A Twelve-Year-Old Girl with Upper Back Pain for One Month
June 15, 2011
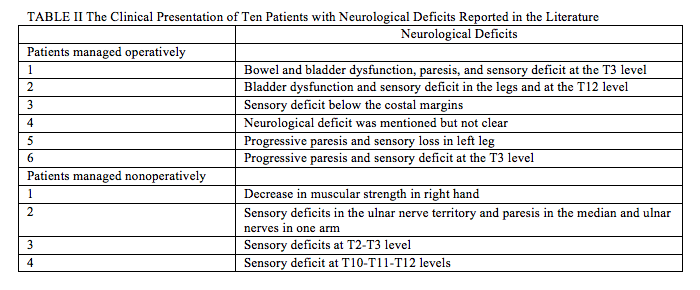
A twelve-year-old girl presented with upper back pain for one month, preceded by a fever forty days earlier. The pain radiated to the front of the chest, was aggravated by spinal motion, particularly bending forward and deep breathing, and was relieved by analgesics. She had tenderness at the spinous processes of T2 and T3 with paraspinal muscle spasm. Spinal motion was extremely painful. Neurological examination was unremarkable, except for a minimal sensory deficit of the left T2 and T3 dermatomes. During the febrile period, the serum calcium level was 2.74 mmol/L (normal, 2.29 to 2.73 mmol/L), the serum phosphorus level was 1.60 mmol/L (normal, 0.81 to 1.45 mmol/L), and the serum alkaline phosphatase level was 157 U/L (normal, 15 to 112 U/L). The erythrocyte sedimentation rate and leukocyte count were normal. The lateral radiograph of the cervical spine indicated a calcified disc at the T2-T3 level. A computed tomographic scan demonstrated a dense round mass centrally located within the disc space. Another dense oval mass was located eccentrically and occupied over half of the spinal canal (Figs. 1-A and 1-B). The occupying ratio of calcification was calculated as the ratio of the maximum anteroposterior thickness of calcification within the canal to the anteroposterior diameter of the spinal canal at the corresponding level as seen on the computed tomography scan. A giant herniated thoracic disc is defined as occupying >40% of the diameter of the spinal canal on the basis of a computed tomography scan or magnetic resonance imaging. The occupying ratio at the T2-T3 level in this patient was 74.5%. A T2-weighted magnetic resonance image revealed marked compression of the dural sac and spinal cord due to a large extradural mass of very low signal intensity at the T2-T3 level (Fig. 1-C).
The patient was initially treated with bed rest for three months and then was allowed to return to school six months later. The pain started to diminish slowly four weeks after presentation and disappeared completely in ten months. A computed tomography scan performed two months after the diagnosis revealed mild resorption of the calcification in the spinal canal, while the calcification within the intervertebral disc remained unchanged. The occupying ratio had decreased to 49.7% at this two-month mark. Six months later, the computed tomography scan revealed complete resolution of the calcification in the spinal canal and mild resorption of the calcification within the intervertebral disc (Fig. 2). Fourteen months later, the computed tomography scan revealed complete resolution of the calcification within the intervertebral disc (Fig. 3).
Proceed to Discussion >>Reference: Wu XD, Chen HJ, Yuan W, Tsai N, Wang XW, Zhou XH, Li H, Sheng XL, Xu SM. Giant calcified thoracic disc herniation in a child. A case report and review of the literature. J Bone Joint Surg Am. 2010:92;92:1992-6.
Intervertebral disc calcification in childhood is an uncommon, distinct disease of unknown cause. About 70% of the cases are located in the cervical spine, while thoracic calcifications account for approximately 20%. Radiographic evidence of disc herniation has been reported in approximately 38% of all patients with symptomatic intervertebral disc calcification in childhood. A herniated calcified disc in the thoracic spine is frequently associated with symptoms and neurological deficits. We reviewed the cases of twenty-one patients with thoracic intervertebral disc calcification, including our patient (Table I). There were fourteen boys and seven girls who ranged in age from one to thirteen years (mean [and standard deviation], 9.8 ± 3.2 years). Eighteen patients were symptomatic (including those with a fever), and three were asymptomatic. Radiographic evidence of herniation was present in fourteen patients (67%), ten of whom presented with neurological deficits and six of the ten underwent surgical treatment (Table II). In our patient, the herniated disc had an occupying ratio of >70%, which has been rarely reported in the radiographic findings in the prior literature. Nonoperative treatment is recommended for cases of calcified intervertebral disc herniation in children. Surgical decompression should be reserved for patients in whom there is persistent or progressive neurological compromise following an adequate course of conservative treatment. In our patient, the radiographic findings indicated severe compression of the thoracic spinal cord, but the patient had only mild unilateral radicular pain and sensory deficits in the T2 and T3 dermatomes. Therefore, nonoperative management was pursued. In a review of the literature, four of the six patients managed surgically presented with progressive paresis or dysfunction of the bowel or bladder and one patient had a severe sensory deficit plane below the costal margins. In the four patients with neurological deficits who were treated nonsurgically, sensory deficits and weakness in the hand muscles were the only neurological findings (Table II). This indicates that patients with mild neurological deficits, such as radiculopathy or myelopathy without motor deficits, can be treated with observation. Surgical management should be advocated for patients with progressive paresis or bowel or bladder dysfunction. The good prognosis for a herniated calcified disc centers on decompression of the spinal cord secondary to resolution of the calcification in the spinal canal. In our patient, resorption was detected in the calcification in the spinal canal during the first two months, as indicated by a decrease in the occupying ratio from 74.5% to 49.7%. Because of total radiation dosage, magnetic resonance imaging rather than computed tomography might be a better way to obtain follow-up in these patients. We suggest that, during the initial course of observation, the occupying ratio should be monitored periodically to identify resorption of the calcification in the spinal canal, as a decreasing ratio is associated with a good prognosis. However, a persistent or increasing ratio might result in deterioration of neurological function and require surgical decompression. Complete resorption usually takes months to years, although rarely has the exact process of resorption been documented. In our patient, the calcified disc split into two fragments: a large fragment prolapsed into the spinal canal, and the other one remained in the intervertebral disc space. Resorption of the calcification in the spinal canal proceeded earlier and faster than that in the intervertebral disc space. In our review of the literature, a similar phenomenon was observed by Mellion et al. and Bagatur et al. in two patients who were managed nonoperatively and by Sato et al. in a report on one patient who was managed operatively. Resorption of the intervertebral calcification may be facilitated by the presence of vascular channels in the cartilage plates. The abundant vascular supply at the posterior aspect of the vertebra including the epidural vascular plexus may contribute to the faster resorption rate of the herniated calcification. The etiology of intervertebral disc calcification in children remains unclear. Tissue calcification is related to necrosis because of insufficient blood supply or a metabolic disorder. The interruption of blood supply could be secondary to trauma, infection, inflammation, or vasculitis. Our patient had an antecedent history of an upper respiratory tract infection and fever. Laboratory results showed a normal erythrocyte sedimentation rate and leukocyte count. Bacterial discitis is an unlikely cause as no disc space narrowing or end-plate destruction was noted in the previous reports. In addition, the use of antibiotics does not appear to facilitate resolution. Some metabolic disturbance may have been present in our patient, as a mild increase in serum calcium, phosphate, and alkaline phosphatase concentrations was detected. Hypercalcemia and hyperphosphatemia play an important role in the occurrence of soft-tissue calcification, and alkaline phosphatase can cleave pyrophosphate, an important inhibitor of calcification. The case of our patient demonstrates that a giant herniation of a calcified disc in the thoracic spine of a child, without major neurological deficits, can be treated nonoperatively. Monitoring the occupying ratio on computed tomography or magnetic resonance imaging is beneficial to evaluate the progress of resorption and to determine subsequent treatment needs.
Reference: Wu XD, Chen HJ, Yuan W, Tsai N, Wang XW, Zhou XH, Li H, Sheng XL, Xu SM. Giant calcified thoracic disc herniation in a child. A case report and review of the literature. J Bone Joint Surg Am. 2010:92;92:1992-6.
Anterior discectomy at T2-T3 and anterior spinal fusion T1-T4
Intradiscal injection of corticosteroids
Nonoperative management with activity limitation
Posterior spinal fusion from T1 to T4 with discectomy using costotransversectomy approach


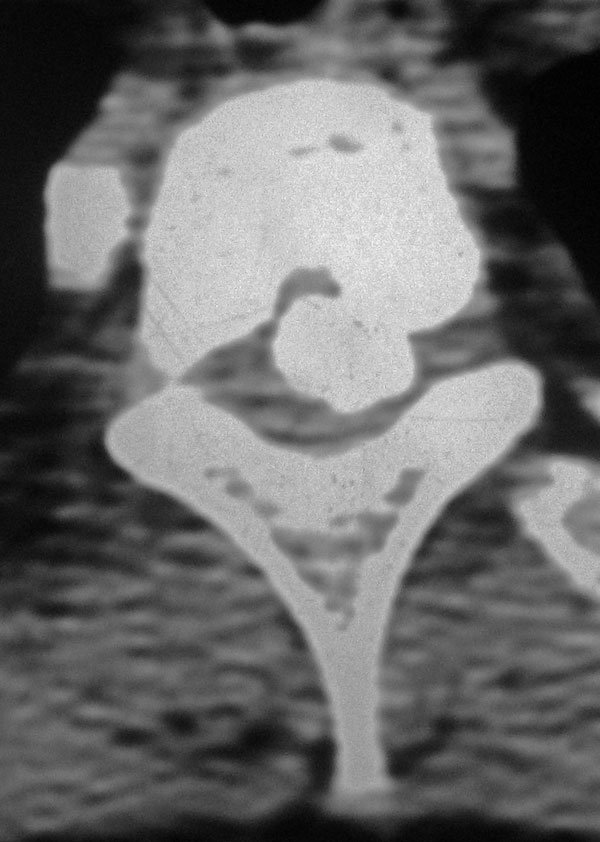
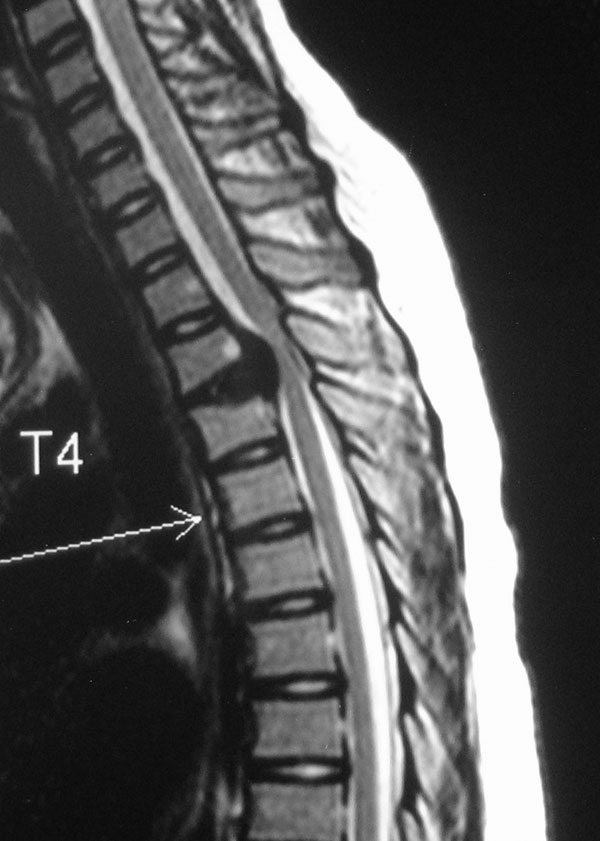
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B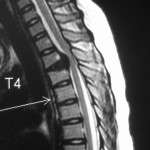 Fig. 1-C
Fig. 1-C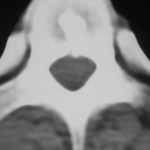 Fig. 2
Fig. 2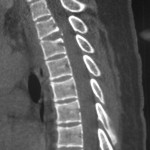 Fig. 3
Fig. 3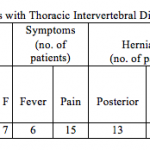 Table I
Table I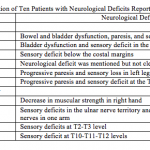 Table II
Table II