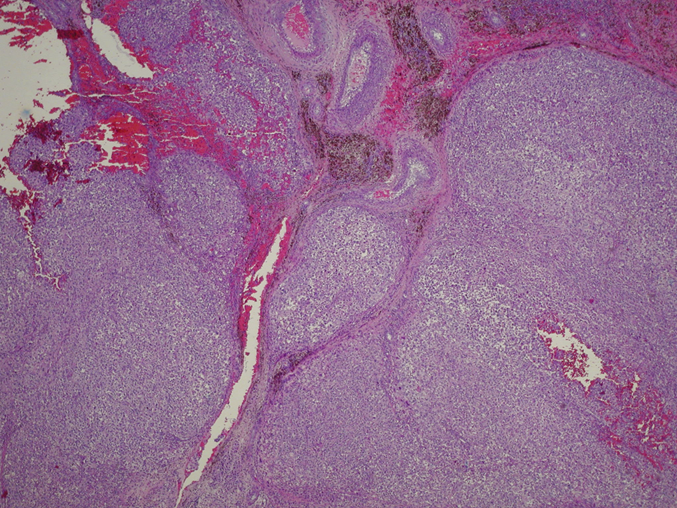
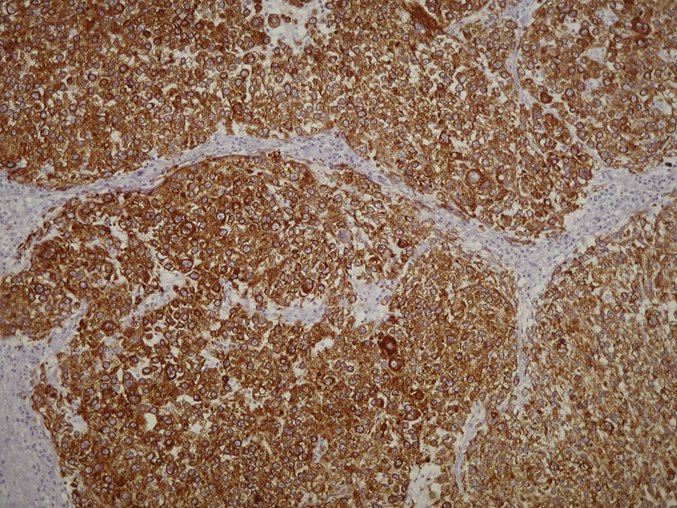
A sixty-five-year-old man presented with left knee pain. Previous medical history included hypertension, benign hypertrophy of the prostate, a sixty pack-year smoking history (stopped thirty years previously), and iron deficiency anemia; upper and lower gastrointestinal studies were normal. An MRI of the knee revealed normal menisci and ligaments, mild degenerative articular cartilage, and a 3.3 × 3 × 5.2-cm mass in the Hoffa fat pad (Figs. 1-A and 1-B). This mass demonstrated hemosiderin deposition and typical imaging features of local pigmented villonodular synovitis (PVNS) on T1-weighted, T2-weighted, and fat-saturation sequences. There was associated bone marrow edema in the adjacent tibial plateau. The patient was followed by his family physician with nonoperative treatment. The pain was progressive but partially relieved with anti-inflammatory medication and the use of a cane. Specialist consultation was not obtained until two years after the initial diagnosis when the patient sustained a fall to the affected knee and was no longer able to walk. Physical examination after the fall demonstrated a large intra-articular effusion, with diminished knee movement from 30° to 70° of flexion. There were palpable masses superior to the patella and tibial tuberosity. There was no adenopathy, and a neurological examination of the limb was normal. The patient stated that he voluntarily had lost thirty-five pounds. Knee aspiration was performed, and clear yellow fluid was noted. Radiographs (Figs. 2-A and 2-B) and MRI sequences (Figs. 3-A and 3-B) were obtained and revealed substantial progression of the disease. The primary lesion in the Hoffa fat pad measured 7.2 × 7.6 × 6.5 cm. Two satellite lesions had developed: one was anterior to the proximal tibial diaphysis (3.6 × 2.4 cm) and one was located at the insertion of the patellar tendon (1.5 × 1.6 cm). Additionally, the patellar tendon and the anterior aspect of the proximal tibial cortex were eroded by the intra-articular mass. Imaging signal intensity on the MRI was again thought to be characteristic of PVNS. Surgical resection of the intra-articular masses and a radical synovectomy were performed through an anterior medial parapatellar approach. Histological examination of the resected tissue is shown in Figures 4-A through 4-D.
The presumptive preoperative diagnosis was PVNS, but histological examination of an intraoperative frozen tissue section revealed a high-grade epithelioid malignancy suggestive of carcinoma. Despite the diagnosis of metastatic disease, it was decided to continue with the surgery as planned. The goals of the surgery were symptomatic relief as well as solid surgical fixation to allow early mobilization postoperatively. Forty percent of the patellar tendon had been eroded by the mass and was repaired with TWINFIX Ti 5.0 (Smith & Nephew) suture anchors and use of a Krackow suturing technique. Differential diagnosis included a primary epithelioid sarcoma, metastatic carcinoma, or metastatic melanoma. The mass was viscous and villonodular in appearance, with red and beige-brown regions. Multiple areas of hemosiderin deposition were found, but there was no evidence of prior or current PVNS. Extensive thin-slice examination of the specimen was performed as well as multiple immunohistochemical stains, which confirmed the diagnosis of metastatic carcinoma (Figs. 4-A through 4-D). These positive cytokeratin stains are consistent with metastatic carcinoma. A postoperative computed tomographic scan of the chest revealed a 2.5 × 2.0 × 3.5-cm mass in the right superior lobe. A positron emission tomography scan demonstrated no other suspicious lesions. Transthoracic biopsy was performed, and identical immunohistochemistry to the metastatic intra-articular mass was revealed. The patient underwent four courses of radiation therapy to the left knee and one reoperation and curettage over the next two years. He was unable to tolerate chemotherapy because of severe renal impairment and eventually died of fulminant pulmonary disease five years after the first MRI and 2.5 years after the first operation.
Proceed to Discussion >>Reference: Mutch JAJ, Doyon J, Mottard S. Intra-articular metastasis of lung carcinoma presenting as pigmented villonodular synovitis of the knee: a case report. JBJS Case Connector. 2013 May 08;3(2):e41.
PVNS is a benign neoplastic process involving the synovium of joints. It is a rare disease that occurs in approximately 1.8 patients per million population, typically presenting in young adults (average age of thirty-three years). The most commonly affected joint is the knee, which, in contrast to the hip and ankle, is rarely associated with cortical erosions. While MRI is an important diagnostic aid for this pathology, caution must be used. The characteristic findings of PVNS on MRI are primarily because of the organization of hyperplastic synovium into villi and nodules and the multiple depots of intracellular hemosiderin. The low signal intensity on T1-weighted, T2-weighted, and proton density-weighted sequences is due to the properties of hemosiderin. The “blooming” artifacts seen on gradient-recalled echo sequences also result from the presence of hemosiderin and are due to differences in ferromagnetic properties with adjacent healthy tissue. However, although hemosiderin deposition is typical in PVNS, it is not specific. Other nodular masses that may present with areas of bleeding include nodular rheumatoid arthritis, synovial sarcoma, hemophilic synovitis, or other traumatic lesions. Thus, while MRI can prove to be valuable in diagnosing PVNS, it is not specific and should always be interpreted in the clinical context and correlated with histopathology as necessary. Our patient was sixty-five years old, somewhat older than is typical for patients with PVNS, and was anemic at initial presentation. He additionally had a sixty pack-year smoking history and had lost thirty-five pounds, although he stated this had been voluntary. The second MRI (two years after initial presentation) demonstrated lesions that were quite aggressive in nature, distinct from the original mass, and eroding the anterior tibial cortex and patellar tendon. While this can occur in PVNS, it is unusual and should alert the treating physician to the presence of a more aggressive lesion. Intra-articular metastases are rare events, but older individuals or those with prior history of malignancy are most at risk. The knee is the most commonly affected joint, and although metastases that mimic mucoid degeneration of the anterior cruciate ligament or the meniscus have been described, they have not yet been described as mimicking PVNS. The possibility of a "collision lesion," namely a second malignancy arising within a pre-existing tumor (presumed PVNS in our patient), should also be considered. These lesions, however, generally contain evidence (islets) of the previous tumor cells; our patient showed no signs of PVNS on pathology. The prognosis associated with metastatic lung disease is generally poor, with an average survival of less than five months. Longer survival, however, has been described, with 11% of patients surviving longer than two years and up to six years in the case of solitary bone metastases. We present a case of a previously healthy patient with knee pain and MRI findings characteristic of PVNS. This lesion was due to an intra-articular metastasis of lung carcinoma. Aggressive features on MRI such as satellite lesions and cortical erosion should alert the treating physician to consider alternative diagnoses, and biopsy should be performed if the diagnosis is in doubt.
Reference: Mutch JAJ, Doyon J, Mottard S. Intra-articular metastasis of lung carcinoma presenting as pigmented villonodular synovitis of the knee: a case report. JBJS Case Connector. 2013 May 08;3(2):e41.
Metastatic carcinoma
Nodular rheumatoid arthritis
Synovial sarcoma
Epithelioid sarcoma
Metastatic melanoma

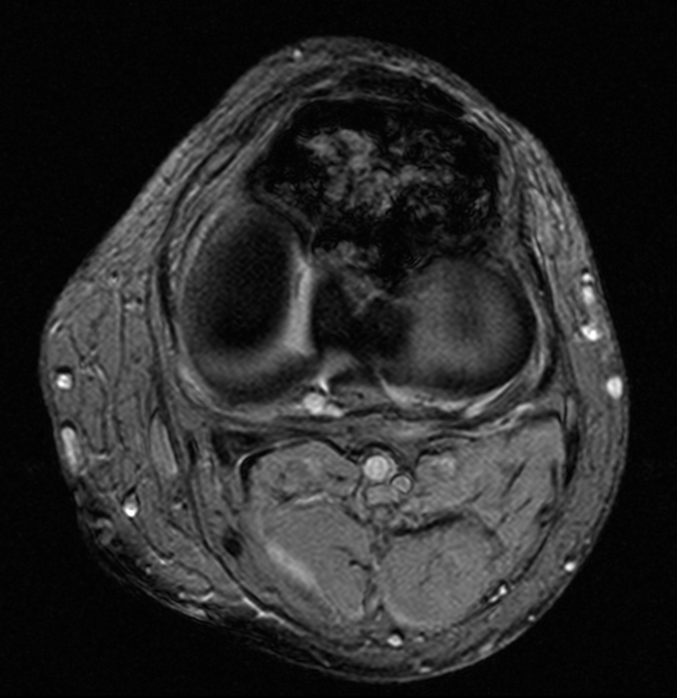

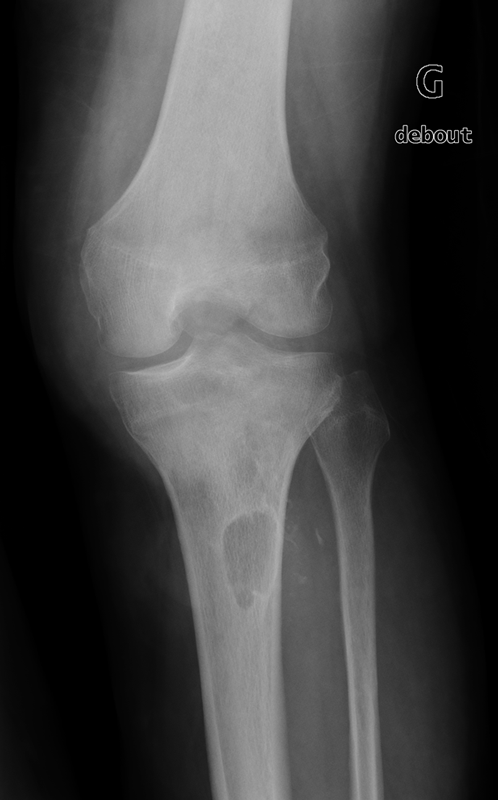
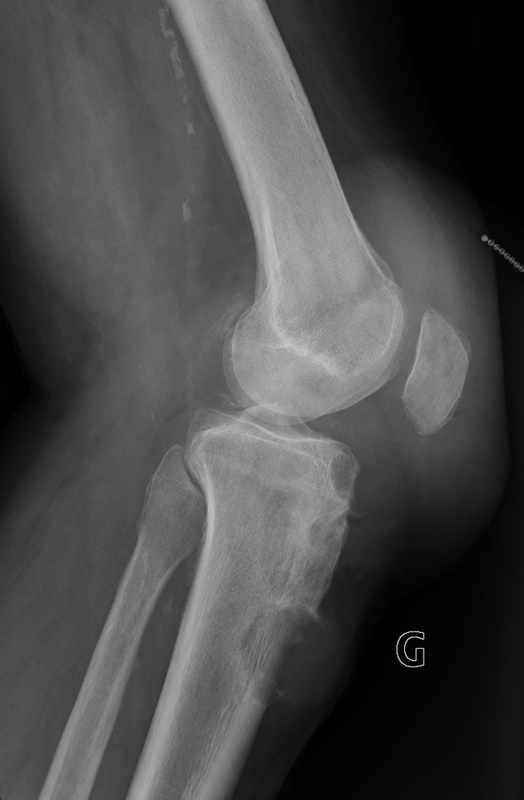
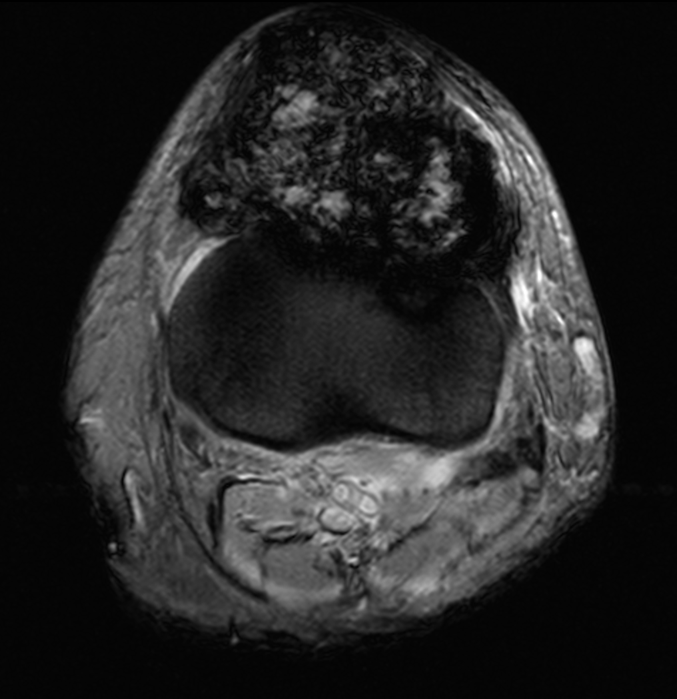
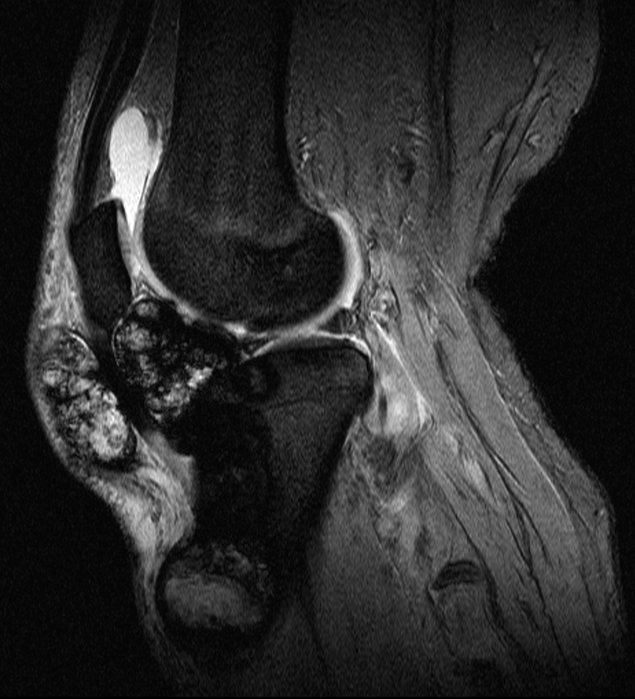
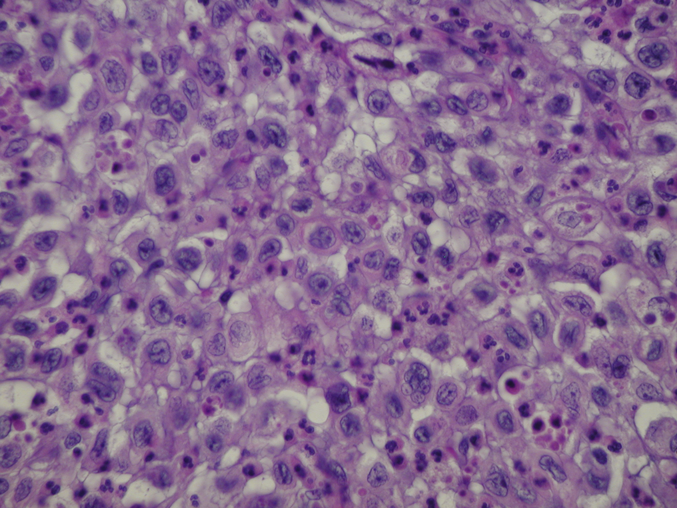
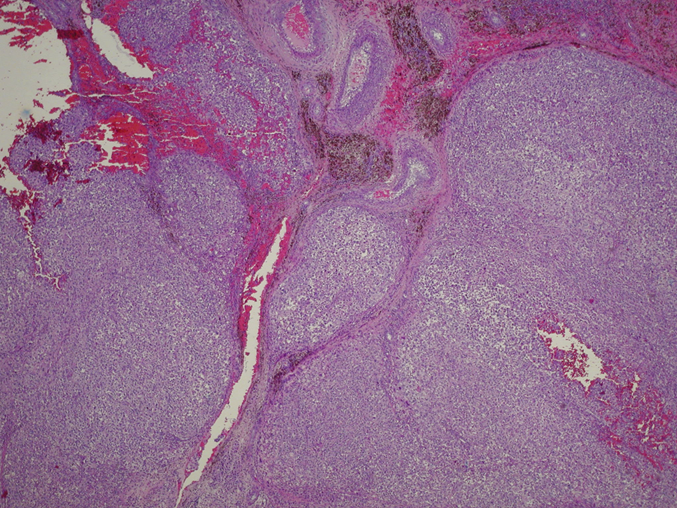
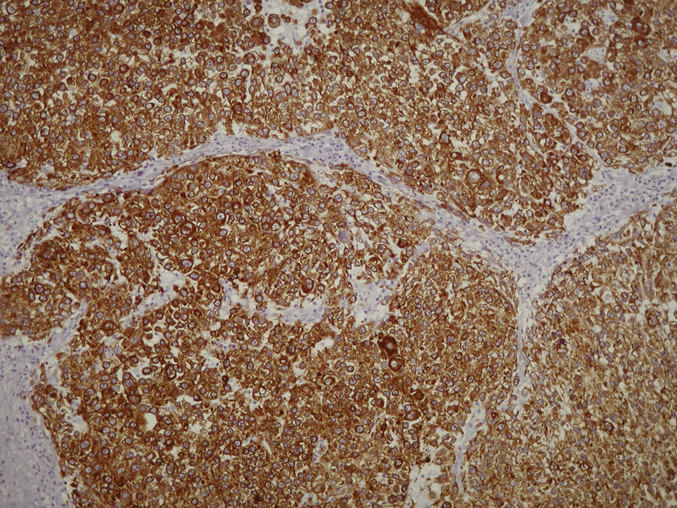
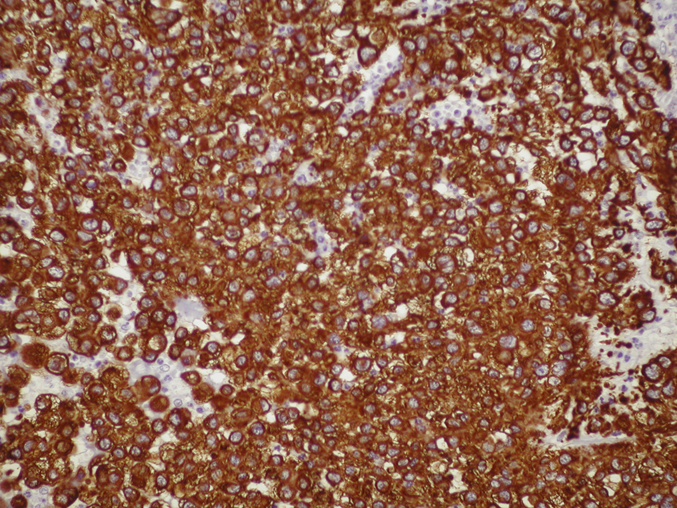
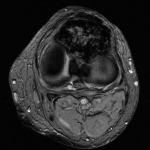 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B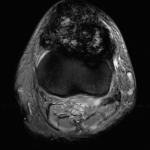 Fig. 3-A
Fig. 3-A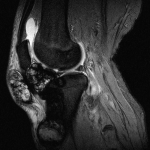 Fig. 3-B
Fig. 3-B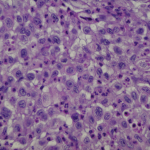 Fig. 4-A
Fig. 4-A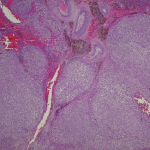 Fig. 4-B
Fig. 4-B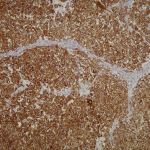 Fig. 4-C
Fig. 4-C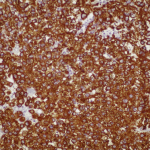 Fig. 4-D
Fig. 4-D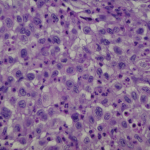 Fig. 4-A
Fig. 4-A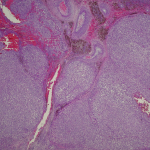 Fig. 4-B
Fig. 4-B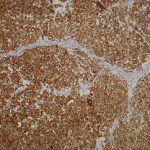 Fig. 4-C
Fig. 4-C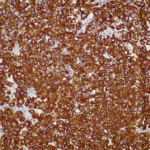 Fig. 4-D
Fig. 4-D