A 51-Year-Old Runner with Acute Hip and Groin Pain
June 1, 2016
The patient was an active fifty-one-year-old woman who, prior to the injury, ran approximately 40 mi (64.4 km) per week. The medical history was notable for hypothyroidism, which was being treated with levothyroxine, and the surgical history was notable for arthroscopic rotator cuff repair and hysterectomy with ovariectomy.
The patient had no symptoms until she experienced an acute onset of right posterior buttock pain during a run. The symptoms did not improve, and she consulted her primary care physician approximately six weeks later. Radiographs that were made at that time (Fig. 1), and physical therapy was prescribed, without improvement. Four months after the injury, the patient was referred to a sports-medicine specialist as well as a physiatrist, and a subsequent magnetic resonance imaging (MRI) scan was obtained (Fig. 2). The patient had previously curtailed her running because of pain, but by this time she had stopped all running activity. Over the ensuing months, the symptoms did not improve. Ten months after the beginning of the symptoms, the patient was referred to our clinic for evaluation.
At the time of presentation to our clinic, the patient described moderate-to-severe pain in the right posterior buttock area. She was unable to sit for any length of time because of pain in this location. She also had pain with walking and activities of daily living. The symptoms had not improved with anti-inflammatory drugs or activity modification, including the cessation of all running activity. Physical examination revealed a fit appearance, with a body mass index (BMI) of 22 kg/m. The pain was reproducible with palpation of the ischium posteriorly via the buttocks. The remainder of the physical examination was unremarkable. Laboratory studies were negative for metabolic abnormality, with normal levels of 25-OH vitamin D, free thyroxine (T4), hemoglobin A1c, electrolytes, and parathyroid hormone. Radiographs were notable for callus formation in the inferior pubic ramus (Fig. 3), and a bone scan revealed focally increased uptake at this location (Fig. 4). The patient was counseled regarding the options for treatment, including continued conservative management and surgical stabilization.
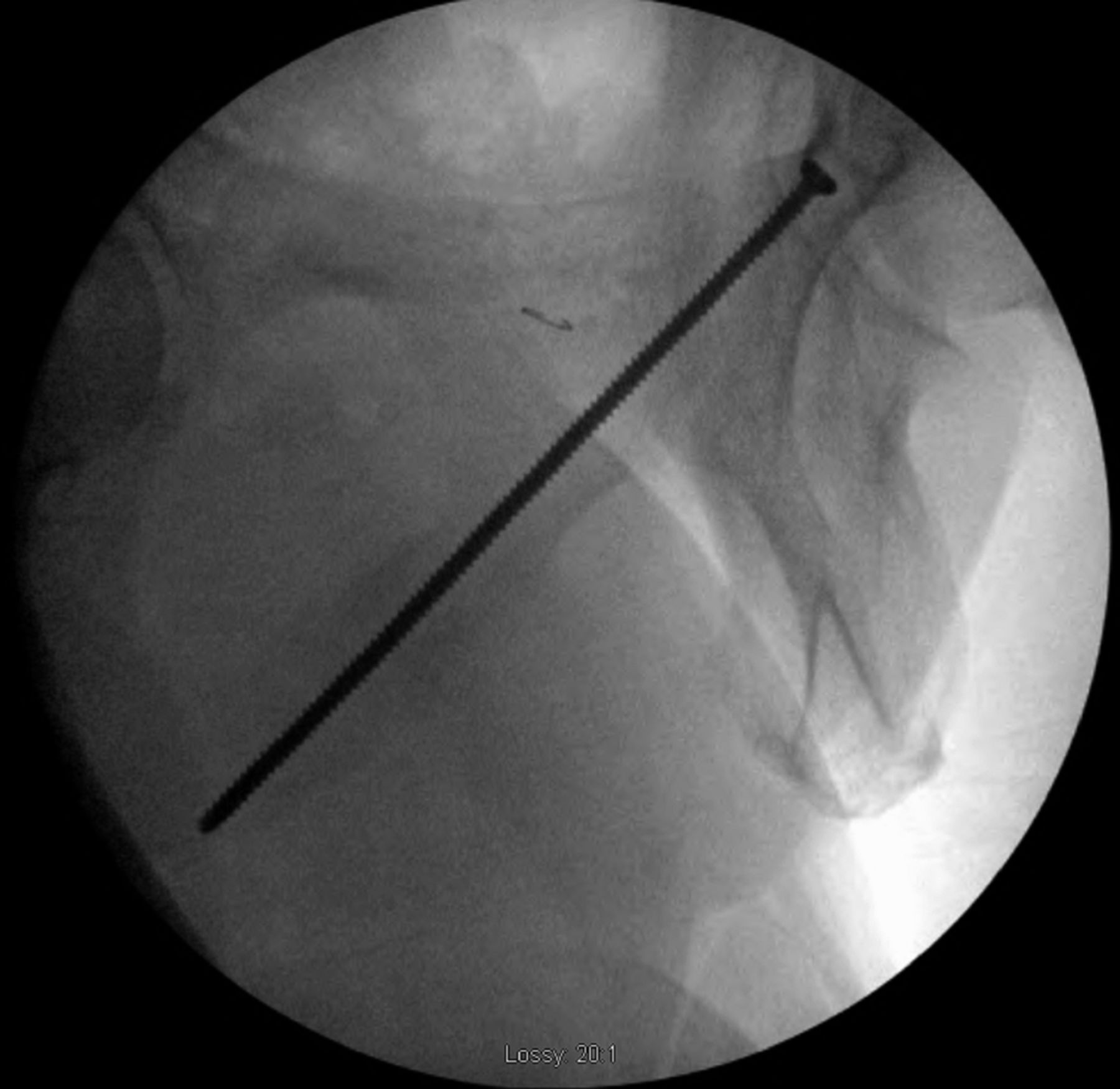
After eleven months of symptoms and ten months of conservative treatment, including four months of complete avoidance of all running activities, the patient elected to undergo surgical fixation for symptomatic and functional reasons. Following the induction of general anesthesia, the patient was positioned supine on the radiolucent table and a urinary catheter was placed to decompress the bladder. The operative site was prepared and draped in the standard sterile fashion. A small stab incision was made over the contralateral (left) superior pubic ramus because of the planned trajectory of the screw, and a 2.5-mm drill was directed across the nonunion site. We then placed a 3.5-mm cortical screw with a length of 115 mm. The screw was fully inserted so that it was flush with the contralateral (left) pubic ramus. We considered advancing the screw through the contralateral pubic ramus down to the operative (right) pubic ramus to avoid leaving a screw that crossed the symphysis, but we ultimately elected not to do so given concerns regarding the placement of a large channel through the contralateral pubic ramus as well as the difficulty of screw removal should it ever become necessary. Fluoroscopy was utilized for this purpose, including the obturator outlet and inlet views (Figs. 5-A and 5-B). Postoperative radiographs demonstrated appropriate screw placement across the stress fracture nonunion (Fig. 6).
The patient reported immediate relief of symptoms, including when sitting and walking, and was discharged from the hospital on the first postoperative day. She was allowed to bear full weight immediately after surgery and returned to her job as a waitress at four weeks postoperatively. At six weeks postoperatively, she had returned to walking 35 mi (56.3 km) per week without symptoms. She was allowed to return to running at twelve weeks postoperatively and was able to do so without pain. At the time of latest follow-up, at sixteen months postoperatively, the patient had returned to all of her previous activities without limitation, and radiographs demonstrated a healed fracture (Fig. 7).
Proceed to Discussion >>Reference: Okike K, Moritz BE. Minimally invasive screw fixation of inferior pubic ramus stress fracture nonunion in a runner: A case report. JBJS Case Connect. 2016 Apr 13;6(2):e26.
While stress fractures are a common injury in runners, the pelvis is an uncommon site. Previous reports of inferior pubic ramus stress fracture have been limited to small series of runners and military personnel. In those reports, conservative treatment (focusing on avoidance of the offending activity) was usually sufficient to allow healing, usually within eight to twelve weeks. However, instances of nonunion and delayed union have been described, often among runners who continued the offending activity after development of the stress fracture.
In the case of our patient, the fracture was not initially appreciated on radiographs and the patient continued to run for seven months following the onset of pain (albeit on a sporadic basis) before stopping. The extent to which this continued activity contributed to the nonunion is unclear. Even after four months of complete avoidance of all running activity, however, the patient continued to have symptoms and radiographic findings consistent with a nonunion. In contrast to previous reports, in which patients reported pain primarily with running, our patient also experienced pain when sitting, which made continued conservative management challenging.
While previous case reports in the orthopaedic trauma literature have described unstable pelvic ring injuries that went on to nonunion and required stabilization, we are not aware of any previous case of a pubic ramus stress fracture nonunion that was treated with surgical fixation. Our patient continued to experience substantial pain with activities of daily living and sitting despite ten months of conservative treatment, the last four months of which featured optimal treatment with the complete avoidance of all running activities. Whereas an open approach to the inferior pubic ramus (for plate fixation and bone-grafting) likely would have required a lengthy recovery period, percutaneous screw fixation was performed with minimal morbidity, allowing an early return to activities. We considered this particular nonunion amenable to percutaneous screw fixation because of its location, which permitted adequate fixation via a percutaneously placed screw, as well as its hypertrophic nature. While radiographs, bone scans, and MRI scans are the imaging modalities that are typically used to evaluate pubic ramus stress fractures, computed tomography (CT) scanning may be added to confirm the hypertrophic nature of the nonunion if percutaneous fixation is being considered.
In summary, inferior pubic ramus stress fracture is a well-described clinical entity, primarily occurring among female runners and military recruits. The diagnosis is often delayed because of nonspecific symptoms but, once diagnosed, the condition is usually successfully treated with conservative measures centering on avoidance of the offending activity. However, instances of nonunion and delayed union have been described. In the present report, we presented a case of an inferior pubic ramus stress fracture nonunion in a runner that was successfully treated with minimally invasive screw fixation.
Reference: Okike K, Moritz BE. Minimally invasive screw fixation of inferior pubic ramus stress fracture nonunion in a runner: A case report. JBJS Case Connect. 2016 Apr 13;6(2):e26.
What is the diagnosis?
Osteoid osteoma
Metastatic carcinoma
Stress fracture
Pelvic floor avulsion
Osteoporosis

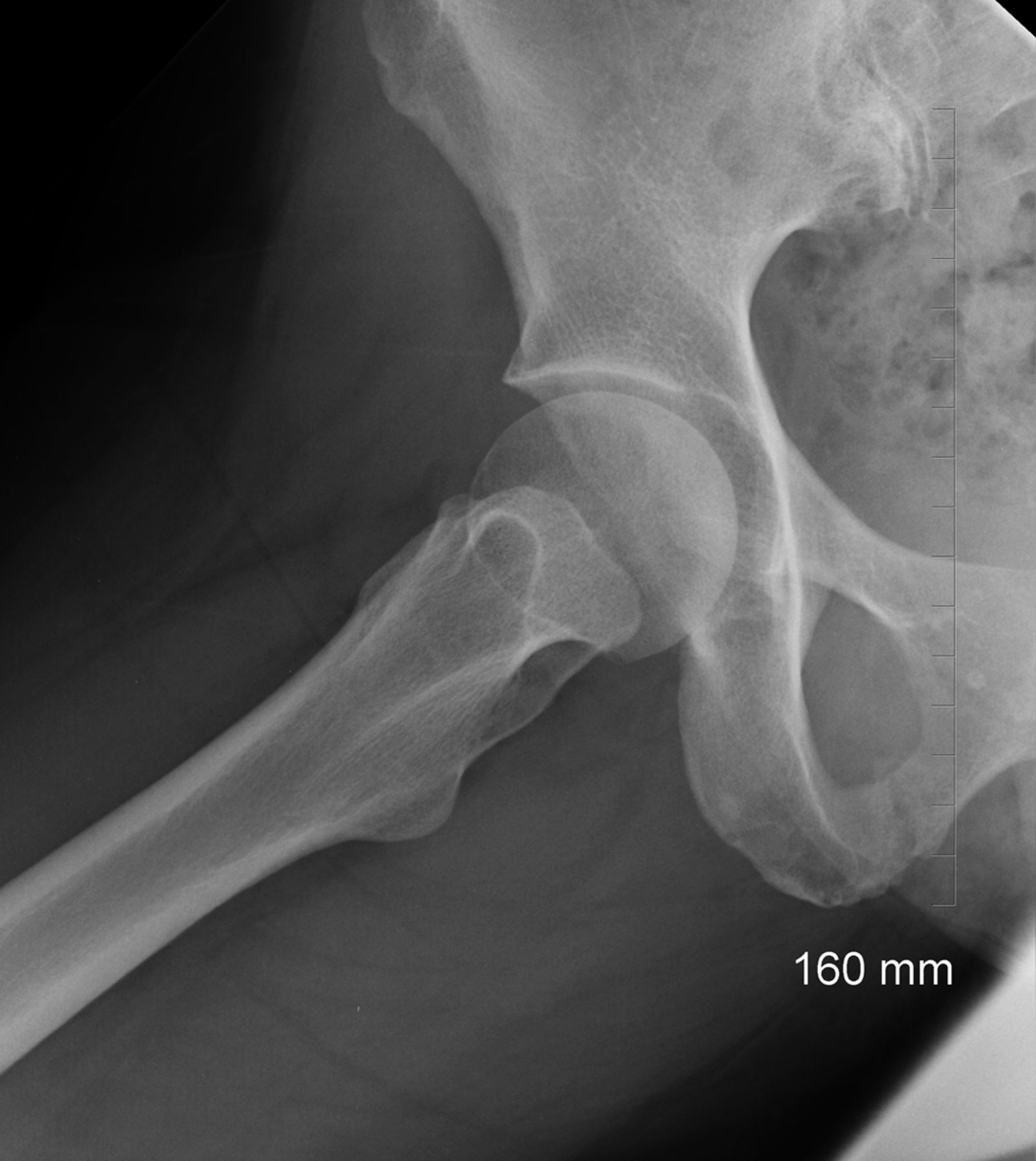
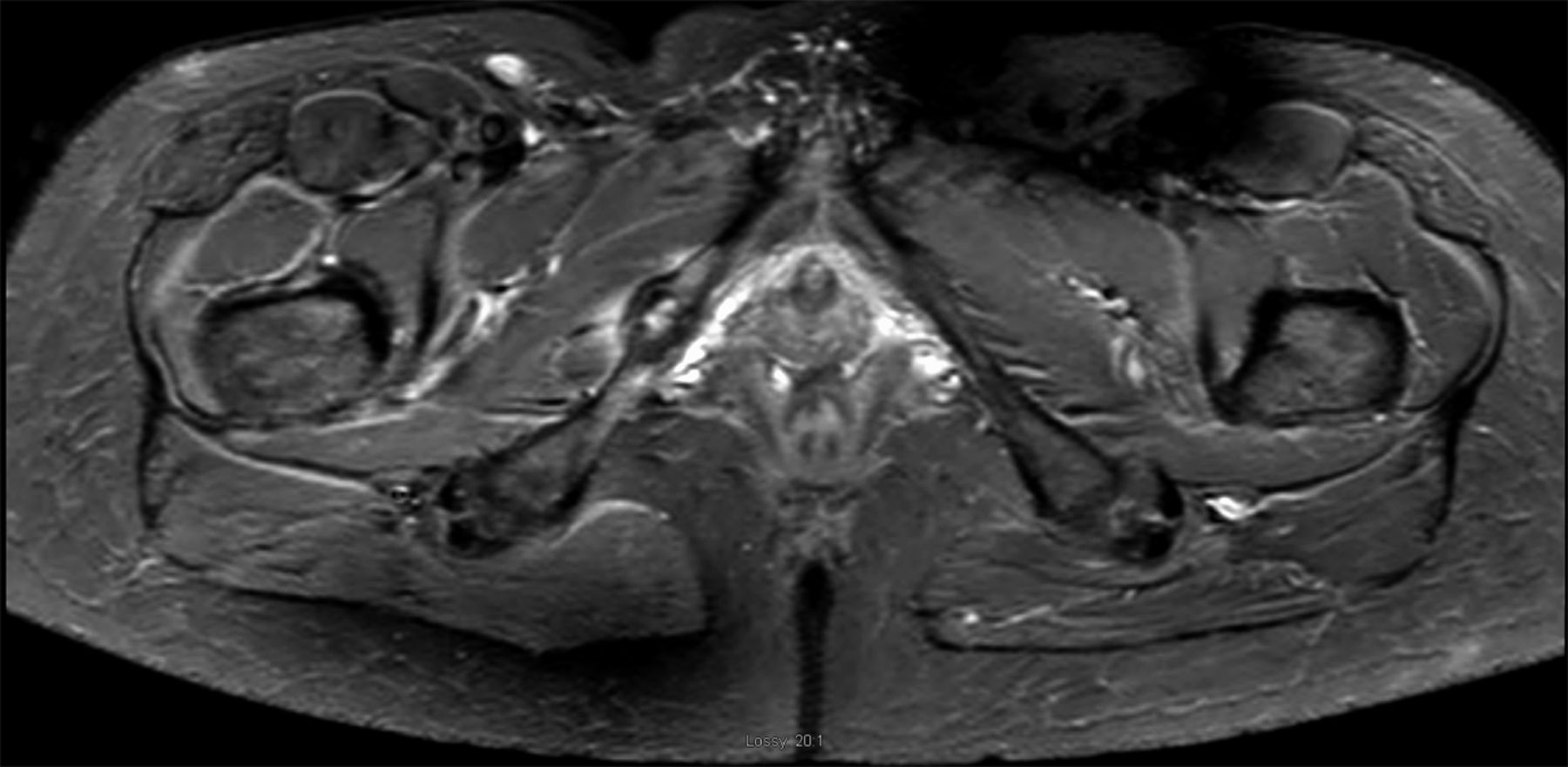
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5-A
Fig. 5-A Fig. 5-B
Fig. 5-B Fig. 6
Fig. 6 Fig. 7
Fig. 7