A Seventy-four-Year-Old Woman with Severe Chronic Groin Pain
November 6, 2013
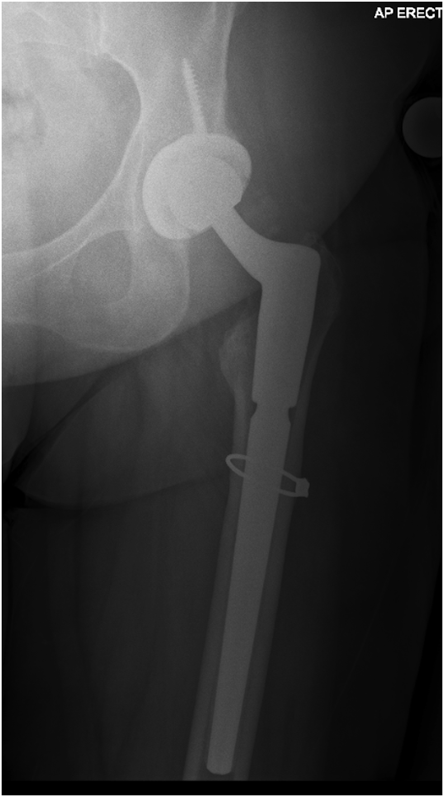
A seventy-four-year-old woman with postmenopausal osteoporosis had presented with severe chronic groin pain, reproducible on physical examination of the hip, and radiographic evidence of severe osteoarthritis of the left hip. An intra-articular cortisone injection three months prior to presentation had resulted in short-term pain resolution. The patient had undergone elective total hip arthroplasty, which was performed through a modified Hardinge approach, with use of a cementless proximally fitting tapered stem. Postoperatively, the patient had walked well with a rolling walker during physical therapy sessions, and she had required only intermittent oral opioids for pain control. At the three-week follow-up visit, she reported progressively worsening left thigh pain with weight-bearing. Radiographs demonstrated anterolateral femoral cortical thickening with transverse lucency at the distal third of an otherwise stable femoral prosthesis (Fig. 1). Retrospective review of the preoperative and immediate postoperative radiographs revealed subtle anterolateral subtrochanteric femoral cortical thickening without transverse lucency, which had previously been unrecognized (Figs. 2-A and 2-B).
The patient was admitted to the hospital, mobilized with restricted weight-bearing of the left leg, and started on oral calcium and vitamin D. Radiographs of the contralateral femur ruled out bilateral lesions. An endocrinologist was consulted. The patient reported a history of osteoporosis, which was diagnosed and treated by her gynecologist with ten years of continuous bisphosphonate therapy. The bisphosphonate had been stopped three months prior to presentation for the hip osteoarthritis. The patient had no history of fragility fracture. After discussing the potential risks, benefits, and current literature regarding teriparatide (Forteo; Eli Lilly, Indianapolis, Indiana), the patient opted against its use. Because no treatment guidelines exist for this type of atypical femoral fracture (AFF), a literature review was conducted. All treatment options were discussed with the patient, including nonoperative treatment, internal fixation, and femoral revision. After weighing the risks and benefits of each option, the decision was made to revise the femoral component with an implant that achieved fixation distal to the fracture. Through the previous incision and a modified Hardinge approach, the hip was exposed, and the partially ingrown stem was removed. At the lateral cortex of the femur, a stable unicortical fracture showing signs of cortical hypertrophy was identified. Given the unicortical nature and transverse orientation of the fracture, fixation of the fracture was not undertaken. A prophylactic cerclage was placed distal to the fracture, and the proximal part of the femur was prepared to accept a revision component. The surgeon chose a tapered modular stem, which is his prosthetic preference for femoral revision requiring distal fixation. Postoperatively, the patient maintained touch-down weight-bearing for six weeks and then advanced to full weight-bearing. Serial radiographs demonstrated a stable appearance of the femoral component and fracture-healing (Figs. 3 and 4). Six months after the revision surgery, the patient reported complete pain resolution.
Proceed to Discussion >>Reference: Reb CW, Costanzo JA, Deirmengian CA, Deirmengian GK. Acute postoperative bisphosphonate-associated atypical periprosthetic femoral fracture: a case report. JBJS Case Connector. 2013 Aug 28;3(3):e85.
Bisphosphonates substantially reduce the incidence of typical osteoporotic fractures. Bisphosphonate use leads to an estimated 47% reduction of typical osteoporotic fractures, and 144,670 such fractures were prevented between 2001 and 2008. Although a direct causal relationship between long-term bisphosphonate use and AFF has not been established, a growing body of clinical literature shows at least a correlation. Basic science and histological studies suggest a mechanism related to fatigue failure of bone, which is related to suppression of bone turnover and remodeling. Confounding, or perhaps compounding, factors include concomitant estrogen, glucocorticoid, or proton pump inhibitor therapy, as well as various comorbidities, including inflammatory conditions (e.g., Crohn disease, rheumatoid arthritis) and diabetes mellitus. These factors may predispose to AFF, even in the absence of bisphosphonate use. Meier et al. estimated the absolute incidence of bisphosphonate-associated AFF to be 32 per million person-years. The odds ratio of AFF increased with duration of use from 35.1 for less than two years to 175.7 for more than nine years. Schilcher et al. found a high rate of concurrent bisphosphonate use among patients with AFF; however, the absolute risk was small: fifty-five per 100,000 person-years. Currently, there are no controlled studies evaluating medical and surgical treatment protocols for the management of patients with AFF. The 2010 American Society for Bone and Mineral Research Task Force Report on AFF defined the case definition of AFF and made management recommendations. Medical interventions included protected weight-bearing, cessation of bisphosphonate use, optimal intake of calcium and vitamin D, and endocrinology consultation. Indications for surgical treatment with intramedullary fixation included painless nondisplaced fractures persisting beyond two to three months, all painful nondisplaced fractures, and all displaced fractures. Consideration of teriparatide therapy was recommended for cases where little evidence of healing was present at four to six weeks after surgery. Incomplete and nondisplaced AFFs that are not associated with prostheses often require surgical fixation. In a study by Mohan et al., the presence of thigh pain, periosteal beaking, and cortical black line were highly associated with fracture completion. Ha et al. found a high rate of fracture completion in nonoperatively managed incomplete or nondisplaced AFFs. Egol et al. reported a 49% failure rate with conservative management of incomplete AFFs. Surgical treatment resulted in a higher rate of healing, decreased time to healing, and greater incidence of pain resolution. Banffy et al. reported a displacement of 83% of nondisplaced AFFs that had been managed nonoperatively. The authors also found shorter average hospital stays in patients treated prophylactically (3.7 days) versus those treated after fracture completion (six days). Although rare, bisphosphonate-associated AFF may be a cause of pain following total hip arthroplasty, with the potential for catastrophic failure. Several cases of late nondisplaced periprosthetic AFF have been managed successfully with nonoperative treatment. Cross et al. reported a unicortical AFF about the distal third of a well-fixed cemented femoral component that occurred more than fifteen years after total hip arthroplasty, which resolved with protected weight-bearing and six months of teriparatide. Curtin and Fehring reported three cases of unicortical AFF that occurred three, fifteen, and eighteen years after total hip arthroplasty, all healing with protected weight-bearing and teriparatide therapy. Egol et al. reported on a periprosthetic AFF that had been successfully managed with plate-and-screw fixation; however, details of the case were not provided. We report the unusual case of a periprosthetic AFF, which became apparent in the early postoperative period. Retrospective review of the preoperative images revealed findings consistent with a proximal femoral stress reaction. This lesion went undetected because the radiographic findings were subtle and the patient had not reported a history of bisphosphonate use or thigh pain with weight-bearing. At the three-week postoperative visit, the patient reported increased pain, and radiographs demonstrated increased cortical hypertrophy and a unicortical fracture. Patient questioning then revealed the history of bisphosphonate therapy, which had been discontinued prior to the initial visit. While it is impossible to prove causality between bisphosphonate use and the postoperative fracture in our patient, the association seems likely. This case highlights the importance of obtaining a history of remote bisphosphonate use in patients indicated for total hip arthroplasty; careful inspection of radiographs when such a history exists is also necessary. There was little literature to guide decision-making in this case. Options to consider included nonoperative treatment, internal fixation, and femoral revision. Nonoperative treatment was not selected because prior literature has shown that AFFs often show delayed healing and progress to fracture completion or displacement. Additionally, the rapid evolution of the patient’s fracture suggested that the total hip arthroplasty had changed the stress pattern in the proximal part of the femur, which could possibly have decreased the success of nonoperative treatment. Open reduction and internal fixation with plate and screws is not recommended for AFF because of high failure rates and the fact that more reliable results have been demonstrated with intramedullary nail fixation. In periprosthetic AFFs, intramedullary nail fixation is not possible. Treating a periprosthetic AFF with open reduction and internal fixation is made more difficult by the presence of the femoral stem, which decreases the options for and security of fixation proximal to the lesion. Furthermore, a plate-and-screw construct is load-bearing, which raises concerns of plate fracture prior to bone healing in fractures at risk for delayed union and nonunion. Revision of late periprosthetic AFFs poses the challenge of removing the well-fixed prosthesis while maintaining the bone stock for subsequent reconstruction. In our patient, the acute presentation of the fracture afforded the possibility of removal of the proximally fitting implant prior to mature osseous ingrowth. Revision to a distally fitting component allowed for distal redistribution of the stress while maintaining proximal stability. In summary, an AFF may be the cause of periprosthetic pain. We report a case of an AFF that manifested acutely after total hip arthroplasty and was managed with early femoral revision. Additional study is necessary for determining the optimal method of managing periprosthetic AFFs. This case highlights the importance of scrutinizing preoperative radiographs for subtle signs of an evolving AFF in patients with a recent history of bisphosphonate use. When suspicion exists, we recommend evaluation with magnetic resonance imaging and careful consideration of femoral component options before primary total hip arthroplasty.
Reference: Reb CW, Costanzo JA, Deirmengian CA, Deirmengian GK. Acute postoperative bisphosphonate-associated atypical periprosthetic femoral fracture: a case report. JBJS Case Connector. 2013 Aug 28;3(3):e85.
Stress fracture of the upper femur
Intracortical chondroma
Iatrogenic femoral fracture
Atypical femoral fracture related to bisphosphonate use
Osteoblastoma

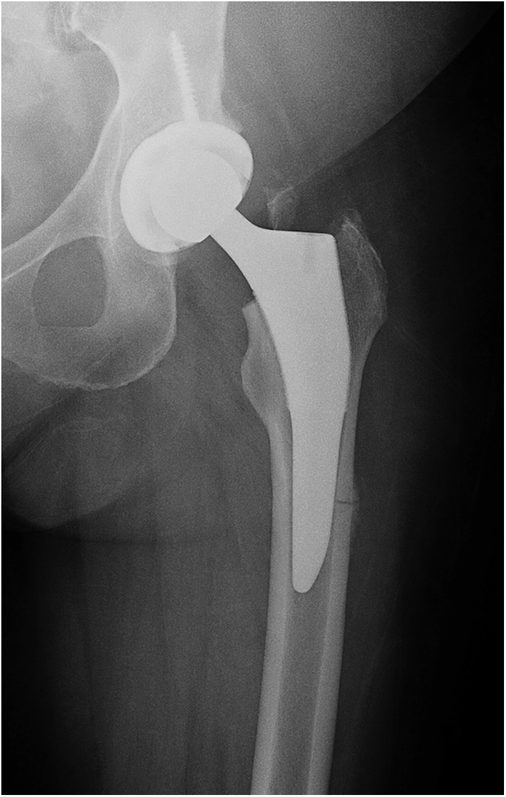
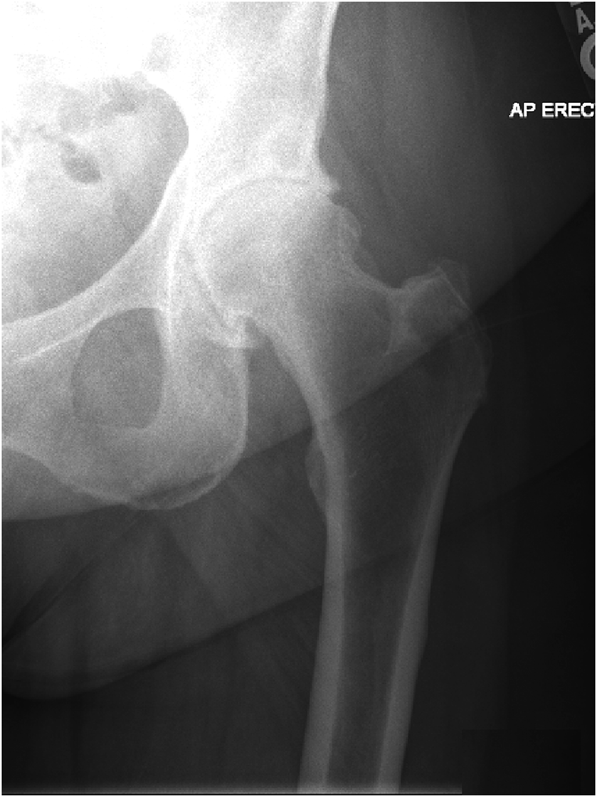

 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3
Fig. 3 Fig. 4
Fig. 4