A 74-Year-Old Woman with Worsening Limp in the Right Lower Limb
April 19, 2017
A 74-year-old, 150-cm-tall woman weighing 45 kg presented with gradually increasing right thigh pain and limping gait for the past month without a history of trauma. She had sustained an osteoporotic intertrochanteric fracture (AO 31 A1-2) in the same hip 3.5 years prior to the visit. This fracture had been treated with internal fixation using an intramedullary nail (INTERTAN; Smith & Nephew). Complete union had been noted at the 1-year follow-up, and the patient had recovered the prefracture gait function (Fig. 1). The bone mineral density T score was −4.1, indicating osteoporosis. Thus, alendronic acid therapy (70 mg once weekly) was started after surgery to prevent a secondary osteoporotic fracture.
The patient was followed until 12 months after surgery. After 1 year, she was lost to follow-up, but she had been taking the alendronic acid regularly. An anteroposterior radiograph 3.5 years later showed focal eccentric sclerosis and thinning of the lateral cortex around the distal portion of the nail with peri-nail lucency (Fig. 1). To evaluate the origin of pain, bone scintigraphy was performed, which revealed hot uptake at the level of the distal interlocking screw (Fig. 2). The patient underwent revision surgery with a long nail (A2FN; DePuy Synthes) to treat the pain. Ambulation with a walker was started 6 weeks after surgery. Complete union was observed, and she remained pain-free at 12 months postoperatively (Fig. 3). However, at the 1-year follow-up, the gait function had not returned to the prefracture status.
Reference: Yoon BH, Park SB. Insufficiency fracture occurring 3 years after union of an intertrochanteric hip fracture: a case report. JBJS Case Connect. 2017 Jan 11;7(1):e1.
Intramedullary nails are now the implant of choice for orthopaedic surgeons when treating intertrochanteric fractures. However, the use of intramedullary nails has been historically related to complications such as secondary femoral shaft fractures that eventually require revision surgery. Most of these are long oblique fractures or spiral-shaped fractures that usually occur as a result of a fall within 3 months of the index surgery. One study suggested a possible explanation as to why secondary fractures often occur before the expected time of fracture union. Before union is complete, some micromotion can cause stress to be transferred from the fracture site to the tip of the implant; those authors suggested that once the fracture has healed, this stress is no longer present. However, the secondary fracture in our patient had a transverse shape and occurred after union was complete. Even after a fracture has achieved complete union, stress concentration at the distal area of the nail can lead to an insufficiency fracture.
Our case has the features of an insufficiency fracture as defined by an American Society for Bone and Mineral Research task force: (1) The fracture was not associated with trauma. (2) It was a complete transverse fracture that extended through both cortices, which was evident on the bone scan. (3) There was apparent localized periosteal thickening of the lateral cortex at the fracture site. (4) The fracture was noncomminuted. Insufficiency fracture occurred through the distal locking screw, and the resulting instability could have led to endosteal thinning.
Although the fracture was not complete in our patient, insufficiency fractures with intractable thigh pain and hot uptake, as noted on bone scintigraphy, seldom heal spontaneously; therefore, revision surgery was scheduled. During this procedure, we performed reaming to obtain a better outcome with the autograft and increase the periosteal blood supply. During the process of reaming, the incomplete configuration of the fracture became complete. Additionally, the alignment of the femoral shaft straightened as did the alignment of the long nail after surgery.
In our patient, the varus femur and the use of alendronic acid possibly led to this insufficiency fracture. Patients with an atypical femoral fracture are known to have a more varus proximal femoral geometry than those without fracture. In our patient, the neck-shaft angle was measured as 117° at the fracture site and 125° on the contralateral side at the final follow-up after the index surgery. The reduced bone turnover by bisphosphonate treatment in our patient also increased the accumulation of microdamage; microdamage can subsequently reduce bone toughness and increase susceptibility to new cracks.
Bisphosphonate treatment was essential to our patient to prevent a secondary osteoporotic fracture. In an aged Chinese population, relatively shorter femora and excessive anterior bowing have been observed. The use of a long nail can prevent abutting of the nail tip with the femoral cortex by passing through the most varus area of the femur, giving more stability to these patients who need long-term bisphosphonate therapy. Although 5° of varus is an acceptable range of reduction for an intertrochanteric fracture, varus should never be allowed in elderly patients who have an especially short curved femur.
Several case reports have described atypical insufficiency fracture after total hip arthroplasty. All of the patients had used bisphosphonate therapy for more than 3 years. These fractures also occurred below or around the stem tip and showed localized periosteal thickening of the lateral cortex. In our patient, worsening of thigh pain without trauma suggested an insufficiency fracture. To our knowledge, atypical bisphosphonate-related fractures at the level of the distal interlocking screw after repair with a short intramedullary nail have not been reported previously.
In our patient, an insufficiency fracture at the level of the distal interlocking screw occurred even though complete union had been obtained. Physicians should be aware of the possibility of a stress fracture when a patient has thigh pain after an intertrochanteric fracture has healed following repair with a short intramedullary nail.
Reference: Yoon BH, Park SB. Insufficiency fracture occurring 3 years after union of an intertrochanteric hip fracture: a case report. JBJS Case Connect. 2017 Jan 11;7(1):e1.
What is the diagnosis?
Osteoporotic femoral fracture
Osteolysis related to fretting corrosion of an interlocking screw
Atypical insufficiency fracture related to an interlocking screw
Posttraumatic femoral shaft fracture
Recurrent intertrochanteric fracture

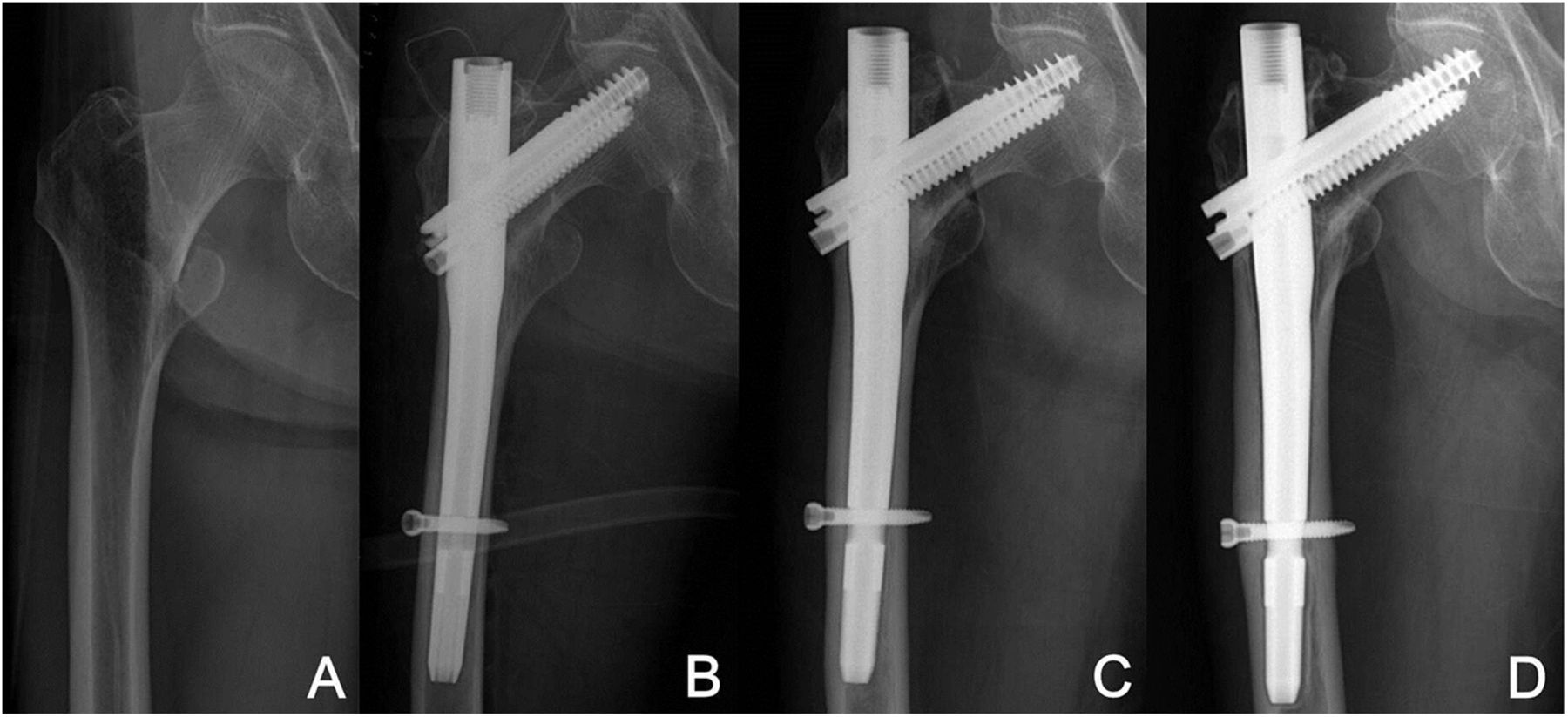
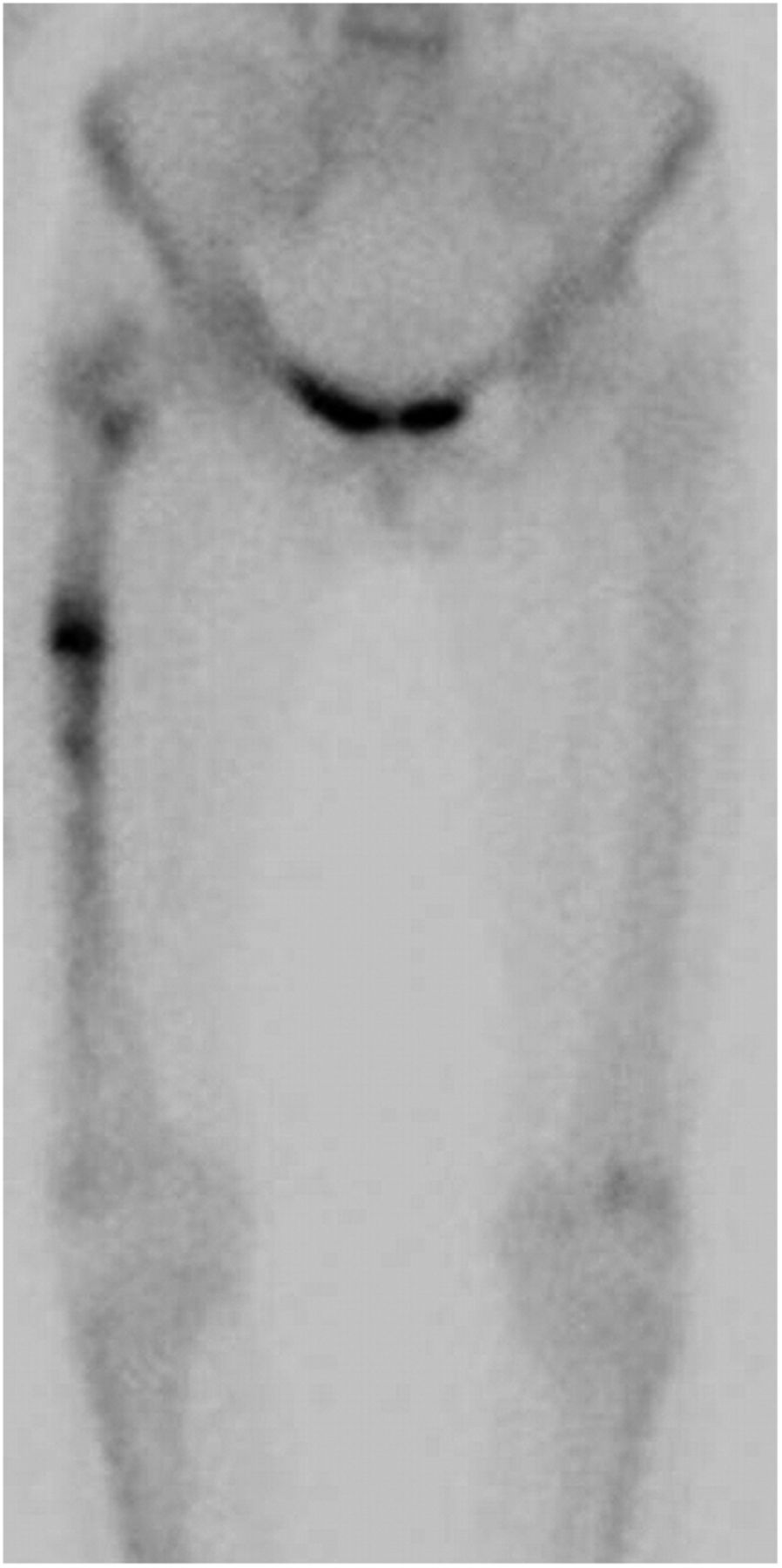

 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3