A Twenty-two-Year-Old Man with a Wrist Injury Following a Car Accident
April 20, 2016
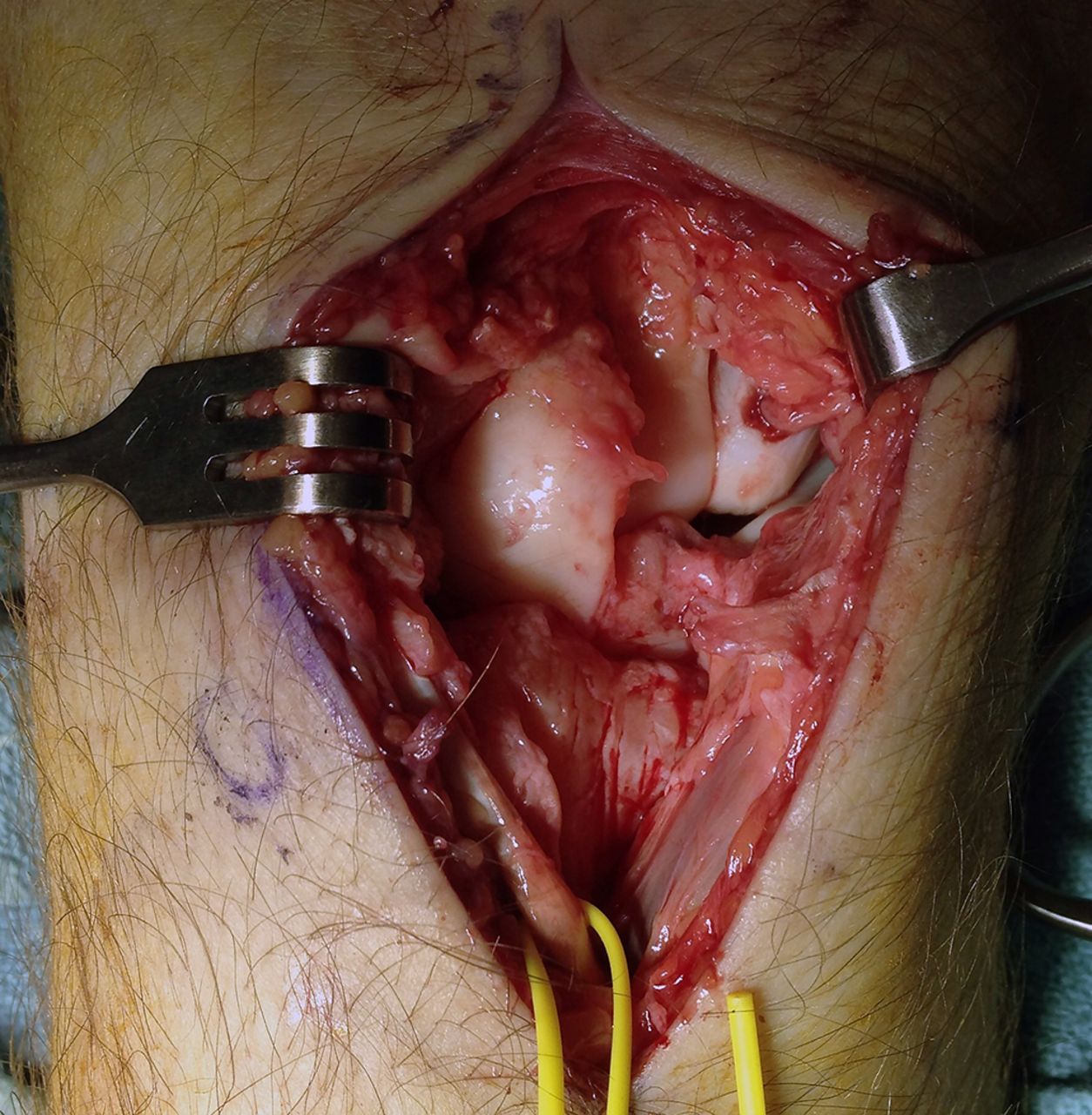
A twenty-two-year-old, right-hand-dominant male patient presented to our trauma center after being involved in a motor-vehicle accident. He was hemodynamically stable with a Glasgow Coma Scale (GCS) score of 15. He was diagnosed with multiple injuries, including a left subtrochanteric femoral fracture; a closed, complex fracture-dislocation of the right ankle; a right lateral process talar fracture with disruption of collateral ankle ligaments; an anteroposterior compression (APC) type-II pelvic ring injury with slight pubic symphysis diastasis; dislocation of the right sacroiliac joint; a sternum fracture; multiple right-side rib fractures associated with a right pneumothorax; liver laceration; subdural hematoma; and a ligamentous injury to the right wrist. Radiographs demonstrated a wrist injury (Fig. 1). This was further elucidated on a computed tomography (CT) scan (Fig. 2). Neurovascular examination was unremarkable. He was brought to the operating room urgently on the day of his injury for emergency stabilization of the femoral fracture and closed reduction of the contralateral ankle and the wrist dislocation. The following day, he underwent open reduction and internal fixation (ORIF) of the pelvic ring, ankle, and talus. Two days after the initial injury, the wrist injury was definitively treated surgically.
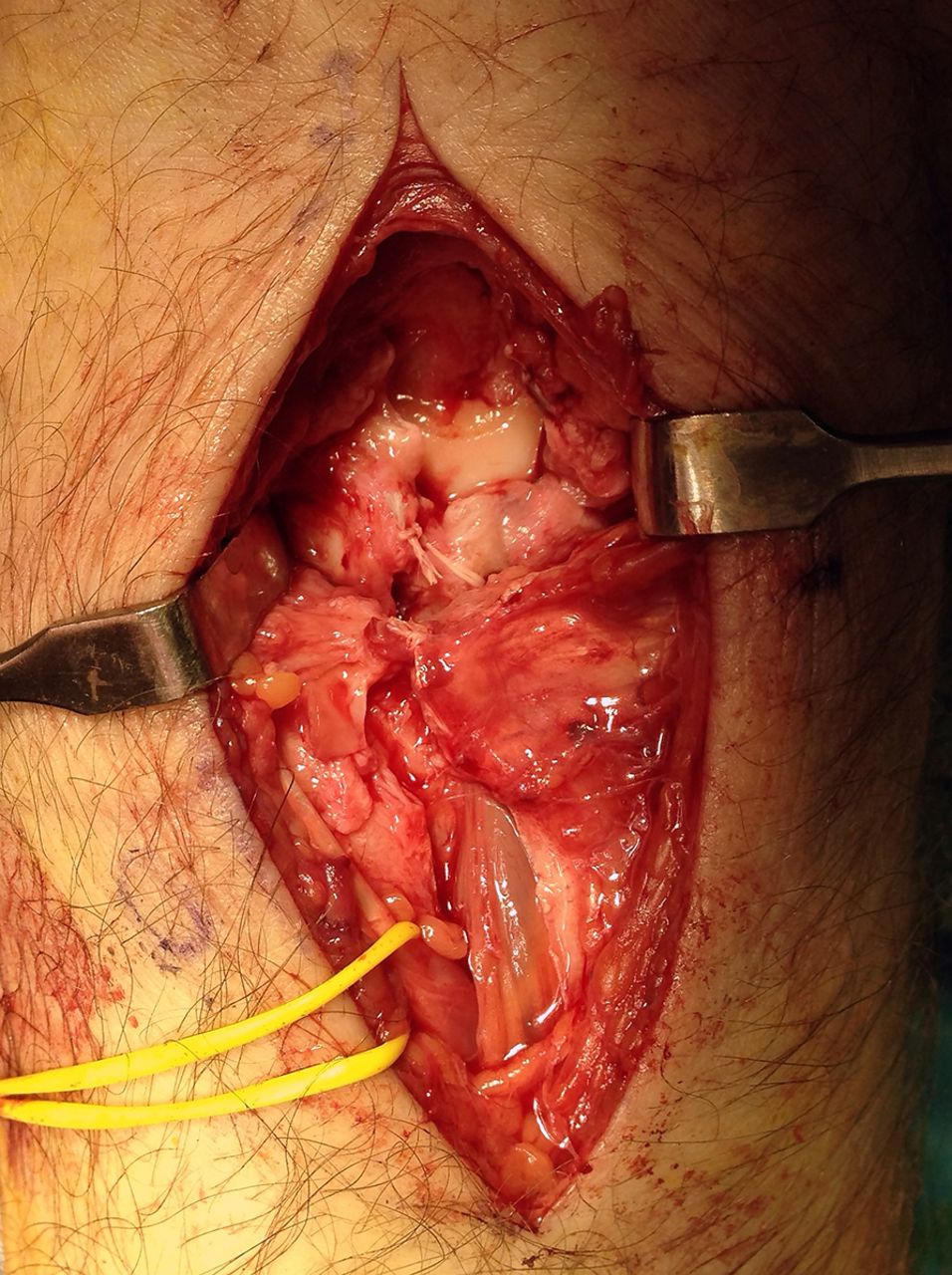
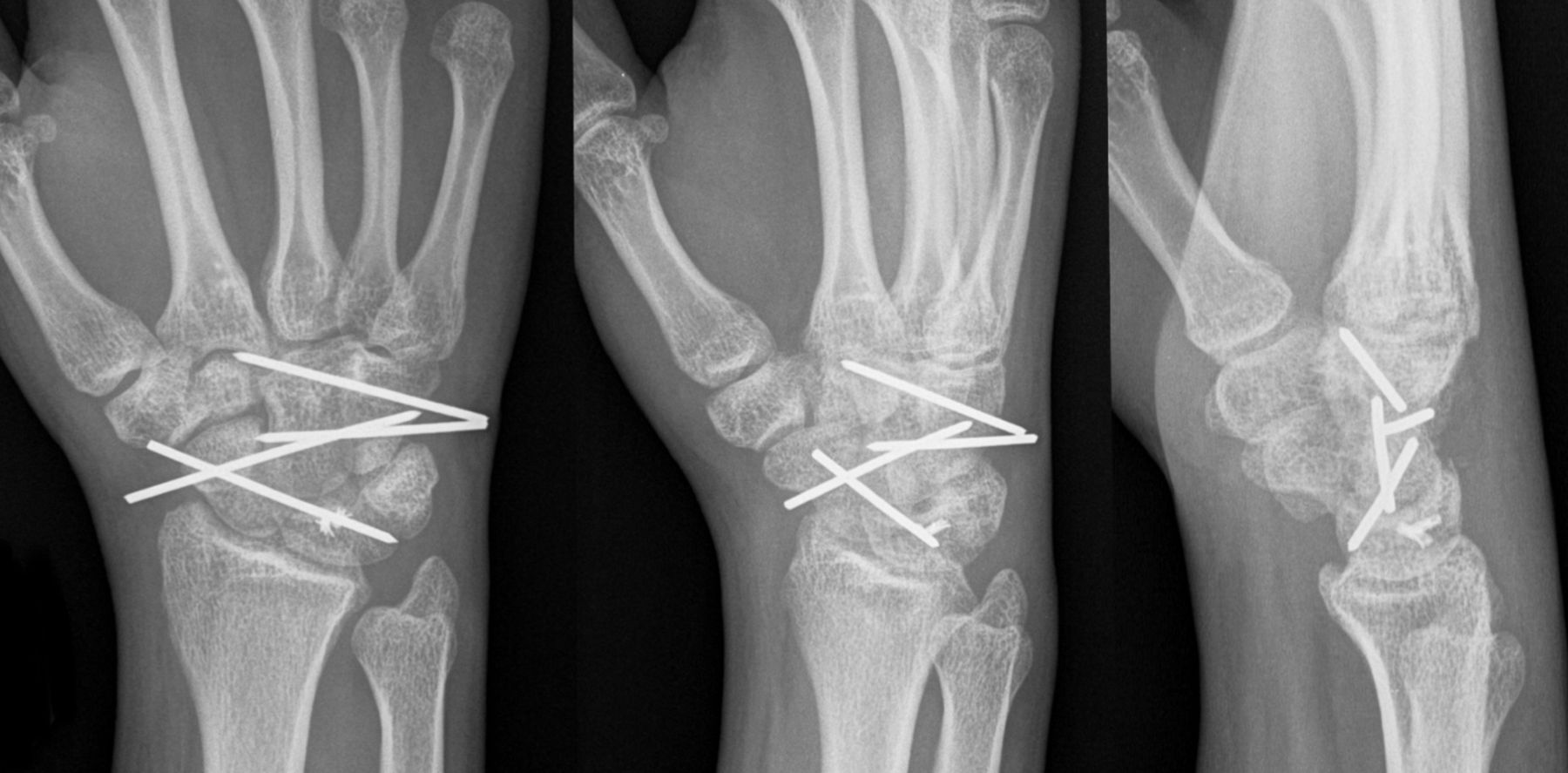
The patient was diagnosed with a volar dislocation of the hamate with a scapholunate dissociation. The carpus was carefully accessed via a dorsal approach through the interval between the third and fourth dorsal compartments. Extensor indicis and communis tendons were elevated and reflected ulnarly, and an arthrotomy was performed (Figs. 3-A, 3-B, and 3-C). The scapholunate ligament was found to be avulsed from the lunate circumferentially. The scaphoid had a substantial flexion deformity, and there was a large gap in the scapholunate interval. The hamate was dislocated volarly and easily reduced with direct, dorsally directed pressure on the hook of the hamate. Percutaneous Kirschner wires (1.6 mm) were inserted from the hamate to the capitate to maintain the reduction. The scapholunate ligament injury was repaired with the use of two Mitek mini suture anchors (DePuy Mitek, Raynham, Massachusetts) that were placed into the lunate in the region of the ligament avulsion. The 2-0 TiCron sutures (Covidien, Dublin, Ireland) from the suture anchors were passed through the remainder of the scapholunate ligament attached to the scaphoid. The scapholunate joint was then reduced and held in place with Kirschner wires (1.6 mm), and the sutures were tied. The alignment of the carpus and the position of the Kirschner wires were confirmed with use of fluoroscopy, and the Kirschner wires were cut and buried beneath the skin (Fig. 4). The wound was irrigated, and the capsule and dorsal retinaculum, followed by the skin and subcutaneous tissues, were closed with interrupted sutures. A thumb spica splint was then applied.
The patient returned to have the sutures removed at two weeks postoperatively but remained in a splint for six weeks. The Kirschner wires were removed in the clinic with use of local anesthetic at twelve weeks postoperatively, and subsequently, the patient began a physiotherapy program to regain range of motion. At one year of follow-up, he had no pain or functional limitations with respect to the wrist. His active range of motion was 40° of wrist flexion, 30° of wrist extension, and supination and pronation equal to those of the contralateral, uninjured wrist. Radiographs indicated anatomical maintenance of the hamate relocation, restoration of a near-normal scapholunate interval, and minimal increase in the scapholunate angle on the lateral projection image (Fig. 5); no arthritis was noted.
Proceed to Discussion >>Reference: Walmsley D, Dhotar H, Geddes C, Axelrod T. Combined volar hamate dislocation and scapholunate ligament rupture: a case report. JBJS Case Connect. 2015 Apr 22; 5(2):e33.
The majority of cases of hamate dislocation that have been reported in the literature were treated by ORIF, with others treated by closed reduction and Kirschner-wire fixation, conservative treatment, or hamate excision. Irrespective of treatment, most patients end up with loss of extension and reduced grip strength compared with that of the uninjured side. A proposed mechanism for hamate dislocation involves direct impact on the hook of the hamate when there is dorsal support of the capitate, rupturing the ligaments around the hamate as the transverse carpal ligament pulls the hamate volarly.
Disruption of the scapholunate ligament is the most frequent cause of carpal instability. The dorsal component of the scapholunate ligament is the thickest, strongest, and most important of the scapholunate stabilizers, acting as the primary restraint to distraction, torsional, and translational forces. Scapholunate dissociation requires more than only scapholunate ligament disruption; it also requires disruption of the radioscapholunate and radiocapitolunate ligaments to appreciate changes in carpal position radiographically. The mechanism of injury is thought to be a sudden impact applied to the hypothenar region with the wrist in a position of extension, ulnar deviation, and supination, driving the capitate between the scaphoid and lunate.
Treatment of acute scapholunate ligament injuries through a dorsal approach for open reduction and use of a Mitek mini anchor for direct ligament repair was reported to have achieved good or excellent results in sixteen out of eighteen patients at an average duration of follow-up of thirty-two months postoperatively. Of note, 50% of these injuries were associated with other carpal injuries. Surgical repair of scapholunate ligament injuries has been shown to restore radiolunate contact pressure to within normal values.
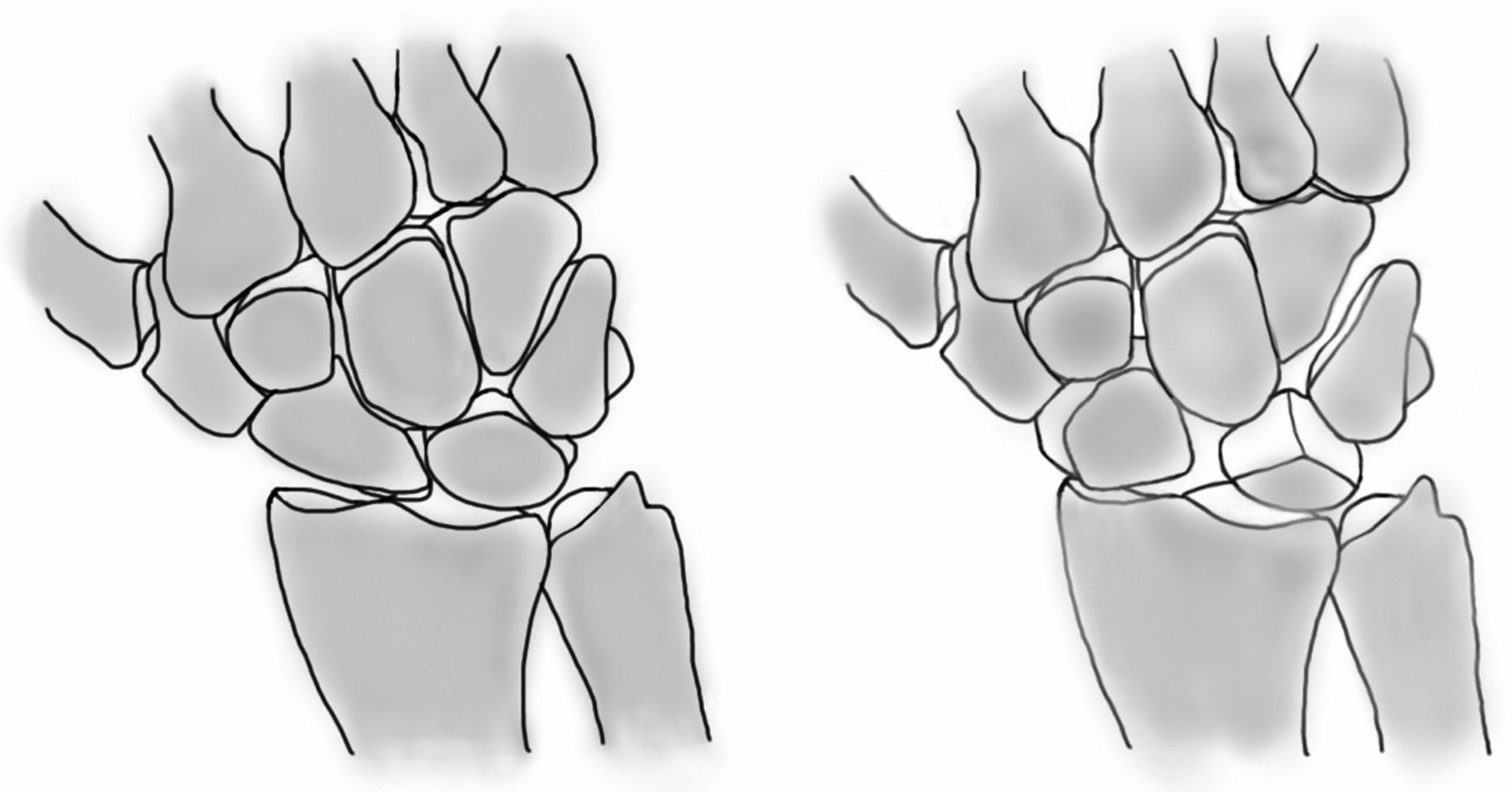
The present case report highlights the need for meticulous review of radiographs and for having a low threshold for acquiring CT imaging to further assess for associated carpal injuries. This injury pattern may represent a variant in the spectrum of perilunate dislocations, with the force passing through the scapholunate interval and space of Poirier (the lunocapitate interval) and exiting through the proximal row adjacent to the hamate, resulting in a volar hamate dislocation in association with the scapholunate dissociation (Fig. 6). Successful surgical treatment for this injury pattern may be performed dorsally via direct reduction and repair of the scapholunate ligament with percutaneous pinning of the affected carpal bones.
Reference: Walmsley D, Dhotar H, Geddes C, Axelrod T. Combined volar hamate dislocation and scapholunate ligament rupture: a case report. JBJS Case Connect. 2015 Apr 22; 5(2):e33.
What is the diagnosis?
Scaphoid fracture-dislocation
Capitate fracture or midcarpal dislocation
Scapholunate ligament disruption
Volar dislocation of the hamate with a scapholunate dissociation
Pisiform or hamate dislocation


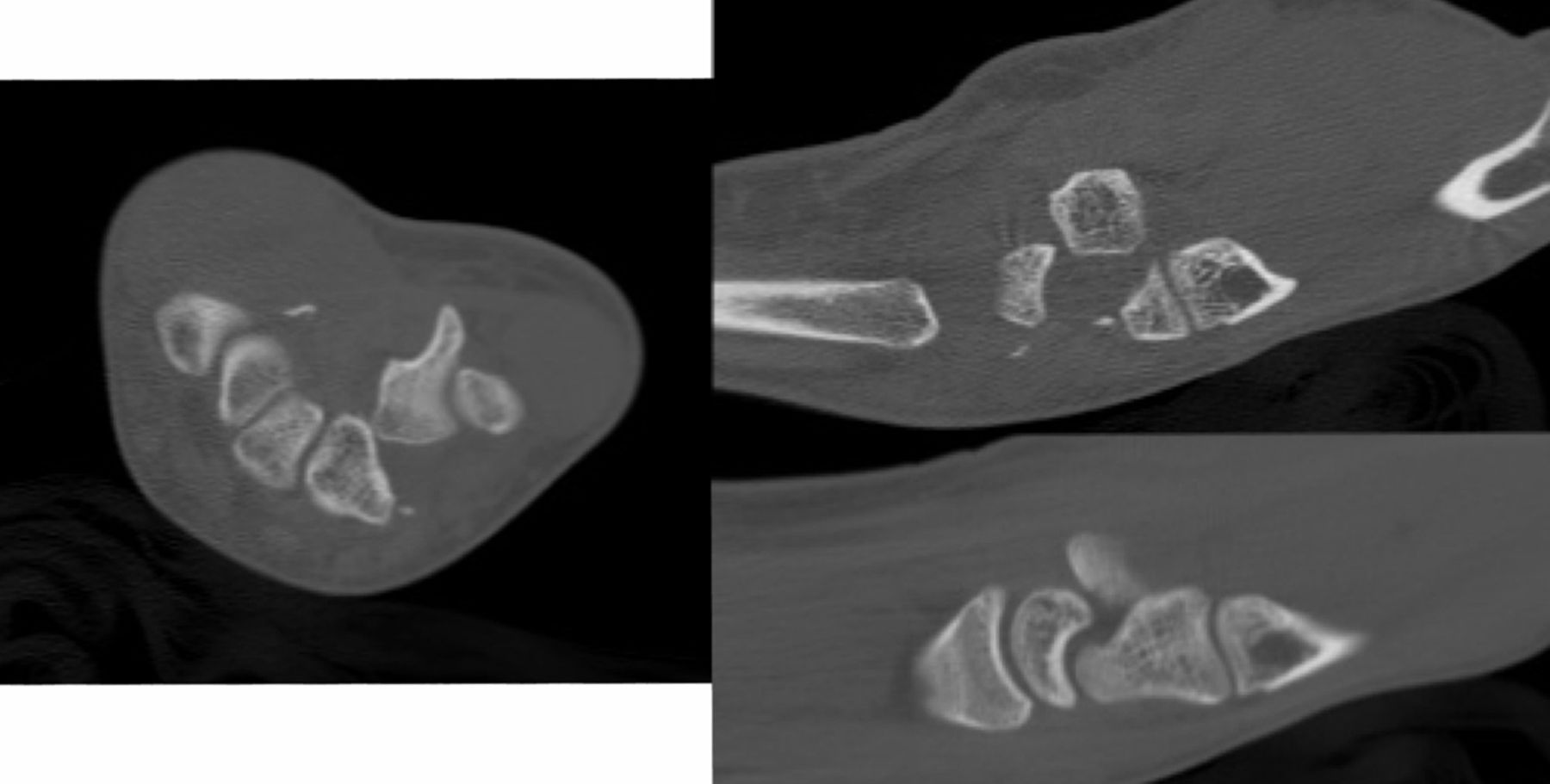
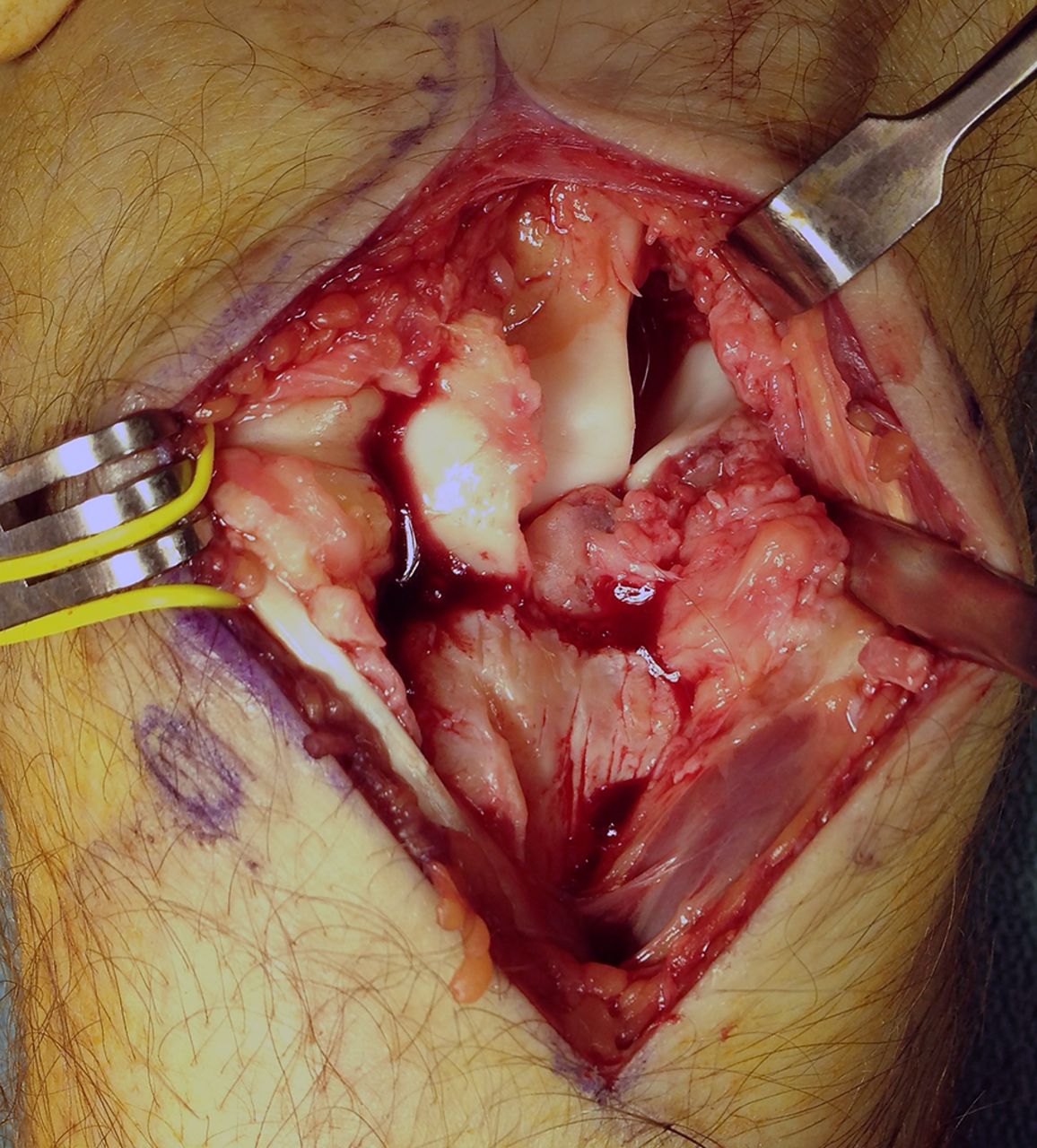
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 3-C
Fig. 3-C Fig. 4
Fig. 4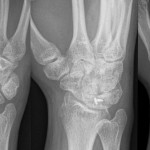 Fig. 5
Fig. 5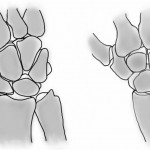 Fig. 6
Fig. 6