A 61-Year-Old Woman with Swelling of the Left Elbow
January 17, 2018
A 61-year-old woman with rheumatoid arthritis (RA) was referred to our hospital because of worsening swelling of the left elbow. She had been diagnosed with RA at the age of 55 years at a local hospital, and the left ankle, the left elbow, and the left shoulder joints were severely swollen. After starting methotrexate (MTX) therapy (6 mg/wk), the joint swelling resolved, and the disease activity remained under good control. The patient continued MTX therapy for 82 months. However, 1 week prior to referral to our hospital, her primary care physician, who suspected a flare-up of synovitis due to RA, performed an intra-articular steroid injection of the elbow joint. One week later, the swelling of the elbow became worse, and the patient was referred to our hospital. As shown in Figure 1, the left elbow was severely swollen. Although 7 days had passed since she had received the steroid injection, the injection site had not healed and there was a discharge from the puncture hole. Radiographs of the left elbow were consistent with Larsen grade-3 joint destruction and a large soft-tissue tumor-like shadow (Fig. 2). Magnetic resonance imaging (MRI) showed a mass lesion with low intensity on T1-weighted images and high intensity on T2-weighted images. Following intravenous administration of a gadolinium-containing contrast agent, enhancement was observed mainly at the periphery of the lesion (Fig. 3). These MRI findings suggested aggravation of rheumatoid synovitis, pyogenic abscess, or a soft-tissue tumor with central necrosis.
Chest radiography showed multiple nodular shadows in both lungs, and chest computed tomography (CT) indicated that these nodules were tumor lesions (Fig. 4). Positron emission tomography (PET) with fluorodeoxyglucose integrated with CT (18F-FDG PET/CT) showed uptake in the left elbow, the lung, and the cervical and axillary lymph nodes (Fig. 5). Laboratory data showed an elevation of the erythrocyte sedimentation rate (91 mm/hr), the C-reactive protein (CRP) level (2.16 mg/dL), the lactate dehydrogenase (LDH) level (343 U/L), and the soluble interleukin-2 receptor (sIL-2R) level (2,880 U/mL).
We performed a needle biopsy of the lesion of the left elbow. The specimen showed acute and chronic inflammatory changes with neutrophilic and lymphoplasmacytic infiltration, accompanied by necrotic tissue. Neither atypical lymphocytic cells nor neoplastic cells were observed. No bacteria were detected on culture specimens or with histologic examination. Because we could not reach a definitive diagnosis, an open biopsy of a cervical lymph node was performed. Histologic examination of the lymph node showed a nodular proliferation of large, atypical lymphoid cells with vesicular chromatin around areas of central necrosis (Fig. 6; link to the digital whole slide image: Cervical Lymph Node). Immunohistochemical staining showed that the lymphoid cells around the necrotic area were positive for B-cell markers CD20 and CD79a, but negative for T-cell markers CD4, CD8, CD3, and CD45RO (Fig. 6). They were also positive for leukocyte common antigen (LCA) and negative for CD10, CD56, CD68, and granzyme B. Epstein-Barr virus latent membrane protein 1 (EBV-LMP1) was also positive in the necrotic area (Fig. 7), although EBV-EB nuclear antigen 2 (NA2) tested negative. In situ hybridization for EBV-encoded RNA (EBER) transcript showed scattered positivity for lymphoid cells in marginal areas of the necrotic area (Fig. 7).
The histologic findings of the lymph node in isolation would be consistent with diffuse large B-cell lymphoma (DLBCL). However, since EBV antigens were detected on histology and the patient had been treated with MTX for a long period (82 months), we made the final diagnosis of methotrexate-related lymphoproliferative disorder (MTX-LPD).
MTX therapy was ceased, and a 5-mg daily dose of prednisolone was initiated for the management of the RA. Soon after the MTX therapy was stopped, the swelling around the elbow started to decrease. Laboratory data, such as elevated serum CRP, LDH, and sIL-2R levels, normalized. At 24 months after the cessation of MTX therapy, the swelling of the elbow joint had completely regressed (Fig. 8), and CT of the lung showed that the pulmonary lesions had disappeared.
Proceed to Discussion >>Reference: Hatano T, Ohishi M, Yoshimoto G, Yamauchi M, Maekawa A, Yamamoto H, Oda Y, Endo M, Bekki H, Matsunobu T, Nakashima Y, Okazaki K, Fukushi J, Oyamada A, Iwamoto Y. Methotrexate-related lymphoproliferative disorder presenting with severe swelling of the elbow joint: a case report. JBJS Case Connect. 2017 Jul-Sep;7(3):e65.
MTX-LPD is classified among “other iatrogenic immunodeficiency-associated lymphoproliferative disorders” in the World Health Organization classification of hematologic and lymphatic tumors. These disorders are defined as lymphoid proliferations or lymphomas that arise in patients who are treated with immunosuppressive drugs (e.g., MTX) for autoimmune diseases, such as RA, or conditions other than those in the allograft/autograft transplant setting. MTX-LPD is thought to be related to the reactivation of EBV. EBV has the capacity to induce proliferation and transformation of different cell types, but is characterized by tropism for B cells. It has been shown that patients with RA have a genetic deficiency of cytotoxic T cells, which may result in an elevated EBV level. MTX reportedly suppresses T-cell activation and T-cell adhesion molecule expression. Reportedly, latent antigens encoded by EBV interfere with a number of cellular pathways, leading to oncogenesis. It is also thought that chronic inflammation due to the activity of RA is related to oncogenesis.
Clinical features of MTX-LPD include fever, weight loss, and swelling of the lymph nodes, which are typical features of lymphomas. MTX-LPD reportedly often presents with extranodal lesions in the lung and the subcutaneous tissues. Severe swelling of the elbow was present in our patient. A needle biopsy of the left elbow lesion failed to detect any tumor cells; however, after MTX therapy was discontinued, the swelling of the elbow showed rapid improvement, as did the lymph-node swelling and metastatic lesions in the lungs. Thus, it is likely that the swelling of the elbow was one of the presentations of a systemic LPD. The needle biopsy of the elbow joint showed inflammation without recognizable atypical lymphoid cells, but there was extensive necrosis, so it seems likely that the biopsy specimen was not truly representative of the actual underlying lesion.
Histologic examination of a lymph node is important for the diagnosis of MTX-LPD. The histologic findings in our patient were basically the same as those with diffuse large B-cell lymphoma: large, atypical lymphoid cells with a vesicular chromatin pattern were present, and these were positive for B-cell markers. EBV-related antigens, such as EBV-LMP1 and EBER, are positive in the majority (67% to 80%) of cases of MTX-LPD. We were able to reach a final diagnosis because the histologic examination of the cervical lymph nodes was positive for these antigens.
The prevalence of lymphoma is known to be high among patients with RA, although it is unclear whether MTX therapy increases the risk of lymphoma. The cumulative dosage associated with increased risk of MTX-LPD has been a major issue of discussion. Kameda et al. reported that a higher MTX dose is associated with LPD onset in patients with RA. Yamakawa et al. studied 21 cases of MTX-LPD and reported that the average dosage of MTX was 6.1 mg/wk for 71.1 months. Our patient had taken a dosage of 6 mg/wk for 82 months, which is more than the total dosage reported by Yamakawa et al.
Reportedly, 23% to 60% of MTX-LPD cases improve after stopping MTX therapy; the rate of complete response is higher in EBV-positive than in EBV-negative patients. According to the World Health Organization, 17% of cases of DLBCL, which is the most frequent type of MTX-LPD, and 28% of patients with Hodgkin lymphoma remit after withdrawal of MTX therapy. Among EBV-positive cases, >40% of patients with DLBCL and >30% of patients with Hodgkin lymphoma are reported to achieve remission by withholding MTX therapy. According to Rizzi et al., 83% of patients with RA with MTX-LPD who showed complete remission had done so within 4 weeks. Chemotherapy and radiation are considered when there is no regression within 4 weeks after stopping MTX therapy. Although our patient was successfully treated by stopping MTX therapy, careful observation for recurrence is needed.
In summary, we have described a patient with MTX-LPD who presented with soft-tissue swelling around the elbow joint. When patients who are undergoing treatment with MTX show severe soft-tissue swelling, MTX-LPD should be considered as one of the possible diagnoses.
Reference: Hatano T, Ohishi M, Yoshimoto G, Yamauchi M, Maekawa A, Yamamoto H, Oda Y, Endo M, Bekki H, Matsunobu T, Nakashima Y, Okazaki K, Fukushi J, Oyamada A, Iwamoto Y. Methotrexate-related lymphoproliferative disorder presenting with severe swelling of the elbow joint: a case report. JBJS Case Connect. 2017 Jul-Sep;7(3):e65.
What is the diagnosis?
Granulomatous inflammation suggestive of Mycobacteria infection
Epithelioid sarcoma
Methotrexate-related lymphoproliferative disorder
Synovial sarcoma
Metastatic carcinoma of lung origin


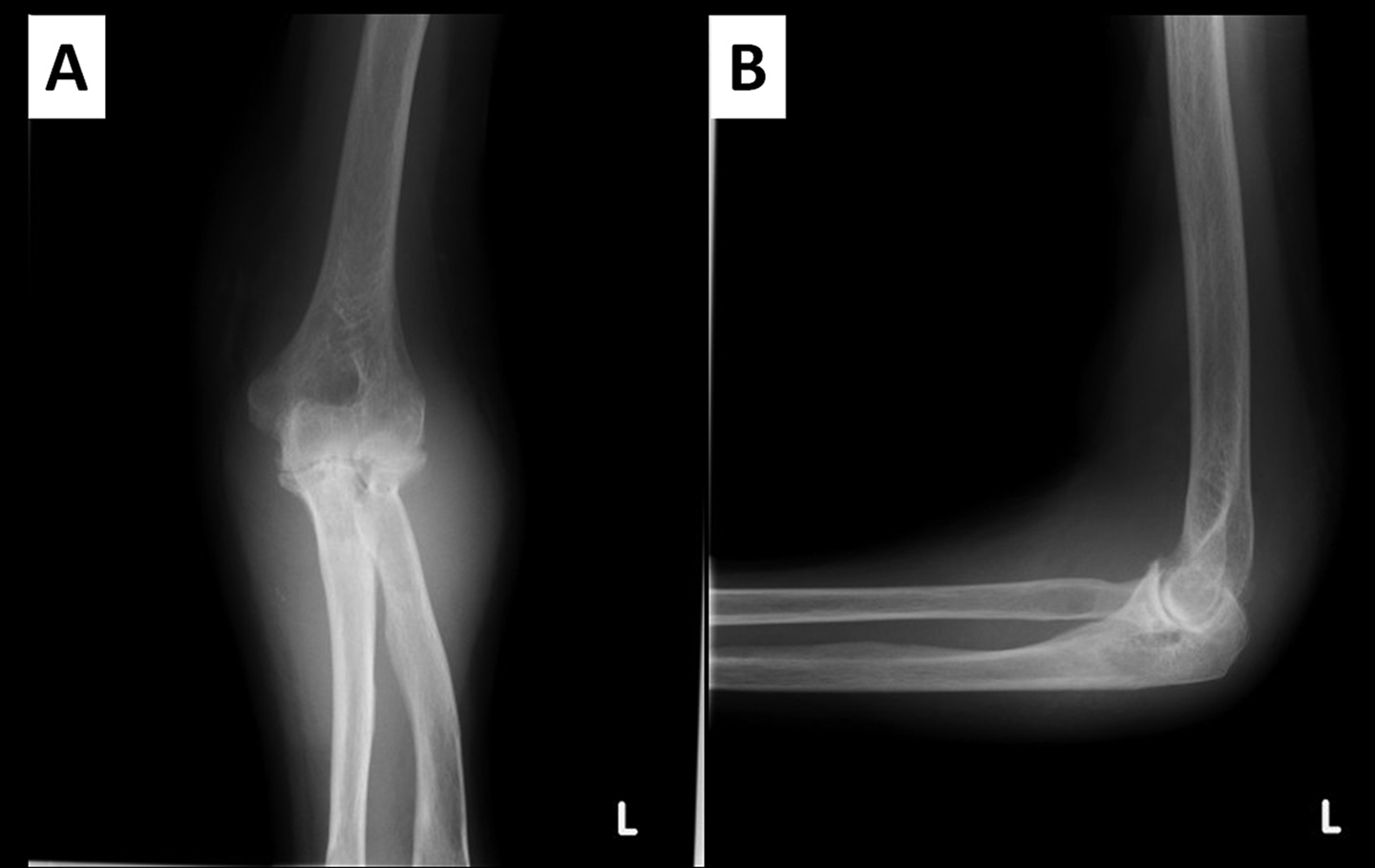
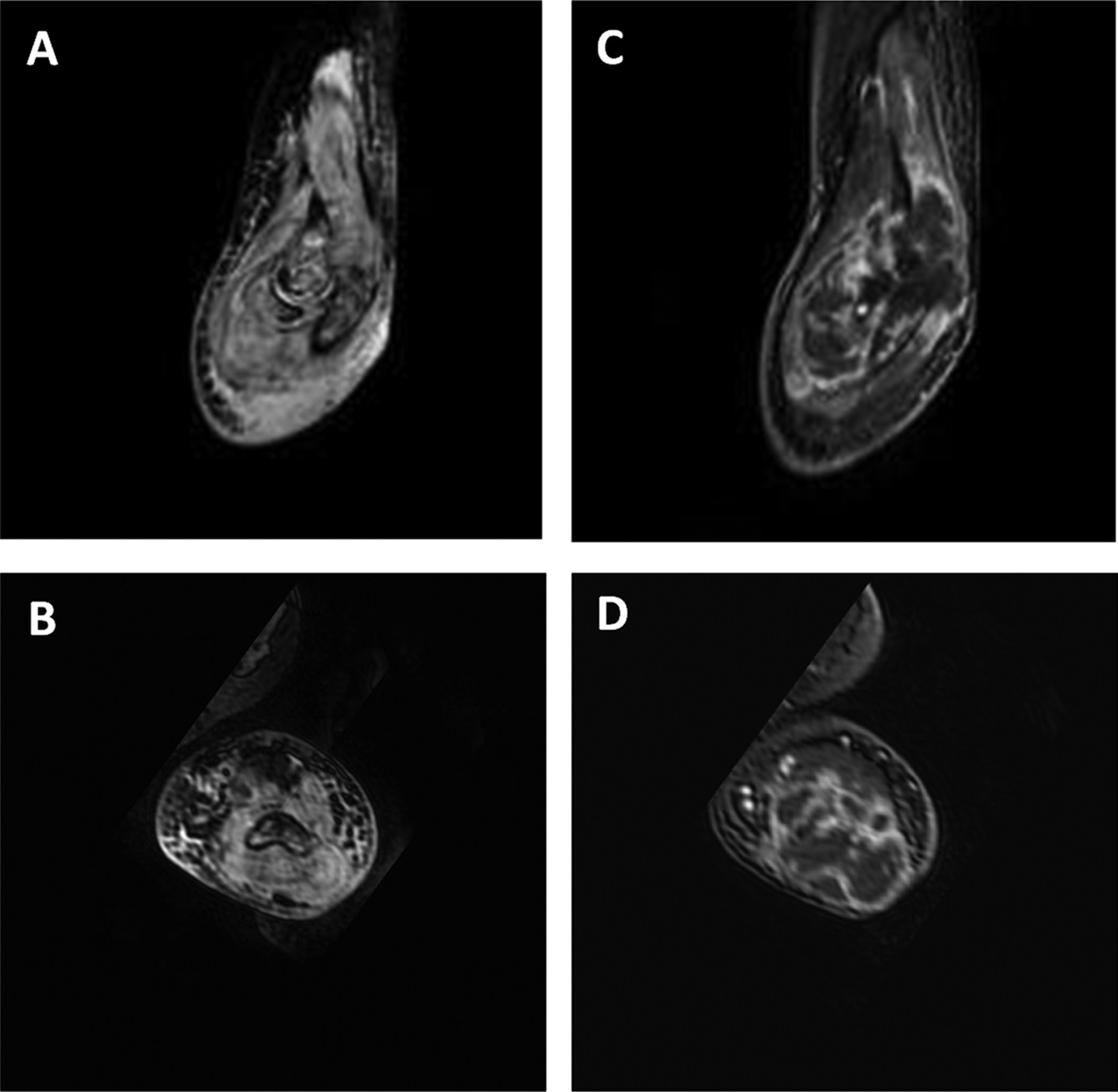
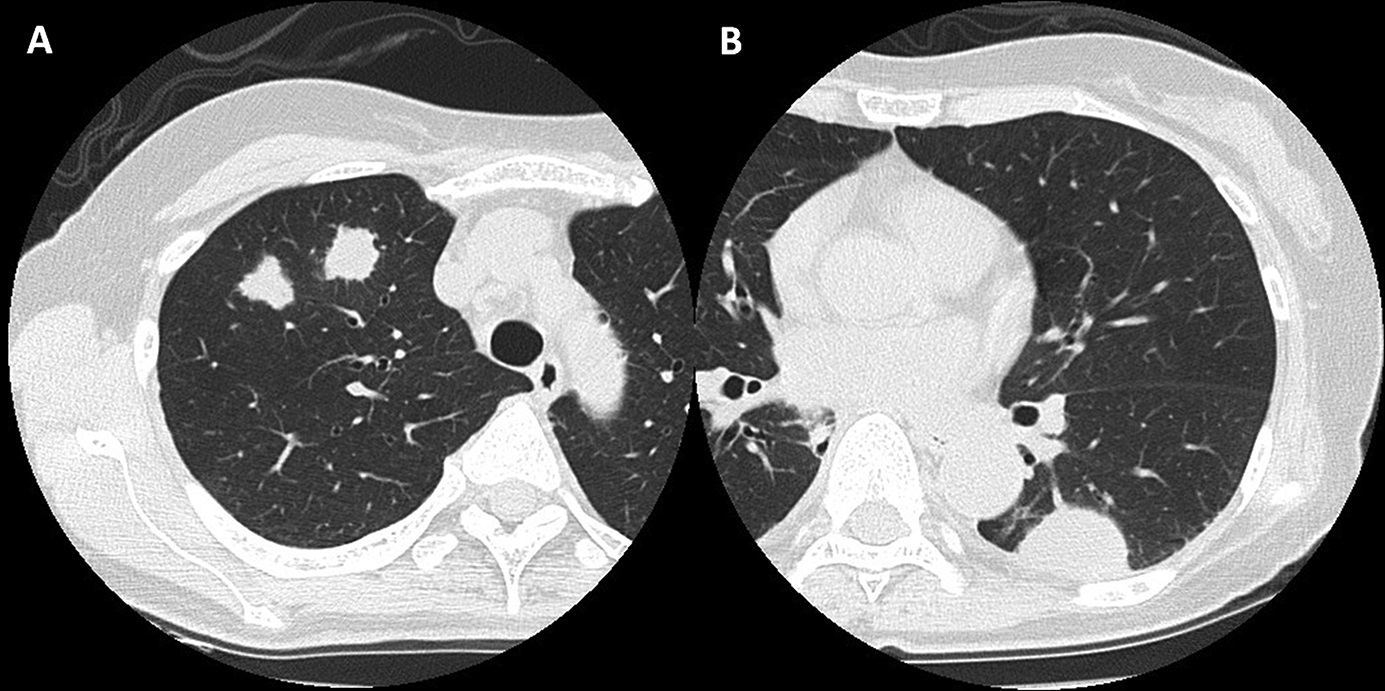

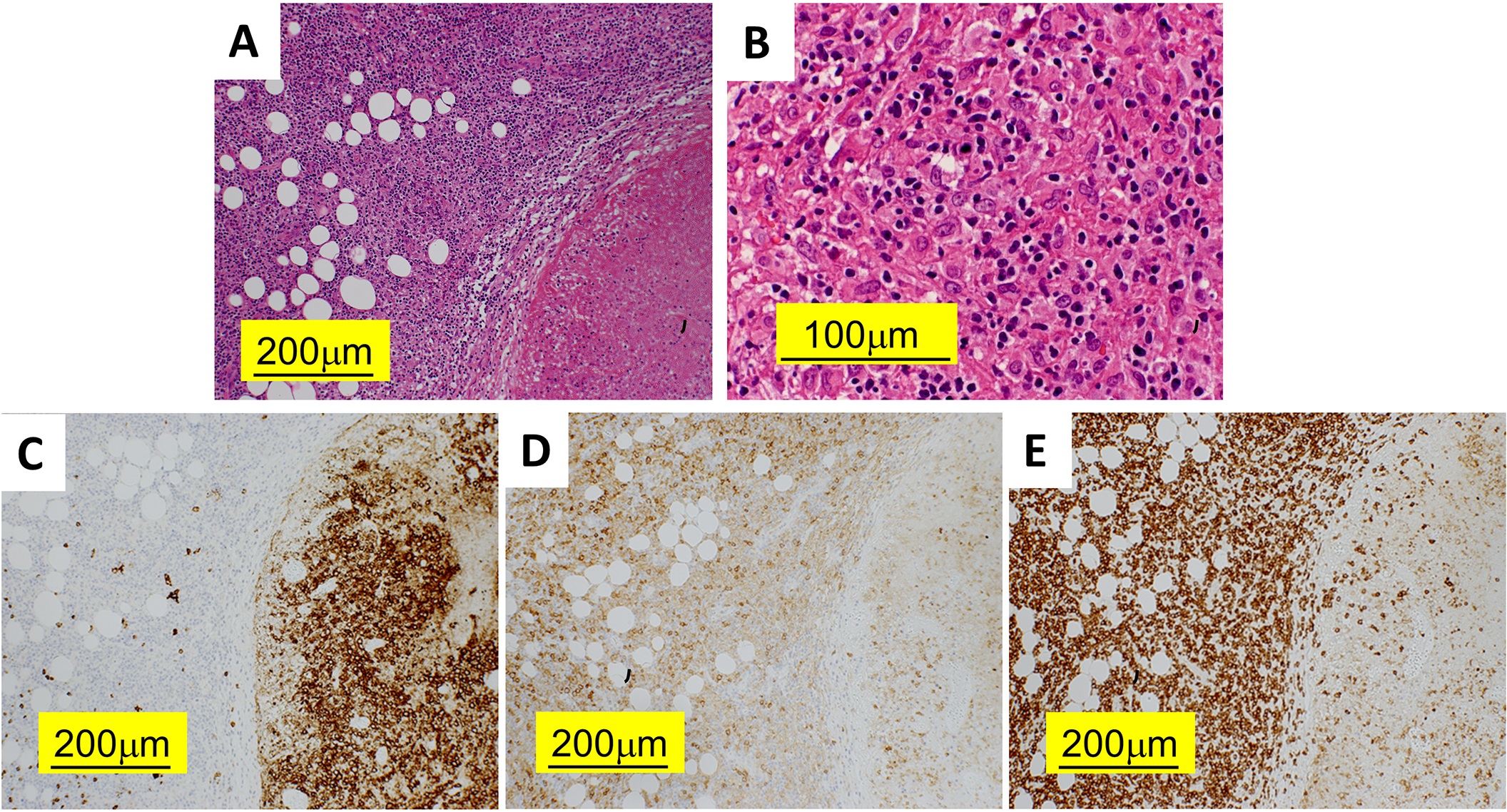
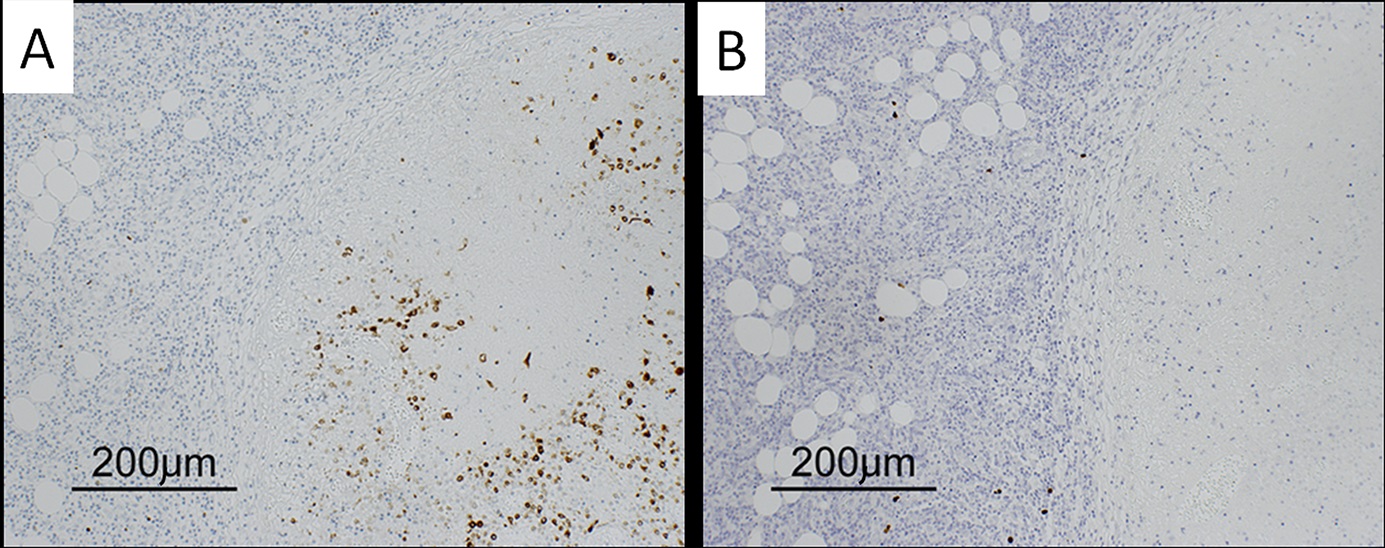
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3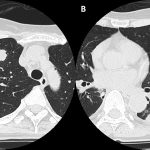 Fig. 4
Fig. 4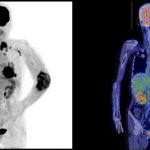 Fig. 5
Fig. 5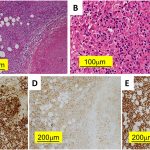 Fig. 6
Fig. 6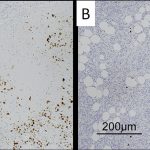 Fig. 7
Fig. 7 Fig. 8
Fig. 8