A 52-Year-Old Man with a History of Stiffness and Pain in the Shoulder
April 18, 2018
A fifty-two-year-old right-hand-dominant man had originally presented ten years previously with a six-month history of atraumatic pain and stiffness in his right shoulder. Rotator cuff strength was equivalent to that in his contralateral (nonsymptomatic) upper extremity, and radiographs demonstrated end-stage glenohumeral arthritis with a well-centered humeral head. After an extensive course of conservative care, he underwent right total shoulder arthroplasty using the Zimmer Anatomical Total Shoulder System with a cemented glenoid component and press-fit humeral stem.
His initial postoperative course was uncomplicated. Nine months after surgery, he had no pain and was able to return to all of his preoperative activities as tolerated. On examination, he had forward flexion to 160°, external rotation to 50°, and internal rotation to the level of T10. Rotator cuff strength was 5/5 in all planes. Imaging demonstrated a well-placed stem and glenoid component with no evidence of loosening (Fig. 1). Three years after surgery, he returned with a six-week history of right shoulder weakness with an insidious onset. Examination demonstrated decreased range of motion (forward flexion to 130°, external rotation to 40°, and internal rotation to L3) as well as decreased abduction and external rotation strength. Radiographs and a computed tomographic (CT) arthrogram demonstrated no rotator cuff pathology or component loosening (Figs. 2-A and 2-B). He was treated conservatively and his symptoms resolved by six months.
Nine and a half years after the index procedure, he sustained a mechanical fall onto his operatively treated shoulder. Imaging demonstrated a periprosthetic fracture involving the humeral stem as well as an additional finding (Figs. 3-A, 3-B, and 3-C). The patient subsequently declined surgical management. Four months post-injury, the patient was satisfied with his outcome, with no pain despite the varus malunion of the periprosthetic fracture. Clinical examination demonstrated active forward flexion to 90°, external rotation to 30°, and 5/5 strength. The patient was able to return to all preoperative activities, and declined any further operative intervention.
The patient was diagnosed with partial dissociation of the humeral head component from the stem.
Proceed to Discussion >>Reference: Lee AH, Dilisio MF, Warner JJP. Late partial dissociation of a humeral head Morse taper associated with periprosthetic proximal humeral fracture: a case report. JBJS Case Connect. 2016 Apr-Jun;6(2):e34.
We report on a rare mode of failure of a shoulder arthroplasty through the Morse taper linkage nine and a half years after the index procedure. Modular humeral components have allowed a more anatomic placement of the humeral component that more effectively restores native patient anatomy. The linkage of the humeral head to the stem in most of the popular arthroplasty designs involves a Morse taper that allows the head to engage into the stem. Morse tapers and reverse Morse tapers have essentially become the universal linkage mechanism to mate the head to the stem in modern modular shoulder arthroplasty systems. We are not aware of any alternative commercially available head-stem linkage mechanism in the shoulder arthroplasty market. While dissociation of the Morse taper linkage has been reported in shoulder arthroplasty, nearly all of these reports have occurred in the first six weeks and were assumed to have been caused by surgeon error in seating the Morse taper mechanism.
A biomechanical study utilizing the Biomet Total Shoulder prosthesis demonstrated that the mean force required to dissociate the humeral head was 2926 N, and that fluid contamination of the taper could also prevent proper engagement of the taper. The present case, however, utilized the Zimmer Anatomical Total Shoulder System, which is designed with an eccentric Morse taper (unlike the Biomet stem). In addition, the stem of the Zimmer system is built ex vivo and has an outflow on the female end of the taper for fluid to escape, thus diminishing the likelihood of fluid contamination.
In the hip, Morse tapers are utilized to link the femoral head to the stem, and there have been several case studies of the disassembly of the modular femoral head component following attempted closed reduction. However, the hip is different from the shoulder in that more uniform compressive loads are applied to the proximal aspect of the femur, in contrast to the more physiologically unstable glenohumeral joint, which sees substantially more shear. These biomechanical differences may be relevant when comparing the Morse taper in hip arthroplasty with the Morse taper in shoulder arthroplasty.
We hypothesize that the patient’s fall resulted in an impaction force that was applied directly to the Morse taper and surrounding bone, resulting in disengagement of the humeral head from the stem, a periprosthetic proximal humeral fracture, and associated rupture of the fibrous capsule. It is possible that the head component was not fully seated; however, our initial and follow-up radiographs had demonstrated correct positioning and appropriate sizing. While corrosion has been well studied in hip arthroplasty, relatively little is known about its effects in the shoulder. Loads transmitted through the shoulder are lower than those in the hip; thus, we expect less force transmission through the humeral prosthesis.
At the six-month follow-up, the patient was doing well, and we expect that the implant will remain in its current position, given the patient’s baseline functional status. The loose component may result in increased metallosis, which may lead to increasing pain and discomfort; however, we are aware of only one such instance following total shoulder arthroplasty in the literature, which occurred within two years postoperatively.
Our report indicates that glenoid loosening and humeral stem loosening are not the only two modes of late hardware failure in total shoulder arthroplasty. Late dissociation of the humeral head from the stem after shoulder arthroplasty is possible and can be caused by a fracture. The shoulder surgeon should be mindful of this potential complication when evaluating periprosthetic proximal humeral fractures and should pay attention to detail in the evaluation of such patients.
Reference: Lee AH, Dilisio MF, Warner JJP. Late partial dissociation of a humeral head Morse taper associated with periprosthetic proximal humeral fracture: a case report. JBJS Case Connect. 2016 Apr-Jun;6(2):e34.
What is the diagnosis?
Adverse local tissue reaction related to corrosion at the head-neck junction
Particle-induced osteolysis
Displaced polyethylene glenoid component
Imaging features suggestive of periprosthetic infection
Partial dissociation of the humeral head component from the stem

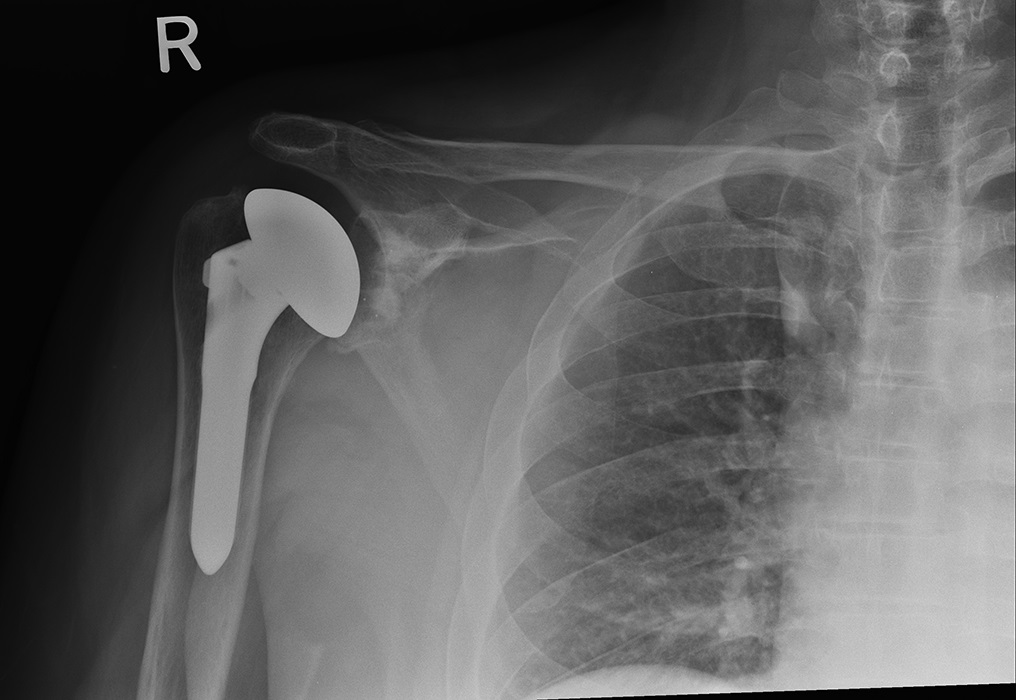
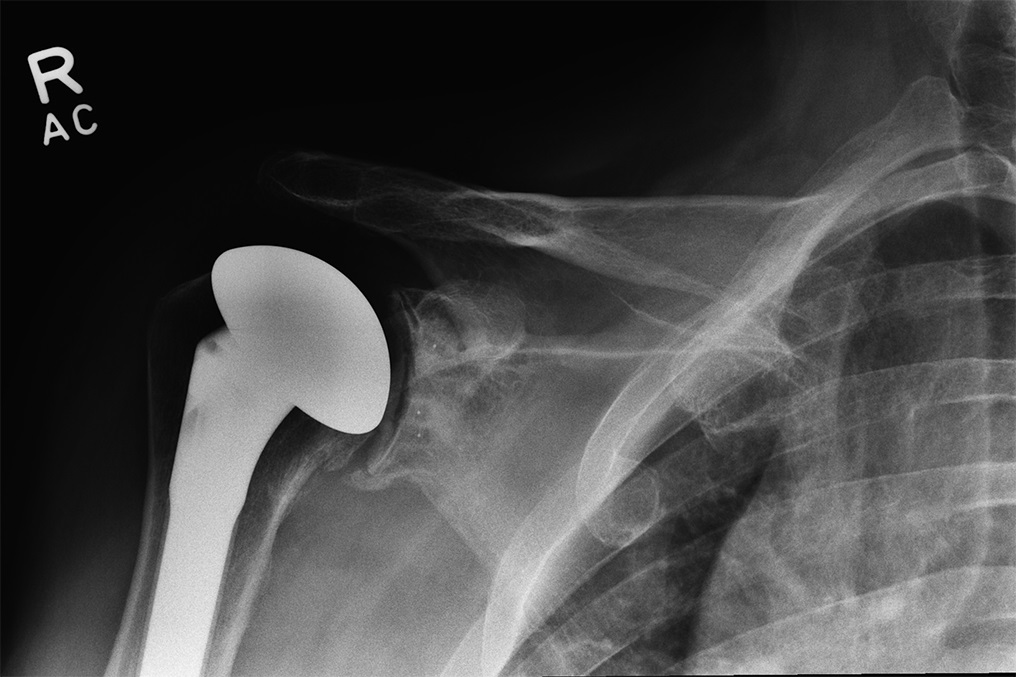
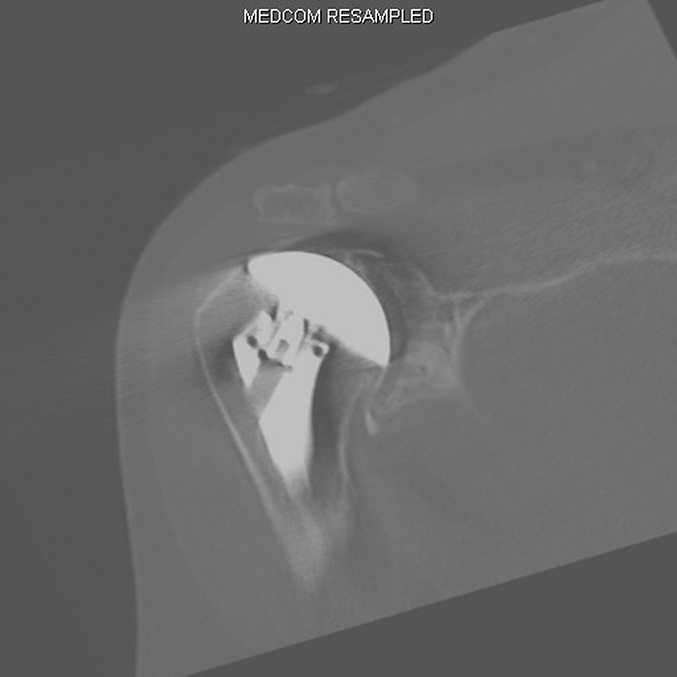
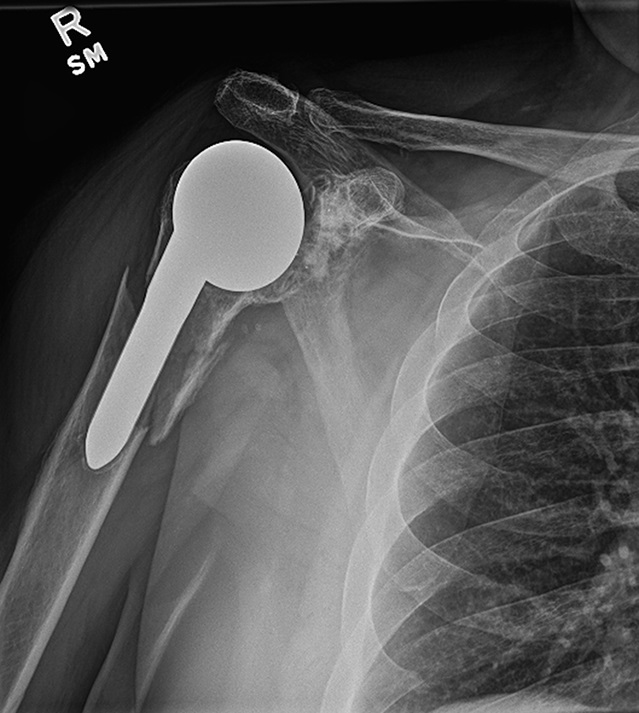
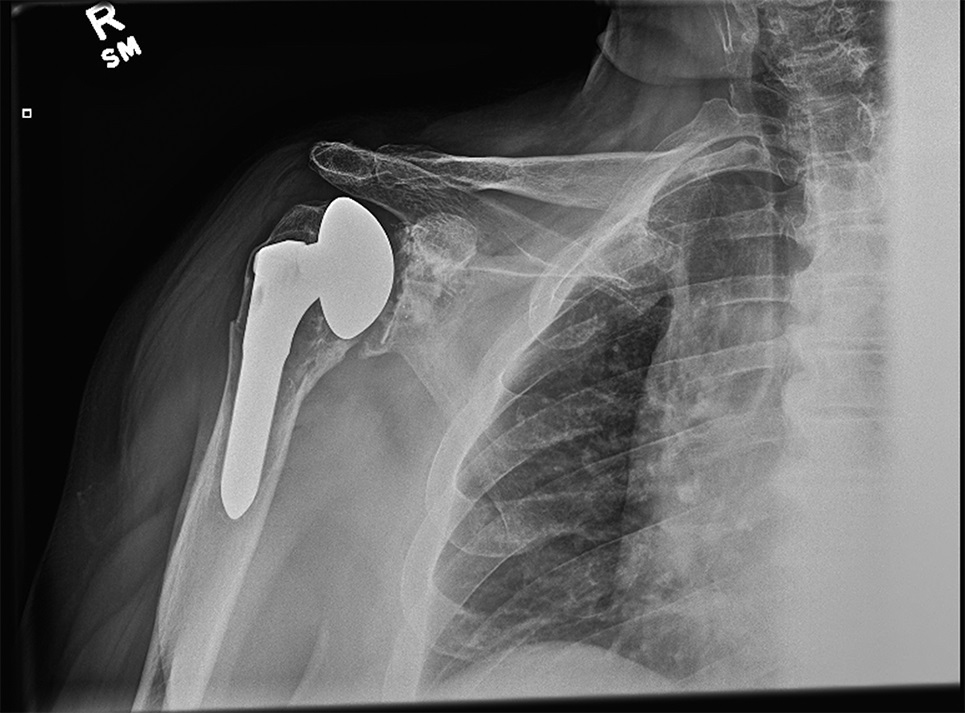
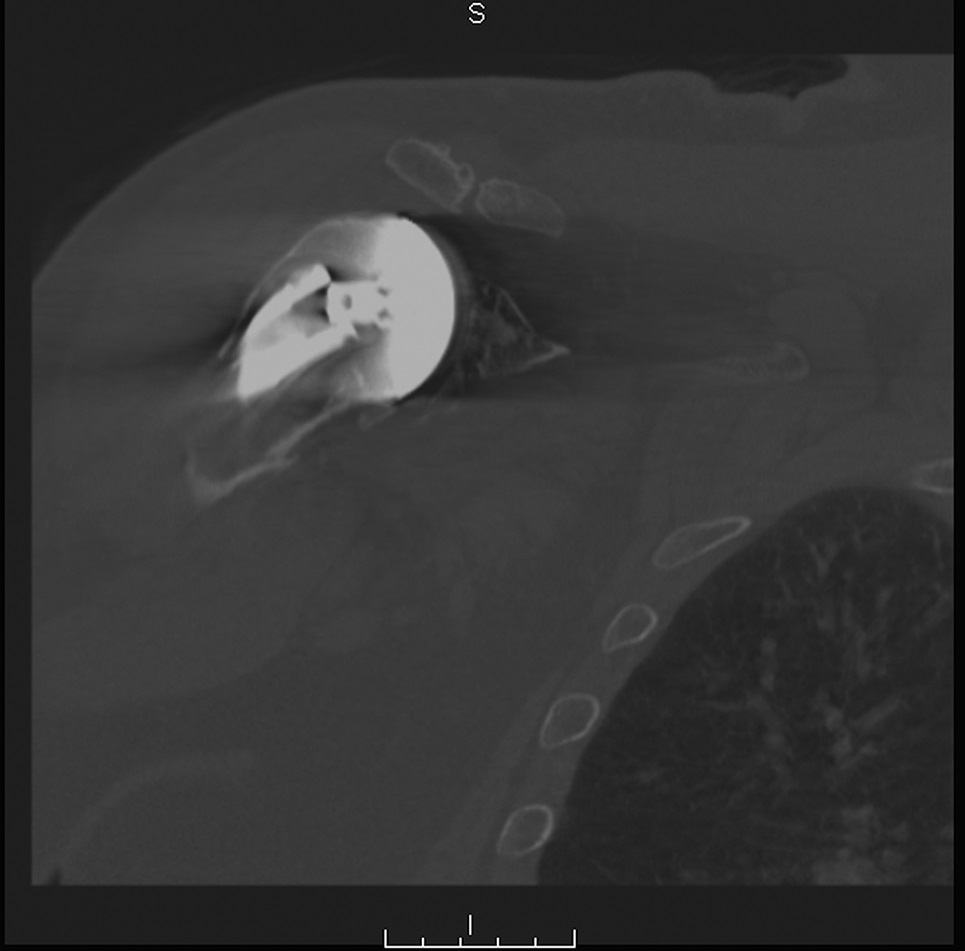
 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 3-C
Fig. 3-C