A 37-Year-Old Man with Persistent Pain and Back Deformity
July 5, 2017
A 37-year-old man, who had undergone an open operation on the right side of the neck for treatment of internal carotid artery stenosis at the age of 6 years, worked as a truck driver without any symptoms related to the shoulders. His occupation included overhead lifting of loads, and he felt sudden pain in the posterior aspect of the right shoulder during heavy load-bearing. Although the severe pain was relieved in 1 month, he developed loss of shoulder elevation, rapid fatigability with pain, and deformity of the back during shoulder motion. The symptoms had persisted for 3 months by the time that he visited our department.
Physical examination showed atrophy of the right trapezius muscle. With the arms at his side, the position and rotation of the scapulae were asymmetric. The right scapula was located laterally, it inclined inferiorly, and its medial border protruded when compared with the left side (Fig. 1-A). During shoulder elevation, inferior rotation and prominence of the medial border of the scapula with lateral displacement became apparent (Fig. 1-B). Active mobility of the right shoulder was severely restricted to 90° in anterior elevation and 70° in abduction. Passive range of shoulder motion was not restricted, and there was no difference in the range of active internal and external rotation on the right and left sides. Trapezius muscle function, which was assessed with a resisted shoulder shrug, was obviously weak on the right side. While performing a wall push-up test, medial winging of the scapula was noted, which indicated weakness in the serratus anterior muscle.
Radiographs of the right shoulder showed no abnormalities. Magnetic resonance images (MRIs) were acquired (Figs. 2-A and 2-B).
The patient was followed conservatively for 2.5 years from the onset of symptoms. The symptoms persisted, and 2 additional electromyography (EMG) examinations, performed at 1 and 2 years after onset, showed no recovery of neurogenic changes in the serratus anterior and trapezius muscles; the patient was diagnosed with combined palsy of the spinal accessory nerve and the long thoracic nerve on the right side. Therefore, surgical intervention was selected.
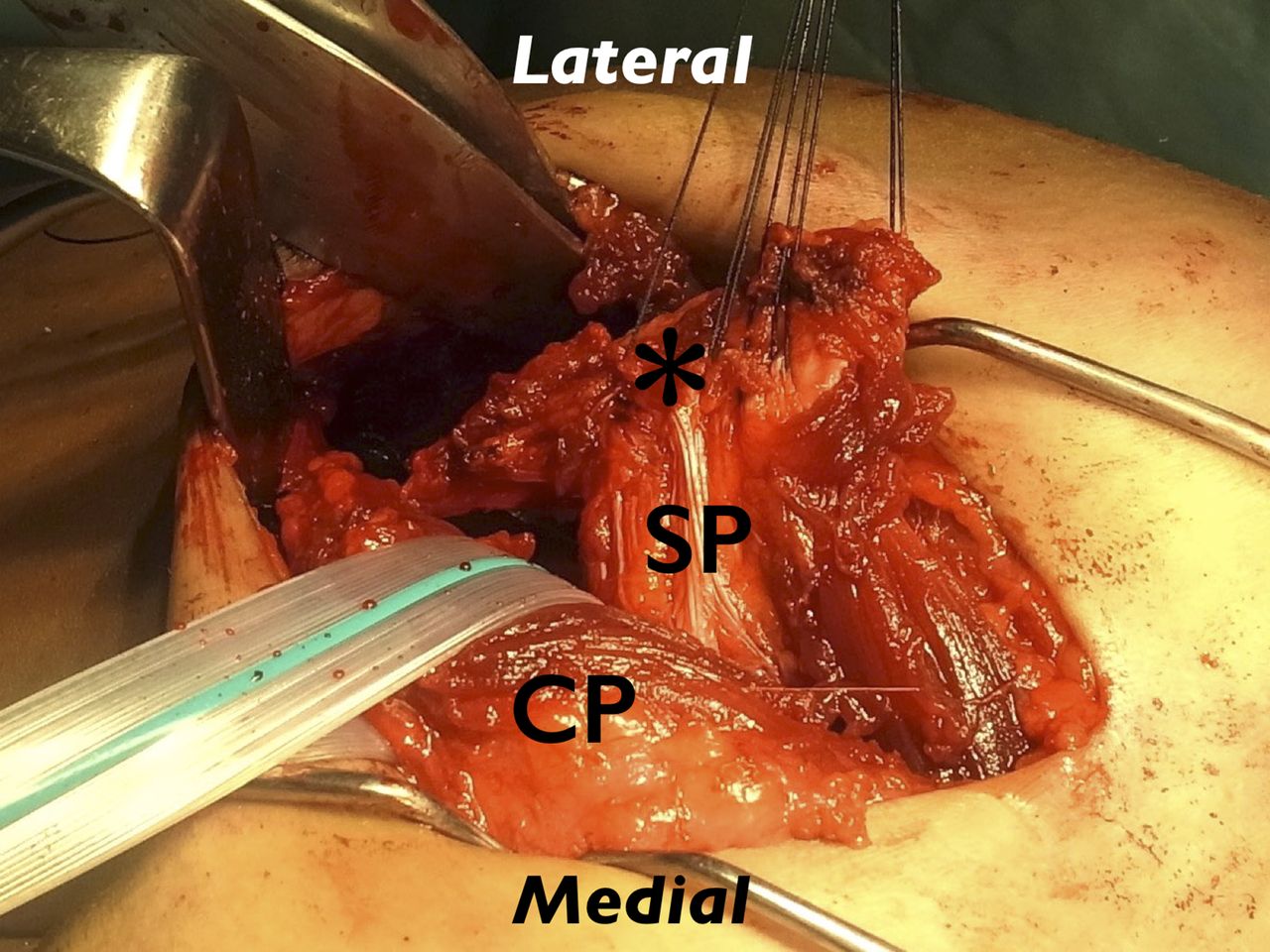
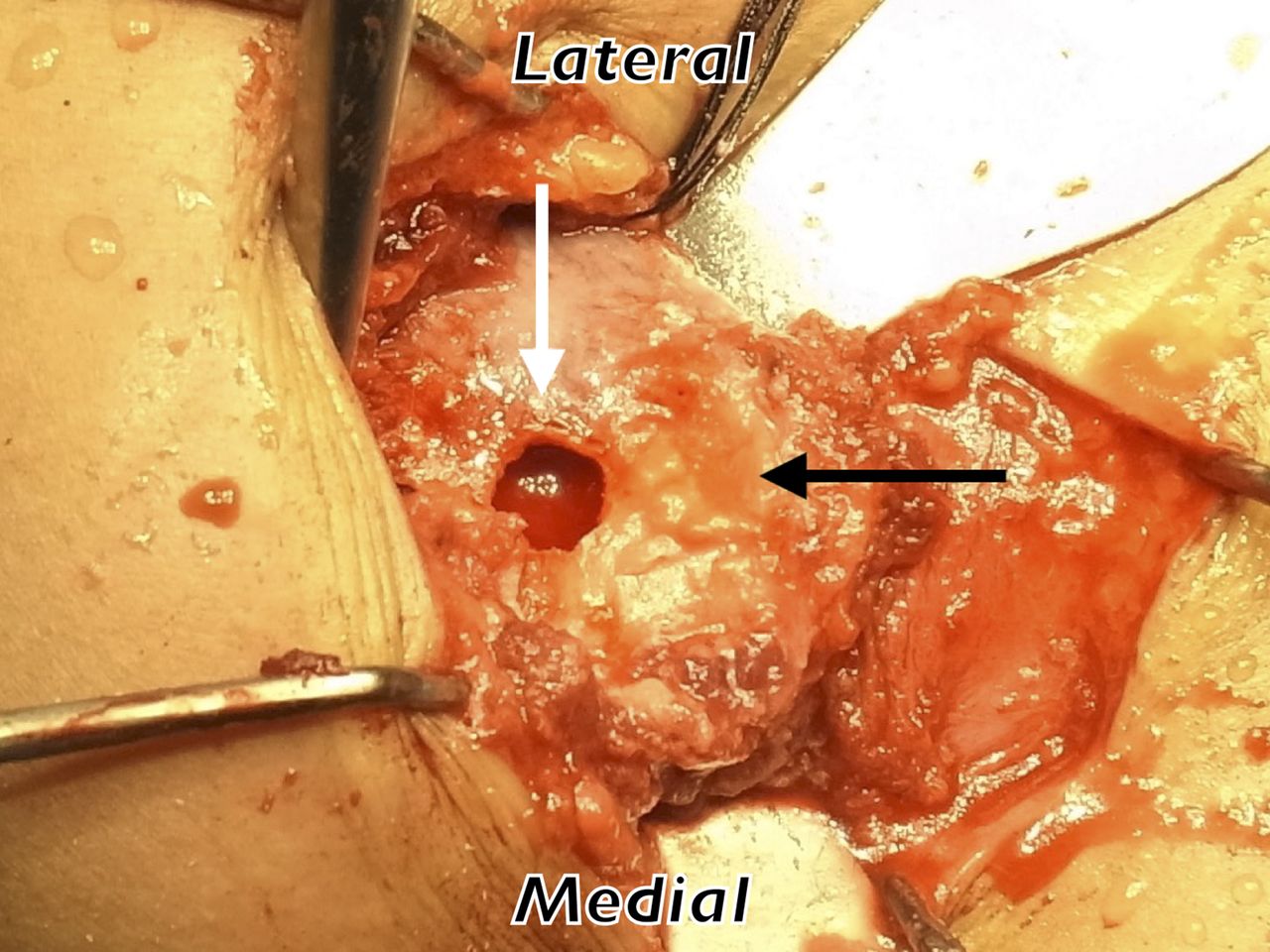
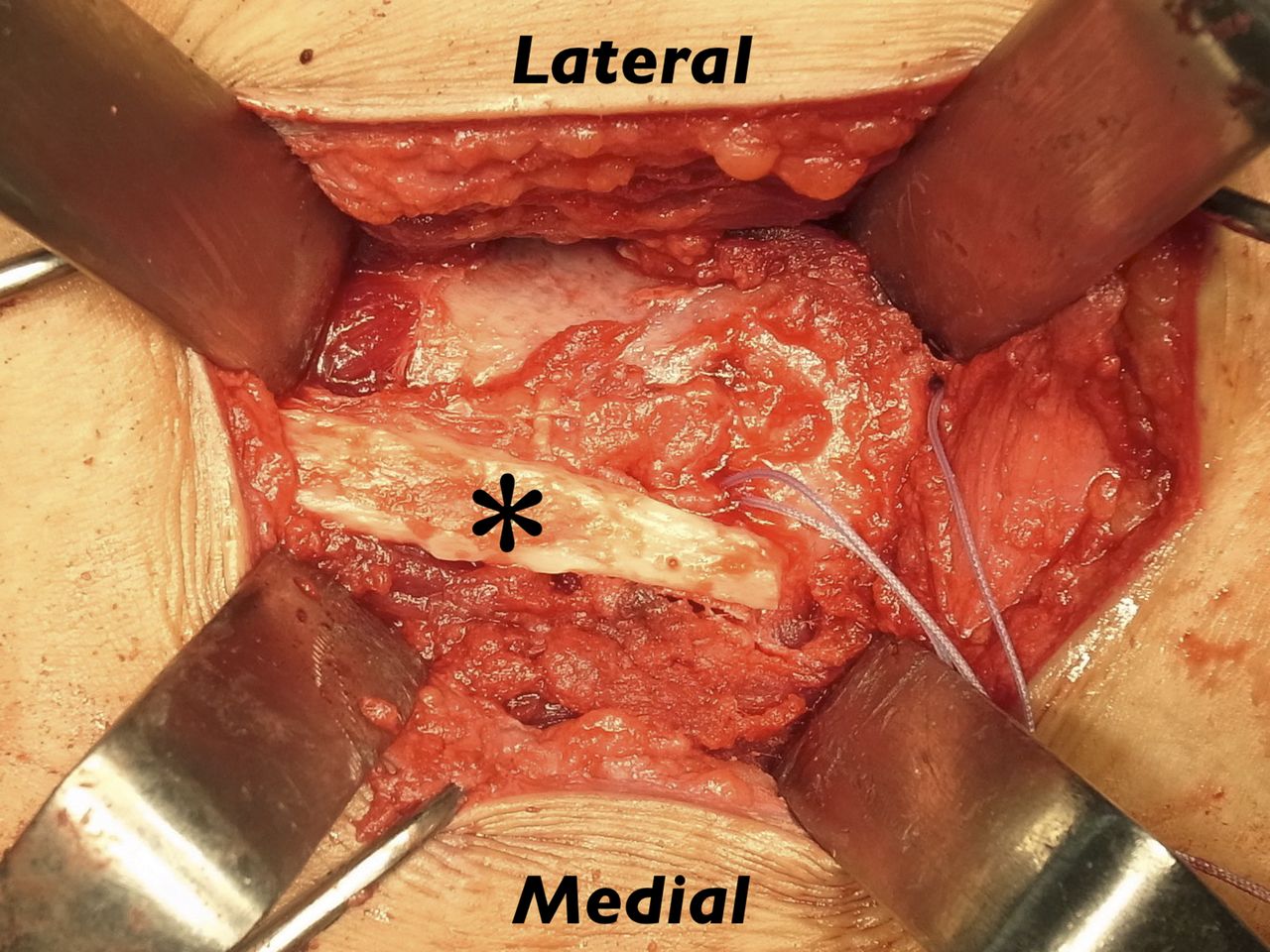
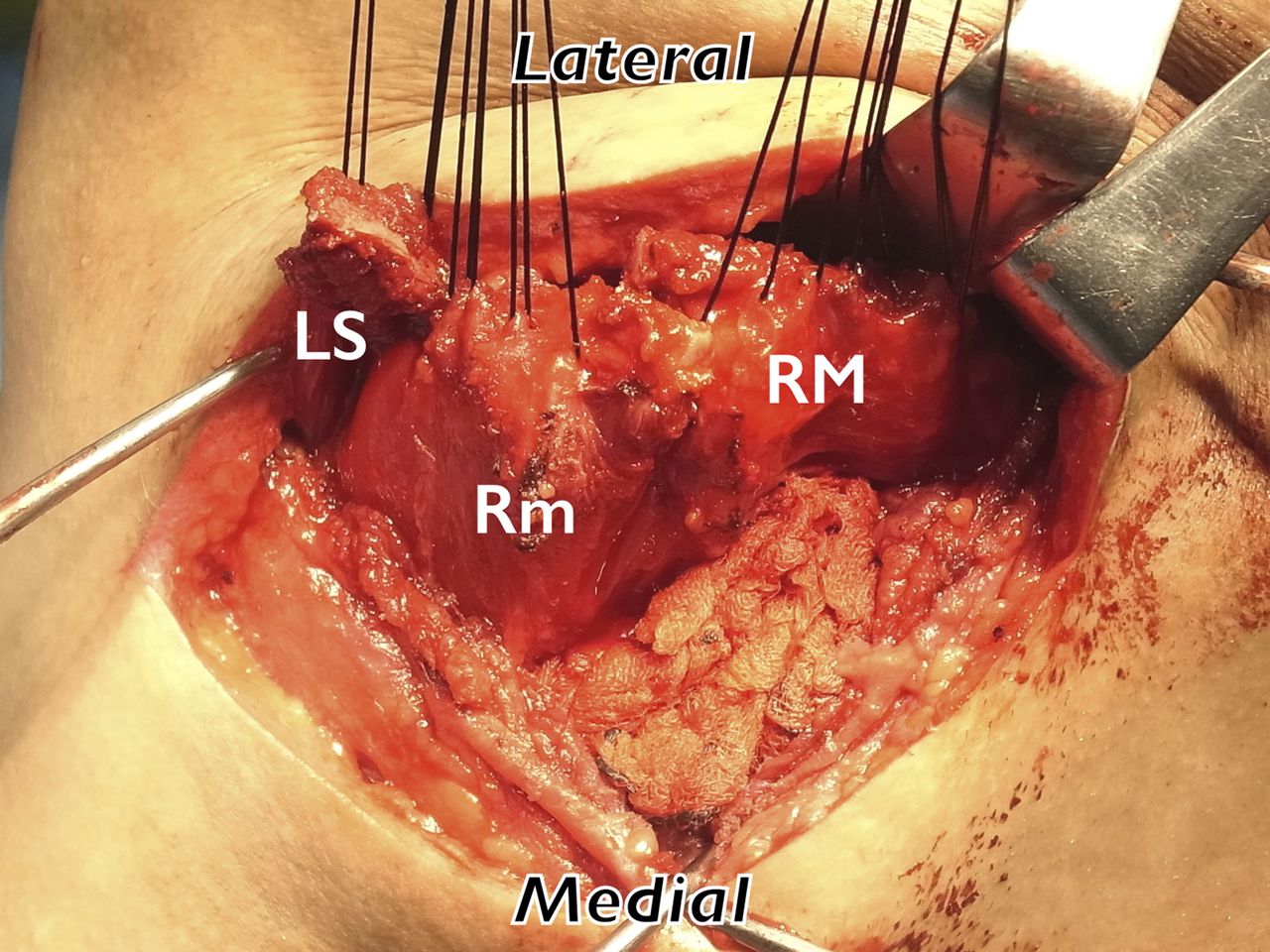
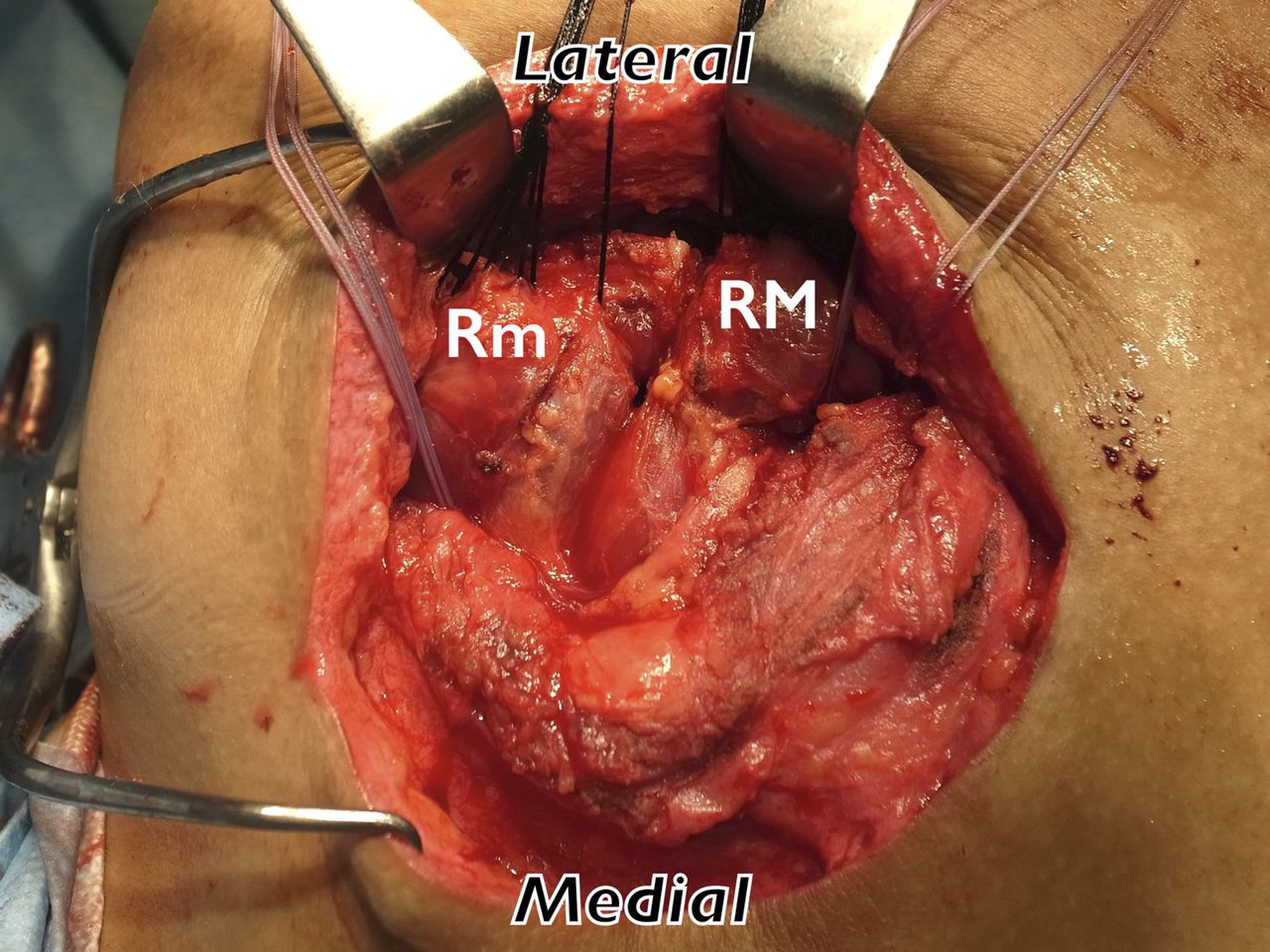
Surgery included a pectoralis major transfer, which substituted for the serratus anterior muscle, combined with levator scapulae and rhomboid muscle transfers, which substituted for the trapezius muscle. The patient was placed in the left lateral decubitus position. Through a 6-cm anterior skin incision, the sternal portion of the pectoralis major muscle was harvested from its insertion with a 4-cm-long piece of the humeral shaft with use of a cutting burr (Fig. 3-A). The pectoralis graft was mobilized medially to gain length for transposition. Then the inferior angle of the scapula was exposed through a 5-cm-long posterior incision along the posterolateral edge, and a bone tunnel with a diameter of 2 cm was created on the inferior angle (Fig. 3-B). A bluntly dissected tunnel from anterior to posterior between the chest wall and the latissimus dorsi muscle was created, and the pectoralis tendon was passed through the tunnel posteriorly. After decortication of the inferior angle, the bone piece that was attached to the tendon was passed into the hole, and the pectoralis major muscle was transferred directly over the lateral aspect of the chest wall (Fig. 3-C). Next, an 8-cm-long incision was made on the medial border of the scapula, and the levator scapulae and rhomboid muscles were detached from the medial edge with small pieces of their respective osseous insertions (Fig. 3-D). With multiple transosseous #2 FiberWire sutures (Arthrex), the levator scapulae muscle was transferred to the scapular spine just posterior to the posterior aspect of the acromion through another 3-cm skin incision, and the rhomboid minor and major muscles were transferred to the upper and lower aspects of the medial two-thirds of the spine of the scapula after the surface of the spine was decorticated (Fig. 3-E). The right arm was immobilized in a sling after surgery. Passive shoulder elevation exercise was started 4 weeks later.
At 2 months after surgery, the patient was allowed to actively elevate the arm, and he was able to start heavy labor and sports activities at 6 months postoperatively. At the final follow-up 4 years after surgery, he did not feel shoulder pain with daily activities. He had returned to work and could lift light objects overhead. Although asymmetric scapular kinematics remained during shoulder elevation, the winging of the scapula disappeared, and the range of shoulder anterior elevation and abduction improved from a preoperative 90° and 80°, respectively, to a postoperative 145° and 150°, respectively, at the final follow-up (Fig. 4). Abduction strength, which was measured with a dynamometer, had improved from 0 to 4 kg, and the Constant-Murley score, which is a 100-point scale, had improved from 37 to 71 points at the final follow-up.
Proceed to Discussion >>Reference: Ago K, Matsumura N, Iwamoto T, Sato K, Nakamura N, Matsumoto M. Scapular winging caused by combined palsy of the spinal accessory nerve and the long thoracic nerve: a case report. JBJS Case Connect. 2017 Apr 12;7(2):e23.
Scapular winging is a rare disorder, often caused by neuromuscular imbalance in the scapulothoracic stabilizer muscles. Long thoracic nerve palsy leads to serratus anterior muscle paralysis. In most cases, injury to this nerve is thought to be caused by mechanical stress, including compression and traction. Serratus anterior paralysis results in medial winging, which includes superior translation of the scapula with inferior rotation of the inferior angle. Spinal accessory nerve palsy leads to trapezius muscle paralysis; the most common cause is iatrogenic injury during neck surgery. Trapezius paralysis results in lateral winging, which is associated with inferior translation of the scapula, with the inferior angle rotated laterally. The findings of the present case were consistent with the diagnosis of combined palsy of both nerves.
Although long thoracic nerve palsy and accessory nerve palsy are common causes for scapular winging, to our knowledge, only 5 cases of combined palsy have been reported. Omar et al. reported a case with a long thoracic palsy and a spinal accessory nerve palsy following a whiplash injury. Sahin et al. reported a case with compressive neuropathy of both nerves secondary to heavy load-bearing. Both of these cases were diagnosed by EMG examination and were treated conservatively. Bigliani et al. reported surgical results in 22 cases of trapezius paralysis, and they stated that 3 of the patients had an additional long thoracic nerve palsy, which was not fully appreciated at the time of initial treatment. The paralysis of the trapezius was iatrogenic in all 3 of the cases, and they assumed that the etiology of the long thoracic nerve palsy was secondary to traction on the nerve by the unsupported shoulder girdle. In the present case, the patient had a history of neck surgery. The spinal accessory nerve likely had been damaged during the childhood surgery, but it remained asymptomatic. Paralysis of the serratus anterior muscle might have been caused by increased mechanical stress on the long thoracic nerve following long-term scapular dyskinesis. The combined palsy of both nerves appeared to result in substantial loss of shoulder function.
First described by Tubby in 1904, the treatment of paralysis of the serratus anterior muscle with a pectoralis major transfer is known to be effective. Besides direct transfer, extension of the tendon by autografts, such as fascia lata or the semitendinosus tendon, has also been described. Excellent results can be expected with both direct and indirect pectoralis major transfers, but they are not applicable to trapezius paralysis. For the treatment of trapezius paralysis, lateralizing transfers of the levator scapulae and rhomboid muscles provide substitutes for all 3 components of the trapezius. Eden first described this transfer, and Lange reported successful results with this technique; this transfer technique is now called the Eden-Lange procedure. The Eden-Lange procedure is a valuable reconstructive procedure for the treatment of trapezius paralysis. However, this procedure is not applicable to serratus anterior paralysis.
In the present case, both serratus anterior and trapezius paralysis were present. Although muscle transfer techniques are reliable procedures for scapular winging, our concern was that the transferred muscles would not fully compensate for the functions of the trapezius or serratus anterior muscles. Thus, we performed both a pectoralis major transfer and the Eden-Lange procedure. The pectoralis major muscle is involved in shoulder flexion, adduction, and internal rotation, and it does not directly affect scapular motion. The rhomboid and levator scapulae muscles normally assist the trapezius to retract and elevate the scapula. These muscles originate from spinous processes and insert at the medial border of the scapula, without a direct effect on glenohumeral motion. We believed that harvest of the pectoralis major, rhomboid, and levator scapulae muscles would not cause a substantial deficit of shoulder girdle function, and that combined transfers would not increase the risk to the brachial plexus. In our patient, surgical intervention successfully relieved the symptoms and improved shoulder function without any complications. This case demonstrates that even with combined paralyses of the serratus anterior and trapezius muscles, combined muscle transfers that substitute for each muscle can improve shoulder function.
Reference: Ago K, Matsumura N, Iwamoto T, Sato K, Nakamura N, Matsumoto M. Scapular winging caused by combined palsy of the spinal accessory nerve and the long thoracic nerve: a case report. JBJS Case Connect. 2017 Apr 12;7(2):e23.
What is the diagnosis?
C3-4 disc protrusion on the right side
Spinal accessory nerve palsy on the right side
Long thoracic nerve palsy on the right side
Facioscapulohumeral muscular dystrophy on the right side
Combined palsy of the spinal accessory nerve and the long thoracic nerve on the right side

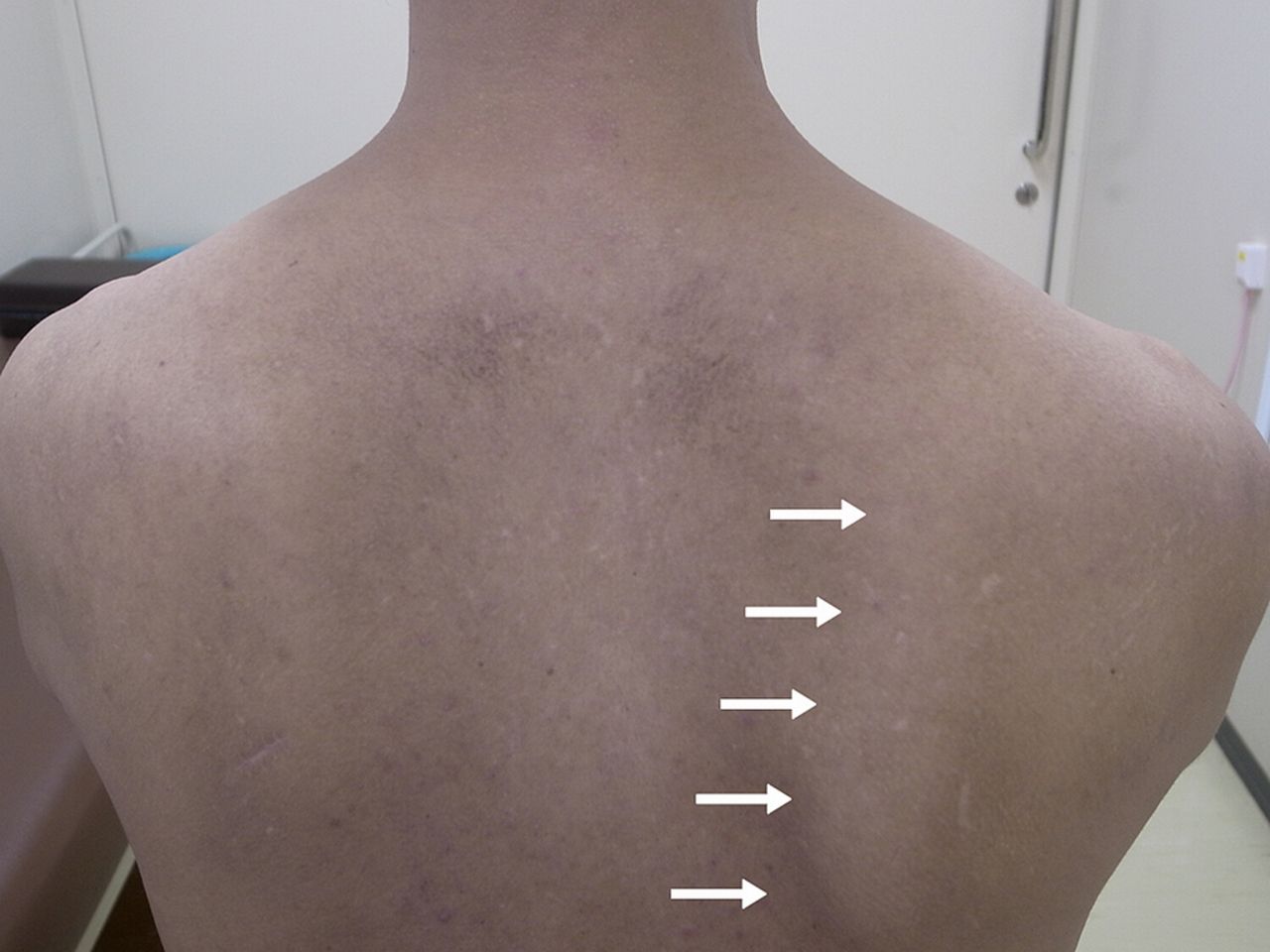

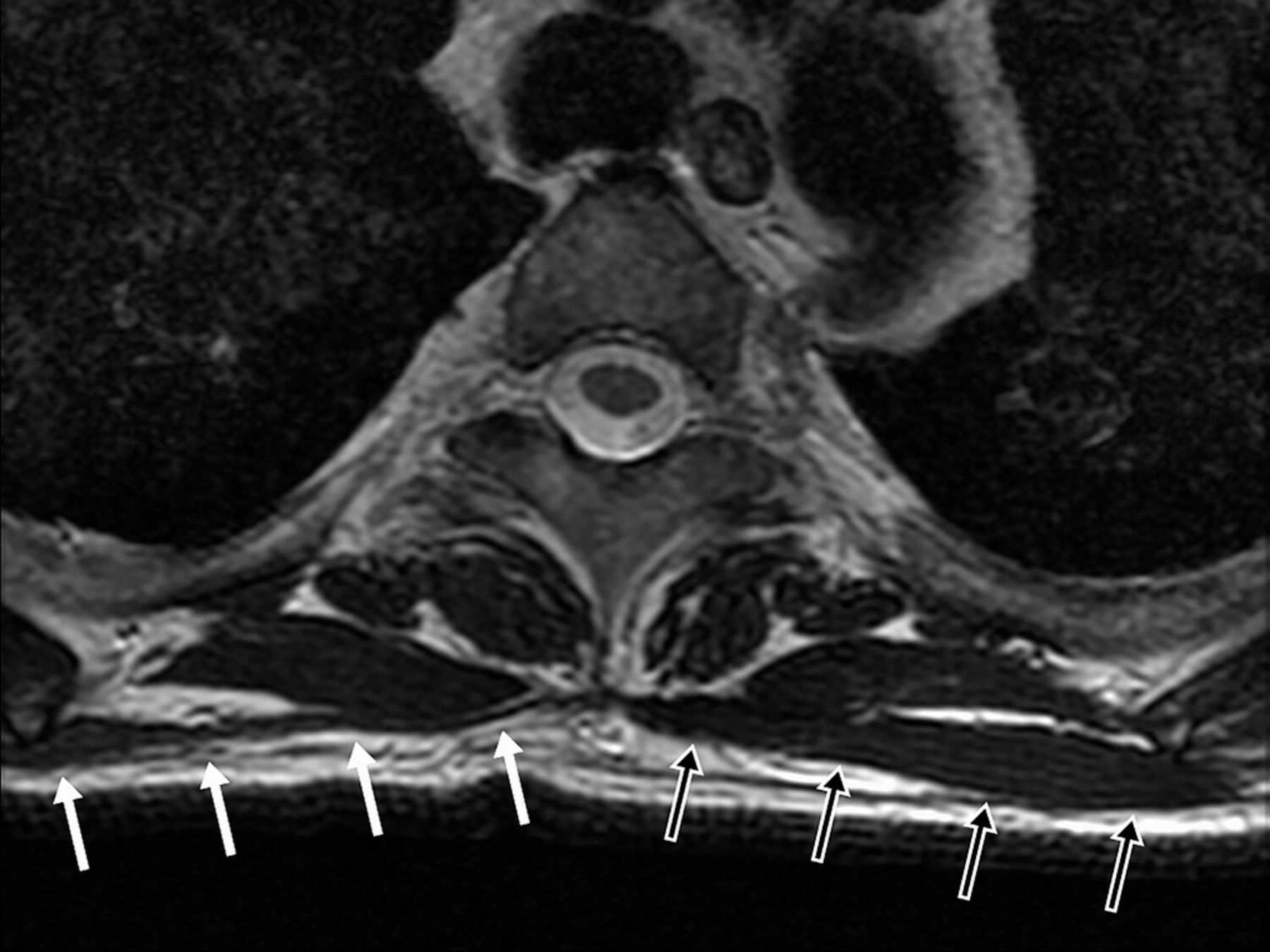

 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B![Fig. 2-A Fig. 2-A Axial T2-weighted MRI (repetition time [TR], 5,200 msec; echo time [TE], 106.4 msec) of the right shoulder (white arrows) compared with the left side (black arrows).](https://quiz.jbjs.org/wp-content/uploads/2017/07/iqjul17-1_fig2a-150x150.jpg) Fig. 2-A
Fig. 2-A Fig.2-B
Fig.2-B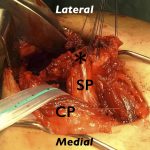 Fig. 3-A
Fig. 3-A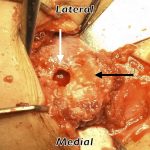 Fig. 3-B
Fig. 3-B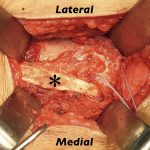 Fig. 3-C
Fig. 3-C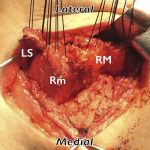 Fig. 3-D
Fig. 3-D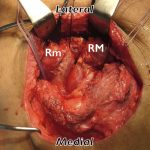 Fig. 3-E
Fig. 3-E Fig. 4
Fig. 4