An Eighteen-Year-Old Female Athlete with Knee Pain
March 16, 2011
An eighteen-year-old female athlete who played floorball (a popular European team sport that is a variant of floor hockey) presented with chronic anterior knee pain that had begun a few months previously without any specific injury event. She was an international-level athlete, and her training had become more difficult because of the persistent anterior knee pain, but she continued to exercise at a reduced intensity. At the first visit to an orthopaedic surgeon, radiographs were interpreted as normal and clinical examination revealed no specific findings other than anterior knee pain with some tenderness of the patella. She was diagnosed with nonspecific anterior knee pain. A radiograph made one year previously showed a normal patella (Fig. 1). An axial T1-weighted magnetic resonance imaging sequence revealed a line of low signal intensity (Fig. 2-A), and a sagittal fat-saturation sequence showed surrounding bone edema (Fig. 2-B). Five months later, because of persistent substantial anterior knee pain, she presented to another orthopaedic surgeon, and additional magnetic resonance images and radiographs of the knee were obtained. The new axial proton density fat-saturation magnetic resonance image is shown (Fig. 3).
The patient was diagnosed with a displaced longitudinal patellar stress fracture. Displacement of the stress fracture had apparently occurred as a result of continued training. The knee was considered to be otherwise normal; the magnetic resonance imaging revealed no other pathologic findings. The tibial tubercle-to-trochlear groove distance was 16 mm (mean normal value, 12.7 ± 3.4 mm), indicating a possible slight increase in the Q angle in this knee. Because of the large fracture size (13 × 27 mm and 30% of the lateral patellar articular facet), open reduction was performed with bioabsorbable cross-pin fixation (Inion OTPS; Inion, Tampere, Finland). Over the next five months, the fracture was redisplaced and the patient underwent a secondary open reduction and internal fixation with use of 4.0-mm cannulated screws (Synthes, West Chester, Pennsylvania) with a lag-screw technique (Fig. 4). Postoperative care included six weeks of knee brace protection with flexion restricted to 90°, after which full flexion was allowed. The patient was allowed to return to training six months after the second operation, and at twelve months she regained her preinjury activity level and began competing again in floorball at the national level. Before she returned to competition, the lag screws were removed because of soft-tissue irritation. Since then, she has not reported any subsequent symptoms.
Proceed to Discussion >>Reference: Sillanpää PJ, Paakkala A, Paakkala T, Mäenpää H, Toivanen J. Displaced longitudinal stress fracture of the patella. A case report. J Bone Joint Surg Am. 2010; 92:2344-7.
Stress fractures typically occur in athletes or physically active individuals who participate in strenuous repetitive physical activities without allowing adequate adaptation of the bone to the stress forces. Patellar stress fractures appear to be quite rare, but our ability to make the diagnosis in daily practice may also be poor. In fact, in the present case, nonsurgical care with rest might have been adequate treatment had the line of low signal intensity not been missed on the original magnetic resonance images. Transverse patellar stress fractures are well described in the literature, and displacement is considered to be an indication for open reduction and internal fixation. Many different sports activities have been described as causes of a transverse patellar stress fracture. In the present case, repetitive pivoting stress forces across the knee joint related to participation in floorball may have predisposed the patient to extensive lateralizing forces of the patella and subsequently to displacement of the vertical stress fracture. We could not determine a specific traumatic event that might have caused displacement of the stress fracture, and we concluded that the medial restraints, including the medial patellofemoral ligament, had remained intact. If the medial restraints of the patella had been loose, the patient would have had difficulties with patellar instability and the lateralizing forces would have produced a dislocated or subluxated patella. Because the medial restraints remained intact, the lateralizing forces created the longitudinal stress fracture. To our knowledge, four cases of longitudinal patellar stress fractures have been reported in the English-language literature; three occurred in children, were nondisplaced, and were treated successfully with conservative means. One fracture in an adult was treated by excision of the small fracture fragment. Because the knee is a common site of overuse injuries such as patellar tendinitis, patellofemoral pain syndrome, patellar subluxation, and unspecified anterior knee pain, a longitudinal patellar stress fracture may be an underlying cause of prolonged anterior knee pain and could go undetected on radiographs if it is not displaced. Therefore, we recommend that patients with persistent anterior knee pain and palpable patellar tenderness undergo magnetic resonance imaging if radiographs and clinical examination do not provide evidence of a cause of the prolonged pain. Treatment options for a longitudinal patellar stress fracture should first include nonsurgical management with rest, which will likely be successful for the majority of nondisplaced fractures. Use of a patellar support or brace for a few weeks after the diagnosis should be considered to minimize the risk of fracture displacement and to help relieve pain. Controlled closed-chain quadriceps exercises with a brace may be performed initially, if the pain is tolerable. Our patient had symptoms over a long period, and eventually the fracture line became displaced, most likely because the patient exercised forcefully after the initial missed diagnosis. Open reduction and internal fixation may be required if the fracture is displaced. Our patient first underwent internal fixation with bioabsorbable pins, but the fracture did not heal and it redisplaced five months after that operation. Because of this experience, we recommend fixing displaced vertical patellar stress fractures with screws that can apply compression across the fracture line to enhance fracture-healing. With rigid fixation, the patient may begin passive mobilization immediately and controlled quadriceps exercises within a few weeks after surgery. We recommended a four to six-month break from athletic participation and that healing of the fracture line be visible on radiographs before the patient is allowed to resume participation in sports. Here, we presented a case of a displaced longitudinal patellar stress fracture, which, although rare, should be suspected in physically active patients with persistent anterior knee pain. We suggest careful clinical assessment of these patients and recommend magnetic resonance imaging for cases of persistent nonspecific anterior knee pain with palpable patellar tenderness. Activity restriction may permit healing of nondisplaced fractures. On the basis of this unique case, we suggest open reduction and internal screw fixation for the management of a displaced longitudinal stress fracture of the patella with a large lateral fracture fragment.
Reference: Sillanpää PJ, Paakkala A, Paakkala T, Mäenpää H, Toivanen J. Displaced longitudinal stress fracture of the patella. A case report. J Bone Joint Surg Am. 2010; 92:2344-7.
Bipartite patella with stress reaction
Longitudinal stress fracture of the patella
Lateral patellar fracture due to recurrent subluxation
Osteoid osteoma of the lateral aspect of the patella

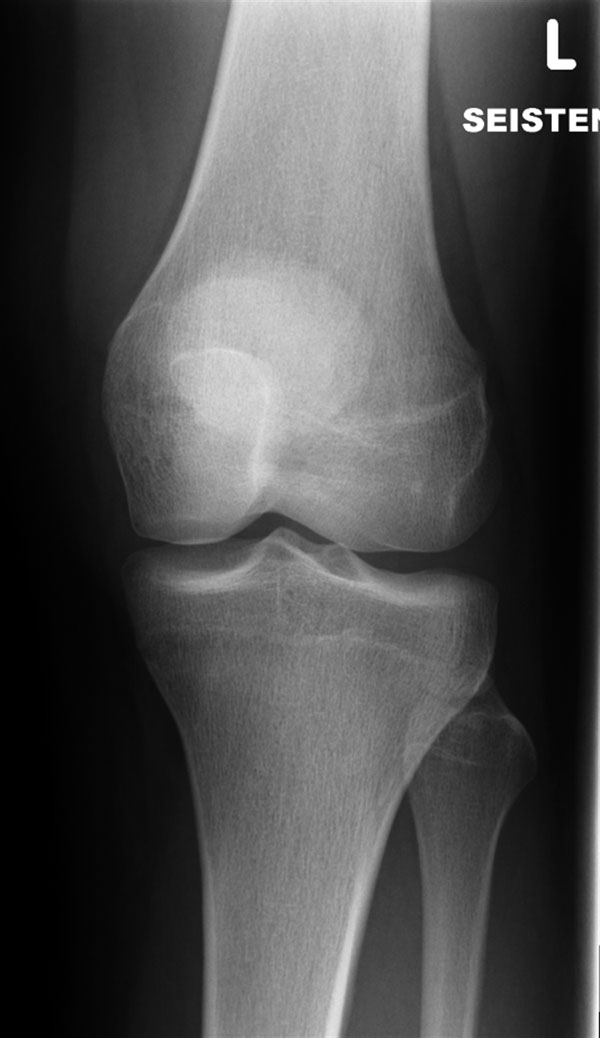
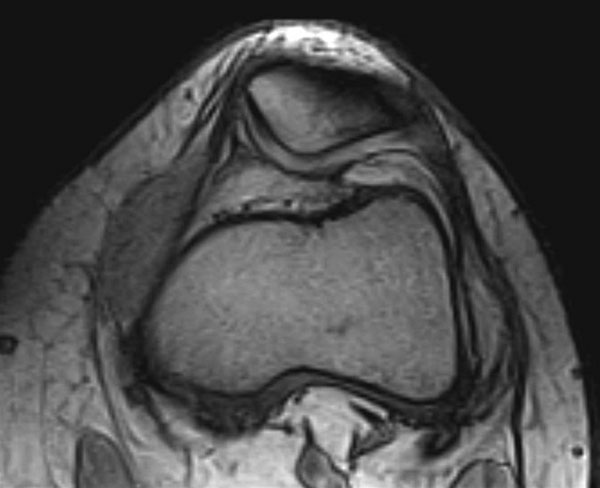
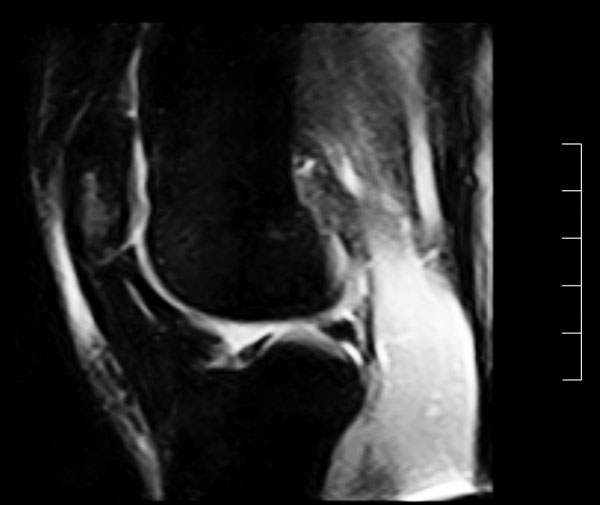
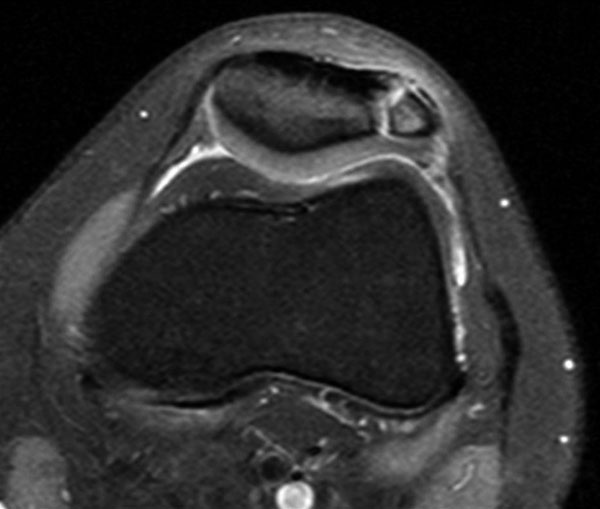
 Fig. 1
Fig. 1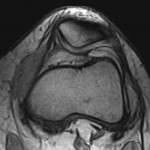 Fig. 2-A
Fig. 2-A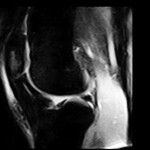 Fig. 2-B
Fig. 2-B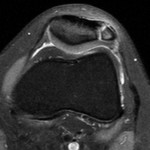 Fig. 3
Fig. 3 Fig. 4
Fig. 4