Forty-Year-Old Woman with Right Knee Pain for Four Months
February 6, 2013
A forty-year-old woman who had no history of trauma was seen with tenderness and effusion of four months’ duration in the right knee. She had also noted transient migratory arthralgias in the left knee and left foot during that time-period. However, the right knee was the only joint affected at the time of presentation. Her medical history included human immunodeficiency virus, diagnosed eleven years earlier; genital herpes simplex virus; polycystic kidney disease; and hypertension. The last CD4 count, three months earlier, was 104 (20%), and the human immunodeficiency viral load was 56,000 (decreased from >1,000,000 five months earlier). The knee was warm, with minimal erythema, moderate effusion, and generalized tenderness to palpation, especially at the suprapatellar area and the medial and lateral joint lines. The range of motion was 0 to 45, and there was pain at the extremes of extension and flexion. Aspiration of knee-joint fluid revealed 671 white blood cells, 13,310 red blood cells, and 71% neutrophils. No other joint was aspirated. The erythrocyte sedimentation rate was elevated to 102, the level of antinuclear antibodies was slightly elevated, and the rheumatoid factor was negative. Radiographs made three weeks earlier had revealed a suprapatellar effusion and soft-tissue swelling. A magnetic resonance image had then revealed soft-tissue edema along the posterior aspect of the knee, a moderate-sized joint effusion, and two focal areas within the joint, showing low signal on both T1 and long fast-spin-echo T2-weighted images (Fig. 1). A percutaneous synovial biopsy was performed six weeks after the knee aspiration. Staining of biopsy sections with hematoxylin and eosin showed fibrotic synovial tissue with numerous inflammatory cells, consisting predominantly of histiocytes, with a few plasma cells and lymphocytes (Figs. 2-A and 2-B). The histiocytes had a vacuolated cytoplasm, which contained ill-defined round-to-oval bodies. A Grocott stain highlighted these intracellular organisms, which measured approximately half the size of a red blood cell (2 to 4 m) (Figs. 2-C and 2-D).
The findings were consistent with a diagnosis of histoplasmosis. Concomitantly, a workup beginning four weeks after the first aspiration confirmed that the pulmonary histoplasmosis had recurred, and systemic antifungal therapy was begun. Knee-joint fluid obtained by repeat aspiration contained 45,300 red blood cells and 3500 nucleated cells, with 53% granulocytes, 22% lymphocytes, and 25% tissue cells. A mycology smear was negative, but culture was positive, with 1+ Histoplasma capsulatum. A Gram stain showed 4+ white blood cells and 4+ red blood cells; no organisms were seen. There was no growth on routine culture of joint fluid. While hospitalized, the patient received liposomal amphotericin B for seven days, and she was discharged with instructions to take oral itraconazole. At the time of her last visit, approximately eight months after the diagnosis of the knee infection, she was continuing to take oral itraconazole (300 mg/day). The knee had no effusion, and the range of motion was 0 to 130 without pain. A repeat magnetic resonance image demonstrated resolution of the previous inflammatory changes and a possible incidental small tear involving the anterior horn of the lateral meniscus. Plain radiographs showed a normal right knee. After having done well for a year, the patient had renewed swelling of the right knee. Cultures of specimens obtained with arthrocentesis were again positive for Histoplasma capsulatum. She received liposomal amphotericin B for eight days and continued to take oral itraconazole. The swelling of the right knee subsided, and, at the time of this writing, the infection was again quiescent.
Proceed to Discussion >>Reference: Weinberg JM, Ali R, Badve S, Pelker RR. Musculoskeletal histoplasmosis. A case report and review of the literature. J Bone Joint Surg Am. 2001 Nov;83(11):1718-22.
Although it is an opportunistic organism, histoplasmosis has been seen both in patients with the human immunodeficiency virus and in those without it. There have been sporadic findings of arthritis in patients with histoplasmosis even when no organisms were grown on culture of synovial fluid. Nightingale et al. reviewed the cases of 980 patients with acquired immunodeficiency syndrome who had disseminated histoplasmosis, but the authors did not mention whether there were findings of arthritis. Allen reported on two patients who had bone involvement with disseminated histoplasmosis, but no clinical evidence of joint involvement was noted in either patient. Class and Cascio reported on a patient who had histoplasmosis presenting as acute polyarthritis; they did not examine the joint fluid since they believed that the joint involvement was an allergic manifestation. Rosenthal et al. discussed the rheumatologic manifestations of histoplasmosis, which occurred in 6.3% of patients with symptomatic histoplasmosis diagnosed during an epidemic in Indianapolis. Cultures were negative for joint disease, and histologic studies did not reveal fungal organisms. Wheat et al. noted that, while cultures of specimens from patients who have chronic pulmonary and disseminated histoplasmosis are often positive, they are rarely positive in epidemics, when the disease is in an acute phase. Localized bone involvement may be seen in conjunction with a normal appearance of the joint space on radiographs; however, there may be atrophy of articular surfaces and secondary changes of surrounding bone. Darouiche et al. reported that histopathological examination of surgical specimens often revealed caseating and/or noncaseating granulomas. Cuellar et al. stated that Histoplasma may be detected in tissues or exudates in only 70% of cases and it takes two to three weeks for complement-fixation antibodies to histoplasmin and Histoplasma yeast antigens to become positive. The 1997 edition of The Medical Letter on Drugs and Therapeutics lists the drug of choice for histoplasmosis as itraconazole (200 mg orally, twice a day) or amphotericin B (0.5 to 0.6 mg/kg intravenously for four to twelve weeks). Amphotericin B is recommended for patients with severe illness. Alternative choices are ketoconazole (400 mg orally, once or twice a day) and fluconazole (400 mg, twice a day). Itraconazole (200 mg orally, once or twice a day) and amphotericin B (0.1 to 0.5 mg/kg intravenously, once a week) are listed as alternatives for chronic suppression in patients with human immunodeficiency virus. Wheat stated that patients with acquired immunodeficiency syndrome have a high rate of recurrence of disseminated histoplasmosis. He therefore thought that a high-dosage initial course of amphotericin is unwarranted. He suggested, as a general approach to the treatment of disseminated histoplasmosis, 1.0 to 1.5 g of amphotericin B over a six-to-eight-week period of induction therapy followed by ketoconazole (400 mg/day) or amphotericin B (50 to 100 mg/wk) over an indefinite maintenance period. He stated that ketoconazole cannot be recommended for immunocompromised patients because it is ineffective for them. In 1993, Drew extensively reviewed the pharmacotherapy for disseminated histoplasmosis in patients with acquired immunodeficiency syndrome. He concluded that amphotericin B is the drug of choice for induction therapy and that it should be followed by maintenance therapy with either amphotericin B or an oral azole antifungal agent that is active against Histoplasma capsulatum for the prevention of recurrence. Itraconazole may be used instead for both induction and maintenance treatment. In summary, histoplasmosis is an opportunistic fungal infection that is not commonly seen in patients who are not immunocompromised. The diagnosis should be considered in a patient with unexplained erythema, pain, and swelling in the knee. Radiographic findings may be inconclusive, and a biopsy is necessary. Treatment options include medical management with itraconazole or amphotericin B.
Reference: Weinberg JM, Ali R, Badve S, Pelker RR. Musculoskeletal histoplasmosis. A case report and review of the literature. J Bone Joint Surg Am. 2001 Nov;83(11):1718-22.
Pigmented villonodular synovitis
Histoplasmosis
Blastomycosis
Tuberculosis
Coccidioidomycosis


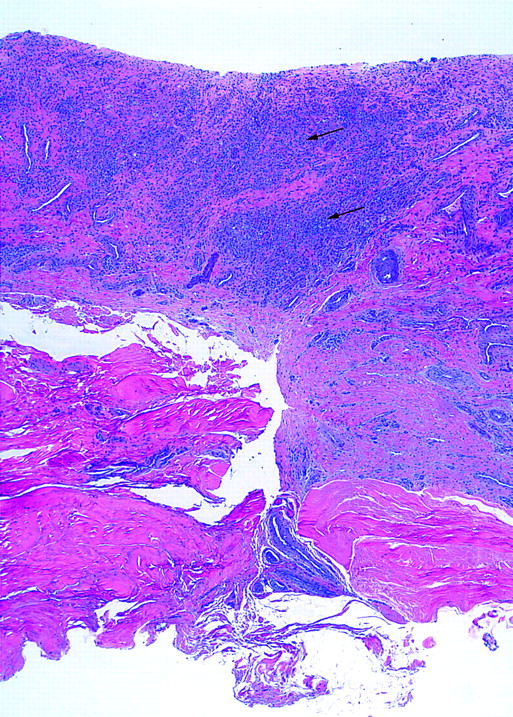
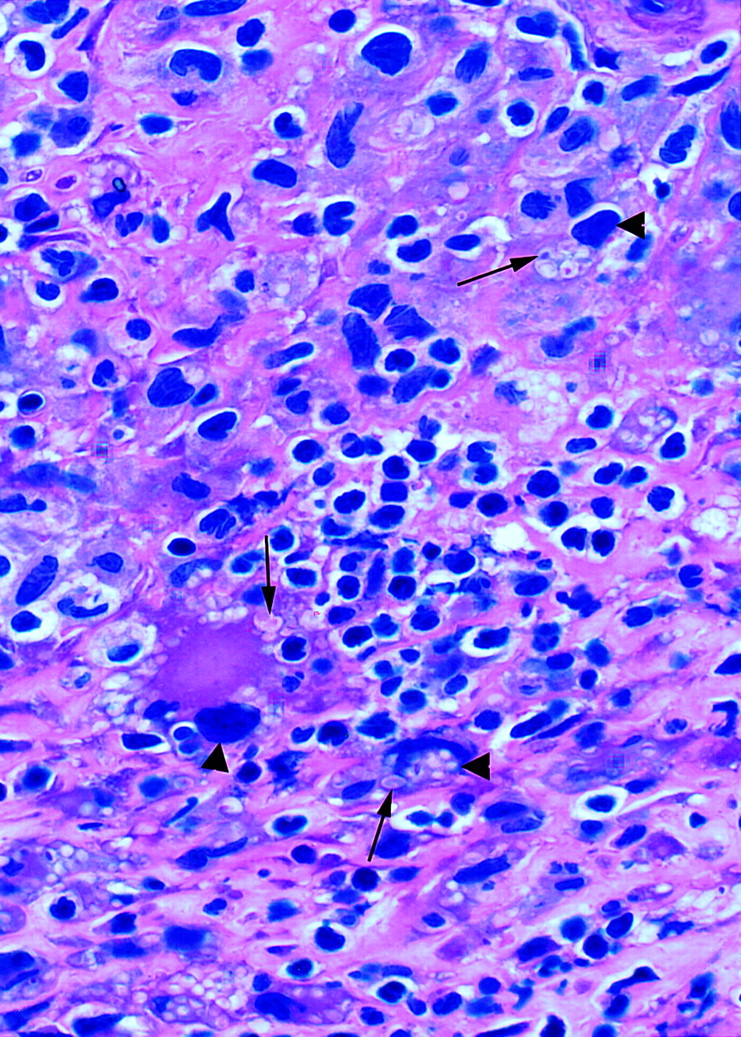
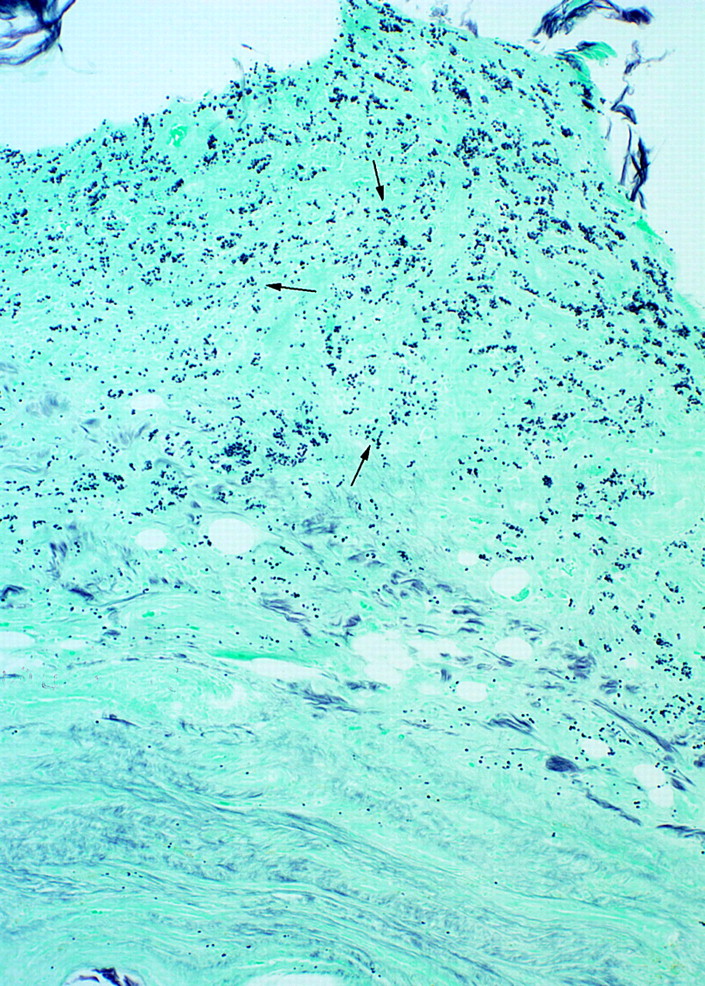

 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A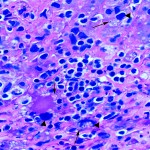 Fig. 2-B
Fig. 2-B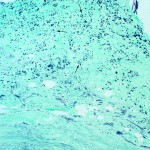 Fig. 2-C
Fig. 2-C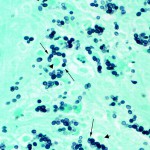 Fig. 2-D
Fig. 2-D