can be obtained if there are concerns about this diagnosis based on the radiographic findings or clinical evolution. If the diagnosis remains in doubt, a biopsy should be considered. Planning for such a biopsy should always be made in conjunction with an orthopaedic oncologist since the potential for major complications or an alteration in the surgical plan is much higher when the biopsy is inappropriately obtained. If a workup is not performed preoperatively and suspicious-appearing tissue is encountered during arthroplasty surgery, histopathologic analysis, including a frozen section, can still be conducted. Rubin et al. performed a meta-analysis of unexpected findings in routine histopathology during total joint replacement, and they recommended reserving this tool for cases in which there is controversy regarding the primary diagnosis or if there are unexpected findings during surgery. For patients with a metastatic lesion about the knee that is isolated to the subchondral region, treatment in the form of total knee arthroplasty is a viable option that can provide excellent pain relief and function.
Reference: Born TR, Rose PS, Mabry TM. Distal femoral subchondral metastasis mistaken for an insufficiency fracture and treated with total knee arthroplasty: a case report. JBJS Case Connect. 2014 Oct 08;4(4):e91.
Subchondral metastatic adenocarcinoma
Osteonecrosis of the femoral condyle
Osteochondritis dissecans
Chondrosarcoma
Subchondral insufficiency fracture

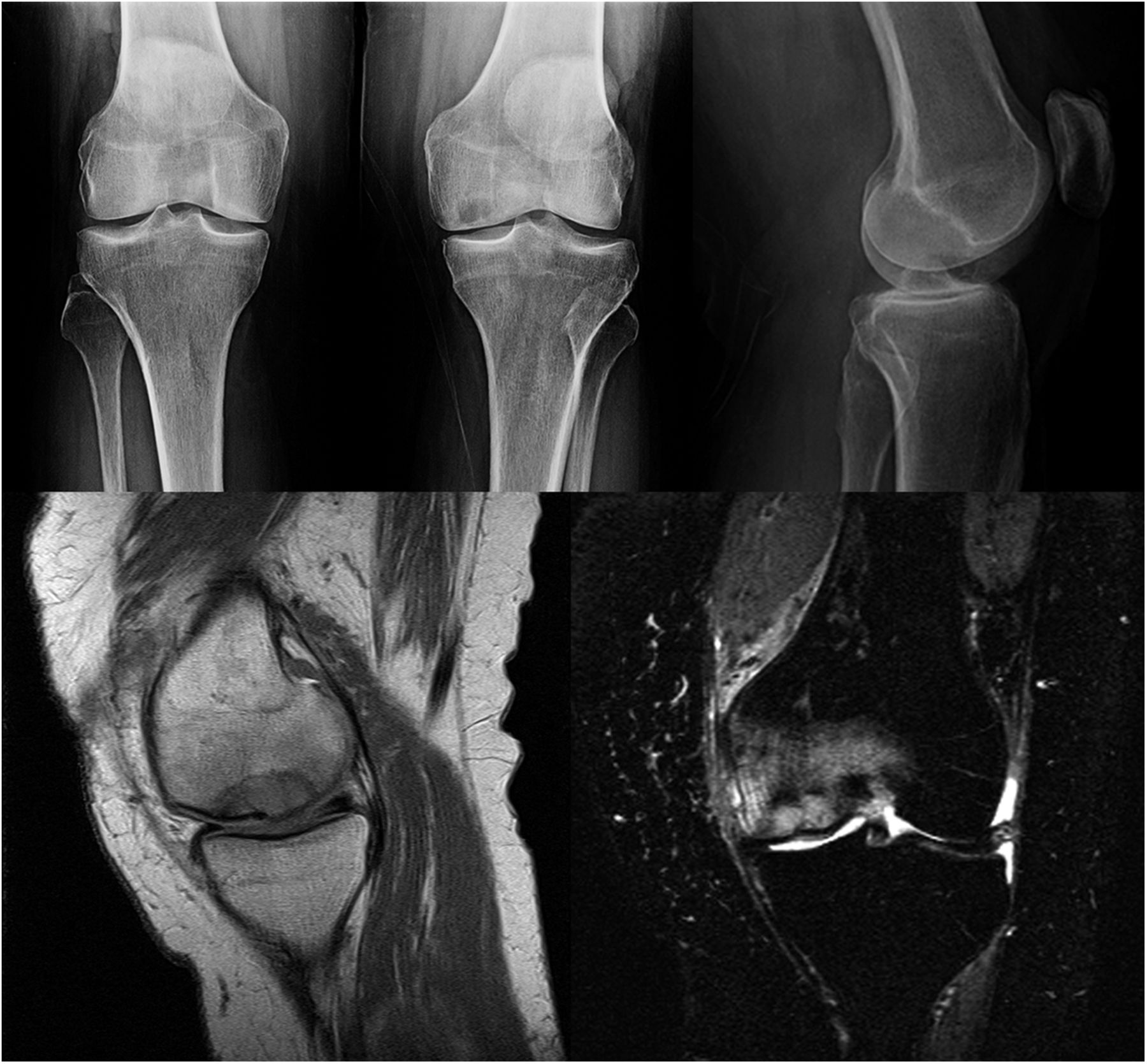
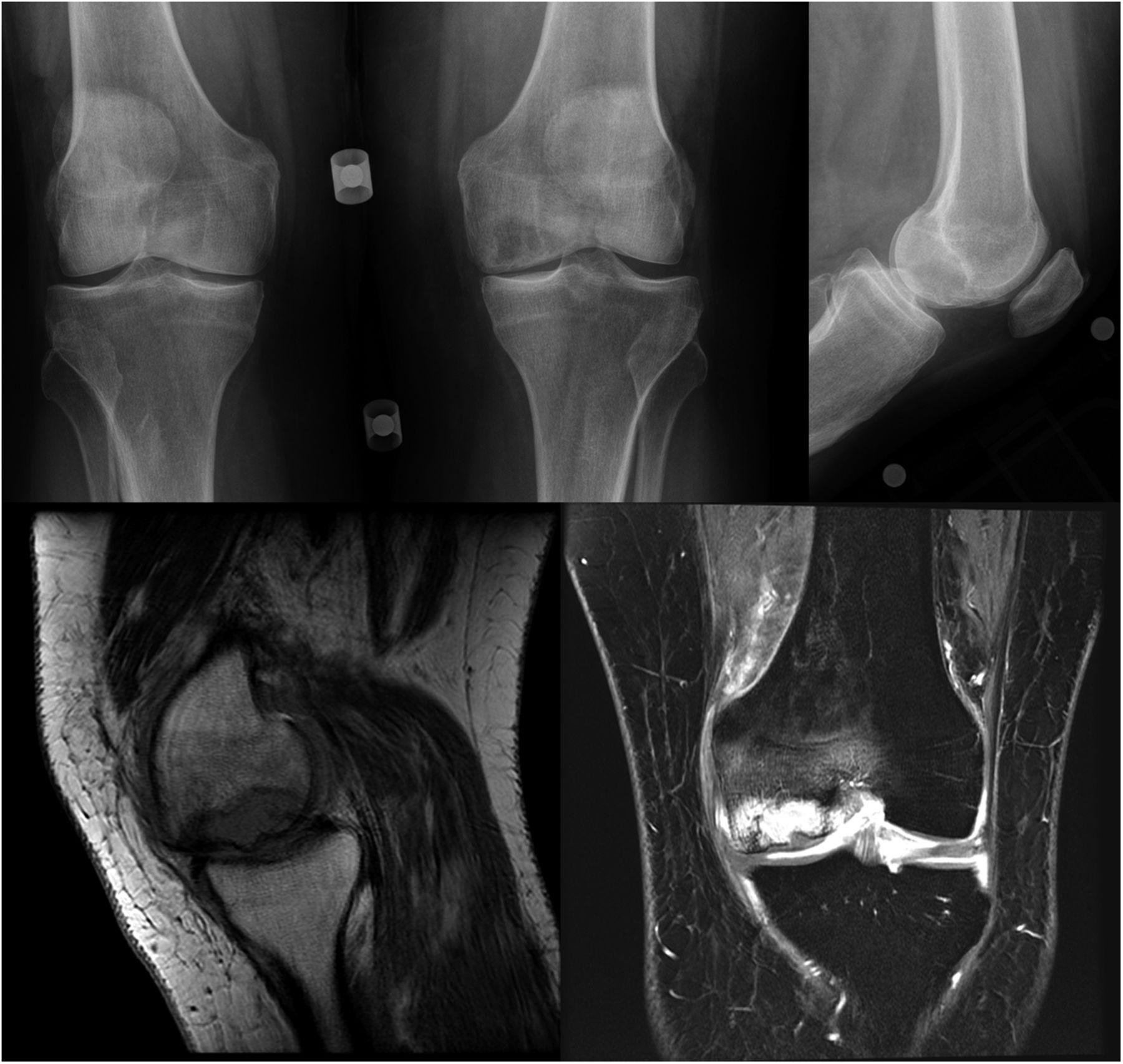
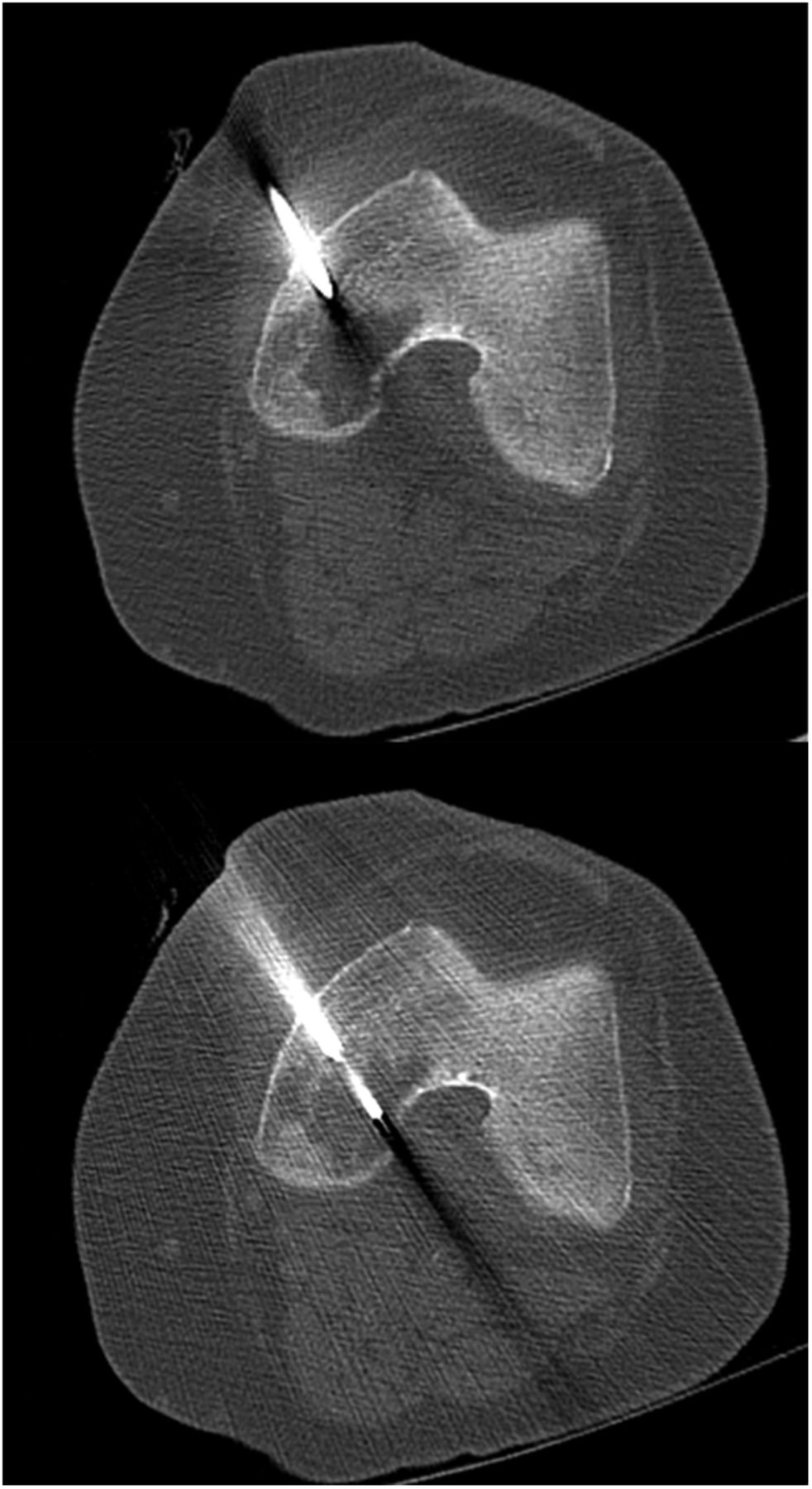
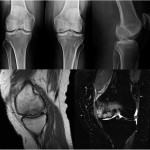 Fig. 1
Fig. 1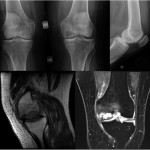 Fig. 2
Fig. 2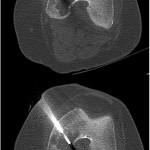 Fig. 3
Fig. 3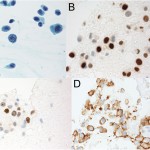 Fig. 4
Fig. 4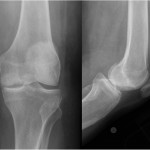 Fig. 5
Fig. 5 Fig. 6
Fig. 6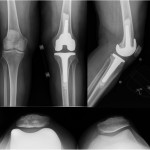 Fig. 7
Fig. 7