A Twenty-four-Year-Old Woman with Knee Swelling
March 20, 2013
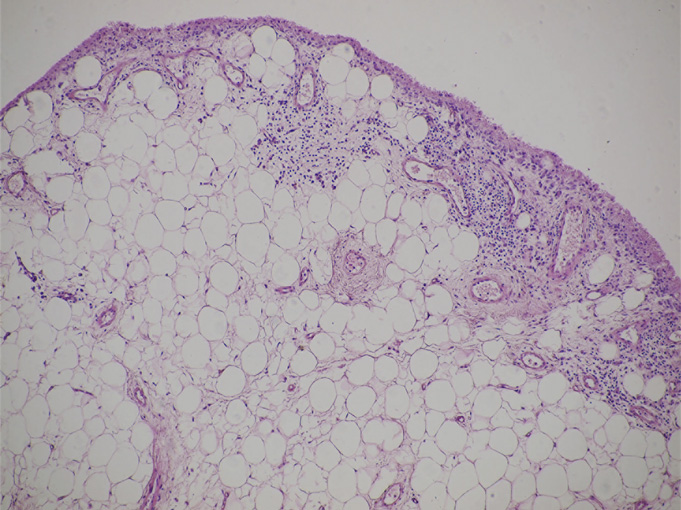
A twenty-four-year-old woman presented with painless swelling of the left knee after minimal trauma while exiting a car. The medical history revealed that effusions in the knee had been recurring for fifteen years for no particular reason. The remainder of the medical and family history was unremarkable. Physical examination showed an effusion in the left knee. Knee motion was 0° to 100° of flexion, with pain at the limit of flexion. Additional physical examination did not reveal any signs of meniscal or ligamentous injuries. Successive knee-joint aspirations were performed to relieve the symptoms. However, four to five days after each of these aspirations, the effusion recurred. The results of laboratory tests, including erythrocyte sedimentation rate, serological tests for rheumatoid factor, and blood uric acid, were within normal limits. The joint-fluid culture was negative for urate crystals, cells, and bacteria. An ultrasound examination showed mild narrowing of the joint space, with villous proliferation of the synovial membrane (Fig. 1). Magnetic resonance imaging (MRI) demonstrated proliferation of the synovial membrane in the suprapatellar pouch, with a joint effusion. Axial T2-weighted sections revealed massive synovial proliferation (Fig. 2). This proliferation generated a characteristic high-intensity signal on T1-weighted images (Fig. 3). After the evaluation, the patient was admitted to the hospital for diagnostic arthroscopy. During surgery, it was noted that there was marked proliferation of the yellow-white synovial membrane, which formed numerous villi, located mainly in the suprapatellar pouch (Fig. 4). Articular cartilage of the medial compartment tissue was obtained for microscopic examination, and it was fixed in 10% buffered formalin for additional examination (Fig. 5).
After the diagnostic arthroscopy had been performed, the patient was discharged from the hospital. Microscopic examination of the specimens revealed villous projection of the synovial membrane, with cell hyperplasia of the synovial lining. There was nearly complete replacement of the subsynovial layer by mature fat cells. Furthermore, focal chronic inflammatory infiltrate, consisting of lymphocytes and plasma cells, was observed (Fig. 5). These findings confirmed the diagnosis of lipoma arborescens. After obtaining the results of the microscopic examination, the patient was admitted to the clinic two weeks later, and arthroscopic synovectomy was performed. Subsequently, two drains were used to control the bleeding and to prevent a hematoma within the knee. The volume of blood collected was 200 mL, and the drains were removed after two days. A brace was applied to the left knee for four weeks following the surgery to protect the knee from accidental trauma and to allow healing. The patient was encouraged to perform isometric thigh exercises to prevent muscle atrophy. There was mild transient pain of the joint for four weeks. At the sixteen-month follow-up, she had no effusion or pain in the left knee
Proceed to Discussion >>Reference: Jurkiewicz A, Krakowski P, Korolczuk A. Lipoma arborescens of the knee treated with arthroscopic synovectomy: a case report and review of the literature. JBJS Case Connector. 2012 Sep 26;2(3);e53.
Lipoma arborescens is an uncommon condition that usually affects the knee, but it may occur in other joints as well. When the lesion is located within the knee, it has a predilection for the suprapatellar pouch. The lesion is more common in men than in women, and it has been reported in a wide age range (nine to sixty-eight years). In most cases, the lesion develops without an association with any known joint disease. Some authors suggest that the lesion has traumatic, inflammatory, or neoplastic origin. It may develop as a complication of trauma or several disorders, including osteoarthritis, chronic rheumatoid arthritis, or tuberculosis. However, the etiology of lipoma arborescens is still not fully known. It is postulated that lipoma arborescens predisposes to osteoarthrosis because degenerative joint changes have been reported in many cases. Ryu et al. reported bone erosion in three of eight patients diagnosed with lipoma arborescens. Additionally, Hallel et al. reported chondromalacia in a nine-year-old girl who had been diagnosed with lipoma arborescens. The clinical presentation, laboratory tests, and conventional radiographic findings of lipoma arborescens are nonspecific. Patients usually complain of progressive joint effusion. As the volume of effusion increases, pain and limitation of motion often develop. Many patients are symptomatic for a number of years. Typically, synovial-fluid cultures are negative for crystals and bacteria. In some cases, radiographs may reveal a soft-tissue lesion within the joint, accompanied by osteoarthritic changes in some patients. MRI examination of lipoma arborescens reveals three common characteristic patterns: multiple villous lipomatous synovial proliferation (occurring most often), an isolated frondlike subsynovial mass, and a mixed pattern. The lesion demonstrates the same signal intensity as fat on all sequences, in contrast to pigmented villonodular synovitis, which demonstrates low-signal intensity that is secondary to hemosiderin on both T1 and T2-weighted images. In most cases of lipoma arborescens, the lesion has grossly yellow-white villous proliferation. Microscopy reveals villi of different size, which are covered with layers of hyperplastic synovial cells with an accumulation of mature fat cells within the subsynovial compartment. Additionally, dilated capillaries and focal inflammatory infiltrates, composed mostly of lymphocytes and scattered plasma cells, can be observed. The recommended treatment for lipoma arborescens is open synovectomy. To the best of our knowledge, the use of arthroscopic synovectomy to treat lipoma arborescens was first reported by Sola and Wright in 1998. According to the literature, recurrence of the disease is uncommon. The young woman presented here had lipoma arborescens within the knee (a typical location). She had chronic joint effusion long before she was diagnosed and treated. By the time the lesion was treated, the patient had already developed degenerative changes within the articular cartilage. It is important to note that widespread use of MRI may improve detection of even minimally symptomatic forms of lipoma arborescens before degenerative changes occur. Because access to MRI evaluation can be limited in many locations, we recommend diagnostic arthroscopy with a biopsy in cases showing chronic effusion within the joint.
Reference: Jurkiewicz A, Krakowski P, Korolczuk A. Lipoma arborescens of the knee treated with arthroscopic synovectomy: a case report and review of the literature. JBJS Case Connector. 2012 Sep 26;2(3);e53.
Pigmented villonodular synovitis
Synovial lipoma
Synovial chondromatosis
Lipoma arborescens
Intra-articular lipoma

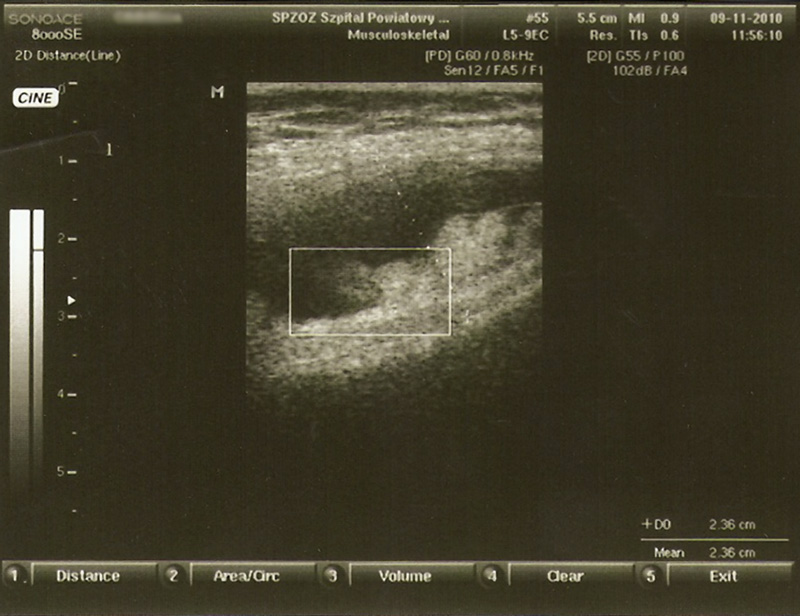


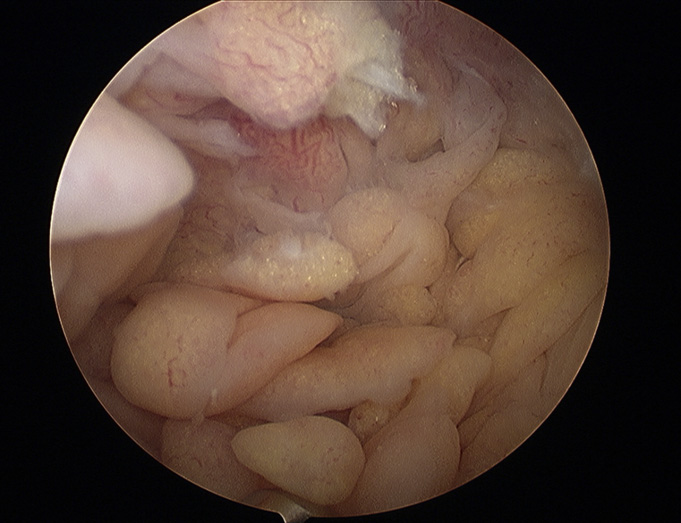
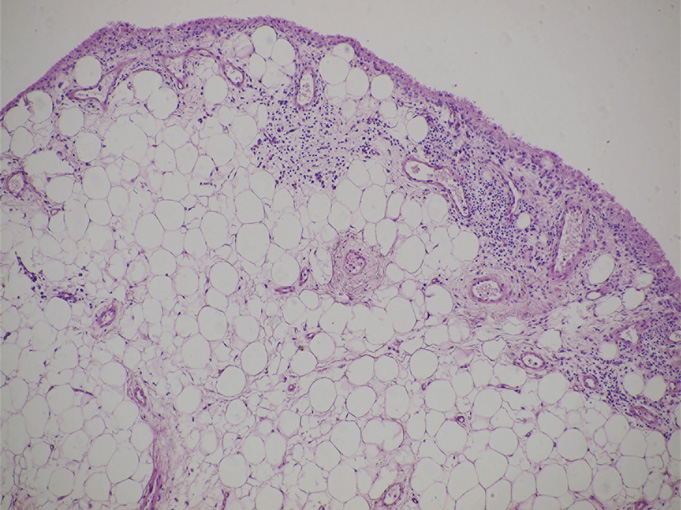
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4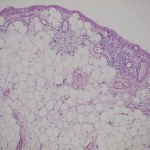 Fig. 5
Fig. 5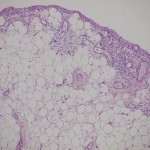 Fig. 5
Fig. 5