A 68-Year-Old Woman with Hip Pain Following a Fall
May 16, 2018
A 68-year-old woman presented with severe right hip pain several hours after a slip and fall from standing at home. She had undergone a primary total hip arthroplasty (THA) on the same side at an outside hospital approximately 15 months prior; there had been no previous dislocations. The indication for the primary THA was osteoarthritis, and it had been performed via a posterior approach. On examination, the patient was in a left lateral decubitus position and unable to lie flat secondary to severe pain. Neurologic function was difficult to fully assess secondary to pain. Sensation was grossly intact throughout the right lower extremity, and the feet were warm and well perfused. However, she was reluctant to move the right toes or the ankle because of pain, making it difficult to fully exclude the presence of a motor deficit. Radiographs demonstrated a posterior hip dislocation (Fig. 1-A).
The hip was easily reduced under conscious sedation with propofol with a single attempt, and was found to be stable by a post-reduction clinical examination in all directions (Fig. 1-B).
Following reduction, the patient was able to wiggle the toes, and sensation remained grossly intact. Additional assessment the next morning revealed improved pain, but absent plantar flexion and dorsiflexion of the ankle, absent extension of the big toe, and decreased sensation in the tibial and peroneal nerve distributions below the level of the ankle. We decided to obtain an urgent magnetic resonance imaging (MRI) examination of the hip with specialized metal-suppression sequences (GE Healthcare Optima MR450w). The MRI is shown in Figures 2-A through 2-D.
The MRI demonstrated tethering and entanglement of the sciatic nerve around the anterior aspect of the prosthetic femoral neck, as well as a large hematoma in the posterior soft tissues of the hip and the thigh (Figs. 2-A through 2-D and Fig. 3). The red arrow in Figure 2-A shows sciatic nerve fibers in an unexpected location: anterior to the femoral prosthetic component. The hematoma (asterisks) anterior to the gluteus maximus displaces the proximal sciatic nerve anteriorly.
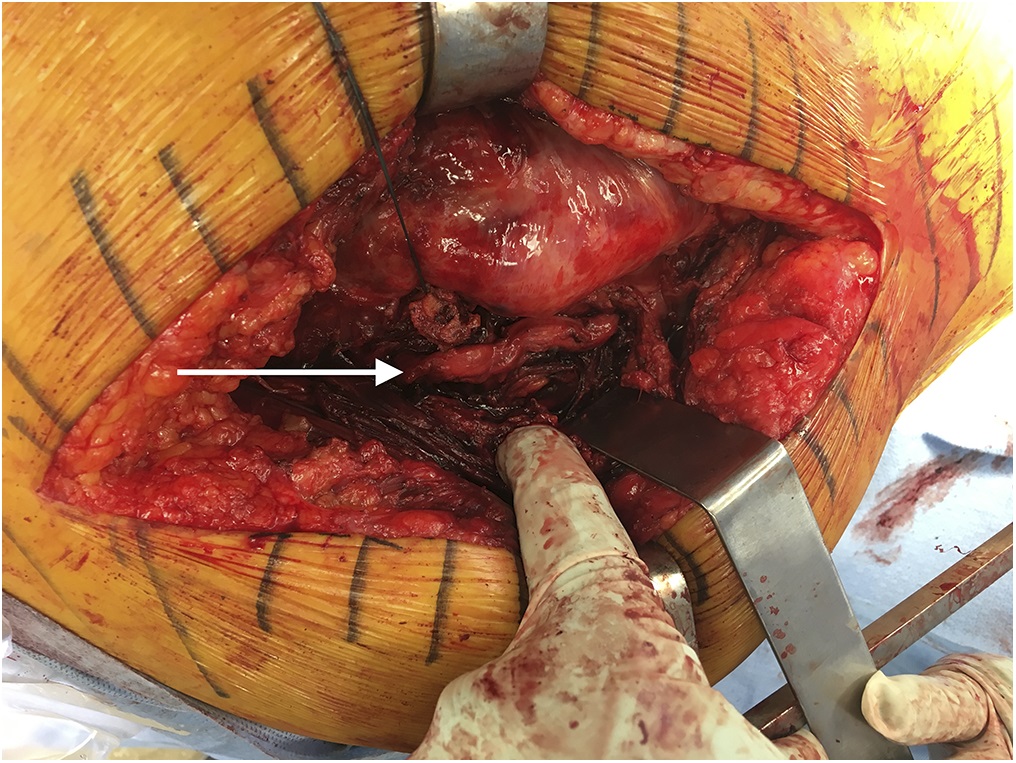
The patient was taken to the operating room later that evening for exploration and release of the sciatic nerve. A posterior approach was used with the old incision, with extension proximally and distally for better visualization. Dissection down through the fascia and gluteal muscles revealed a hematoma around the short external rotators, which was evacuated. The sciatic nerve was not found in its normal anatomic position with respect to the external rotators. Careful dissection was continued to the sciatic notch, and the nerve was found exiting the pelvis. The nerve was followed to the 12 o’clock position on the acetabulum. A high capsulotomy was performed, and reflection of the piriformis and external rotators revealed the sciatic nerve to be extremely attenuated and draped around the anterior aspect of the neck of the femoral component (Fig. 3-A). Distal dissection demonstrated that the remainder of the exposed sciatic nerve was structurally intact.
The hip was carefully dislocated while protecting the sciatic nerve. The femoral head and the neck were then elevated above the acetabular cup, allowing the entangled sciatic nerve to return posteriorly to its normal anatomic position. A stricture was noted where the nerve had been in contact with the implant. Additional exploration of the sciatic nerve was carried out proximally and distally, demonstrating a hematoma surrounding the nerve as it traveled distally into the posterior aspect of the thigh compartment. The hematoma was evacuated. There was no evidence of any other site of nerve damage or impingement. Revision to a dual mobility prosthesis was performed, and the revised hip was stable in all directions, without interposition of the sciatic nerve (Fig. 3-B).
Immediately postoperatively, the patient continued to have absent plantar flexion and dorsiflexion of the ankle, absent extension of the big toe, and an unchanged sensory deficit in the tibial and peroneal nerve distributions below the level of the ankle. An abduction pillow and knee immobilizer were used to avoid additional tension on the injured sciatic nerve from hyperflexion of the hip. She was discharged on postoperative day 2 to acute inpatient rehabilitation, where she was fitted with an ankle-foot orthosis. Three weeks postoperatively, a sciatic nerve palsy persisted, with no return of motor function or sensation. Electromyography and nerve conduction studies (EMG/NCS) were performed at that time to document the baseline nature of the sciatic nerve injury (i.e., localization, complete versus incomplete) and to determine whether the neurologic deficit was due to neurapraxia or a more severe anatomic disruption with axonotmesis or neurotmesis. EMG/NCS demonstrated substantial injury to the proximal aspect of the sciatic nerve involving all components. There was evidence of slight early reinnervation of the medial hamstring muscles, but otherwise there was no evidence of activity in any of the other muscles innervated by the sciatic nerve. NCS revealed total Wallerian degeneration of the large myelinated nerve fibers distal to the knee. These results suggested a poor prognosis for substantial recovery of motor function distal to the knee, although a repeat EMG/NCS 3 to 4 months later might have better detected early reinnervation. The patient was discharged home with services 2 days after the EMG/NCS. The last follow-up occurred 3 weeks after the surgery. She has since been lost to follow-up despite repeated attempts to contact her via telephone calls and voicemail messages.
Proceed to Discussion >>Reference: Cheung ZB, Patel AV, DeBellis N, Unis DB, Benitez CL. Sciatic nerve entanglement around a femoral prosthesis during closed reduction of a dislocated total hip prosthesis: the role of metal-suppression MRI: a case report. JBJS Case Connect. 2018 Jan-Mar;8(1):e3.
The reported rate of dislocation following THA varies, ranging from 2.4% to 3.2% following a primary THA, and rising to 4.8% to 7.4% after revision THA. More than half of all dislocations occur within the first 3 months postoperatively, and more than three-fourths occur within 1 year. Nerve injury is a known complication of hip dislocations, and the sciatic nerve is at particular risk of injury in posterior dislocations. The sciatic nerve can be acutely lacerated, stretched, compressed, or later encased in heterotopic ossification.
Risk factors for dislocation following THA include patient-specific characteristics such as advanced age, anatomic variations of the hip, metabolic bone disorders, neuromuscular conditions, inflammatory arthropathies, osteonecrosis of the femoral head, prior fractures or surgical procedures involving the hip, and noncompliance. Surgical risk factors, including approach, component positioning, soft-tissue tension, and surgeon experience, also have been shown to be associated with dislocation after THA.
Sciatic nerve palsy following closed reduction of a dislocated THA is rare. To our knowledge, there are only 7 documented cases in the literature. Lazansky reviewed 501 Charnley THAs, and reported 1 case of sciatic nerve palsy following closed reduction. The treatment and outcome were not described. Stockley and Bickerstaff, Leversedge et al., Chan et al., and Haque and Sundararajan described cases of sciatic nerve palsy following closed reduction, with intraoperative findings of sciatic nerve entrapment by the neck of the femoral component. Ng et al. described a case of complete sciatic nerve palsy following a difficult and prolonged closed reduction, with intraoperative findings revealing no evidence of sciatic nerve impingement or a compressive hematoma. Therefore, traction injury was proposed as the most likely cause of the sciatic nerve palsy. Lastly, Smith et al. described a case of sciatic nerve palsy in which operative exploration revealed compression of the sciatic nerve by a large hematoma. The neurologic sequelae in these previously documented cases varied, with only 1 patient regaining full nerve function.
In our patient, the sciatic nerve was entrapped around the femoral component, likely as the hip was being reduced. However, we cannot fully exclude the possibility that some degree of neurologic injury had been present prior to reduction since the patient was reluctant to move the ankle or the toes on presentation. To our knowledge, this case is the first description of a sciatic nerve palsy following closed reduction of a dislocation of a THA in which preoperative MRI with metal-suppression sequences demonstrated entanglement of the sciatic nerve around the femoral component, which was subsequently confirmed by intraoperative findings. This specialized metal MRI protocol consisted of a high-resolution proton-density metal artifact reduction sequence (PD-MARS) to evaluate the anatomic relationships of the soft tissue and the course of the sciatic nerve, as well as a short tau inversion recovery (STIR) sequence with high bandwidth to provide homogeneous fat tissue suppression and better evaluation for tissue pathology. The STIR sequence serves as a fluid-sensitive sequence to evaluate for fluid collections, hematomas, and periprosthetic fractures. With regard to evaluation of complications of total joint arthroplasties, this specialized MRI technique with metal-suppression sequences can provide greater signal at the bone-metal interface as well as improved surrounding soft-tissue detail compared with conventional MRI.
Normally, the sciatic nerve exits the pelvis via the greater sciatic foramen, where it courses anterior to the piriformis muscle. More inferiorly, the sciatic nerve courses posterior to the quadratus femoris and obturator internus muscles, anterior to the gluteus maximus, and it runs lateral to the semitendinosus muscle at the level of the ischial tuberosity. In our patient, we hypothesize that the large perineural hematoma seen intraoperatively and with MRI may have displaced the sciatic nerve anteriorly, which from an anatomic standpoint would make the nerve more likely to become entangled around the femoral component during reduction of a posterior dislocation.
In summary, it is imperative to assess and document neurovascular status before and after any attempts at manipulation of a dislocation of a THA because nerve injury may occur from the initial dislocation or the subsequent reduction maneuvers. In cases where sciatic nerve palsy is noted following closed reduction, we propose an emergency metal-suppression MRI examination to evaluate for sciatic nerve entanglement or compression. Long-term outcomes following sciatic nerve release or decompression are varied, but the literature suggests that neurologic recovery likely will be incomplete. Quick recognition and diagnosis of nerve entanglement is imperative to improve outcomes. Rehabilitation and bracing should begin as early as possible to prevent an equinus foot deformity.
Reference: Cheung ZB, Patel AV, DeBellis N, Unis DB, Benitez CL. Sciatic nerve entanglement around a femoral prosthesis during closed reduction of a dislocated total hip prosthesis: the role of metal-suppression MRI: a case report. JBJS Case Connect. 2018 Jan-Mar;8(1):e3.
What is the diagnosis?
Entangled sciatic nerve around the prosthetic femoral neck
Inflammatory pseudotumor impinging on the sciatic nerve
Partial sciatic nerve laceration
Peripheral nerve sheath tumor arising from the sciatic nerve
Changes consistent with tenosynovial giant cell tumor (pigmented villonodular synovitis)

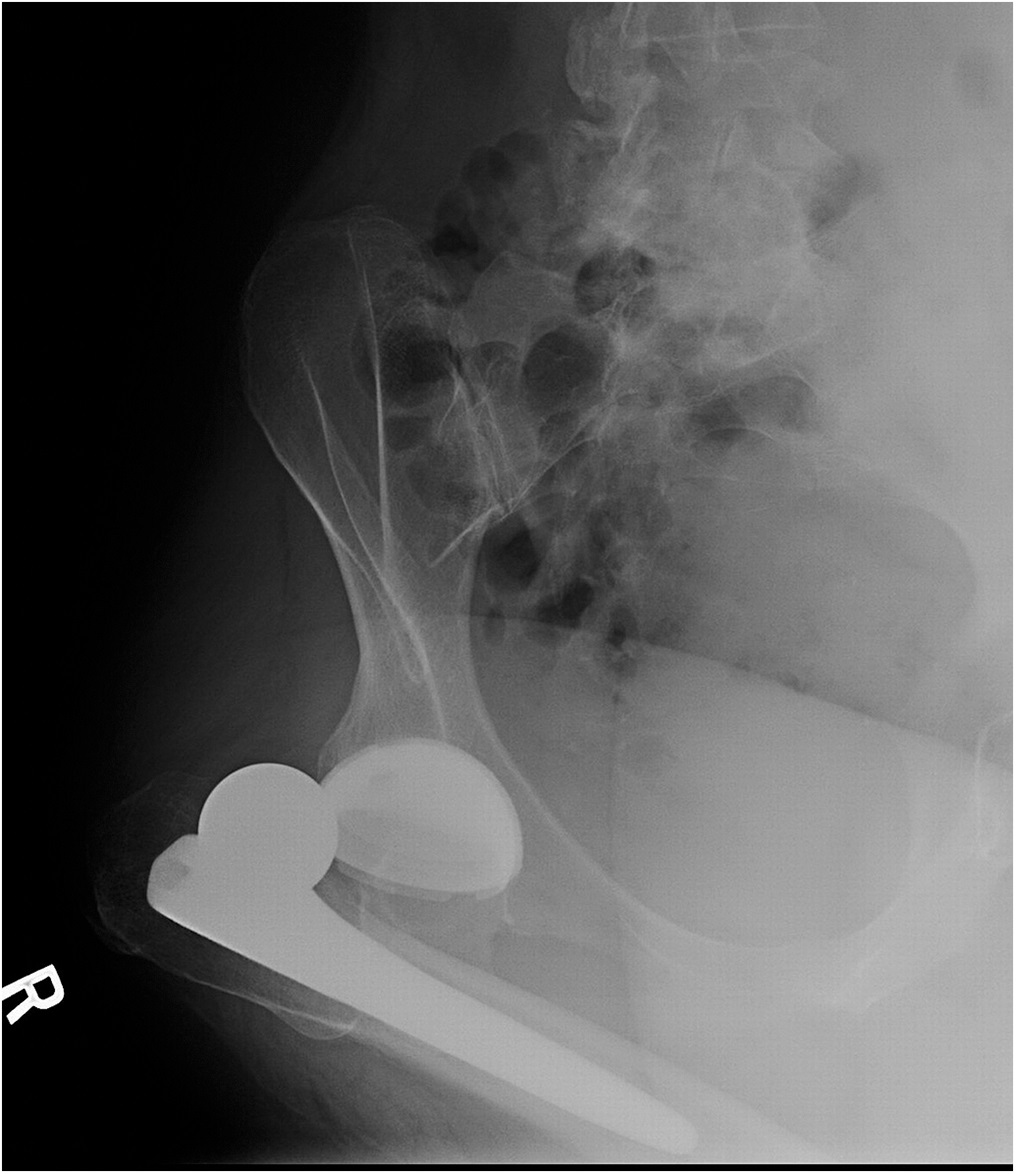
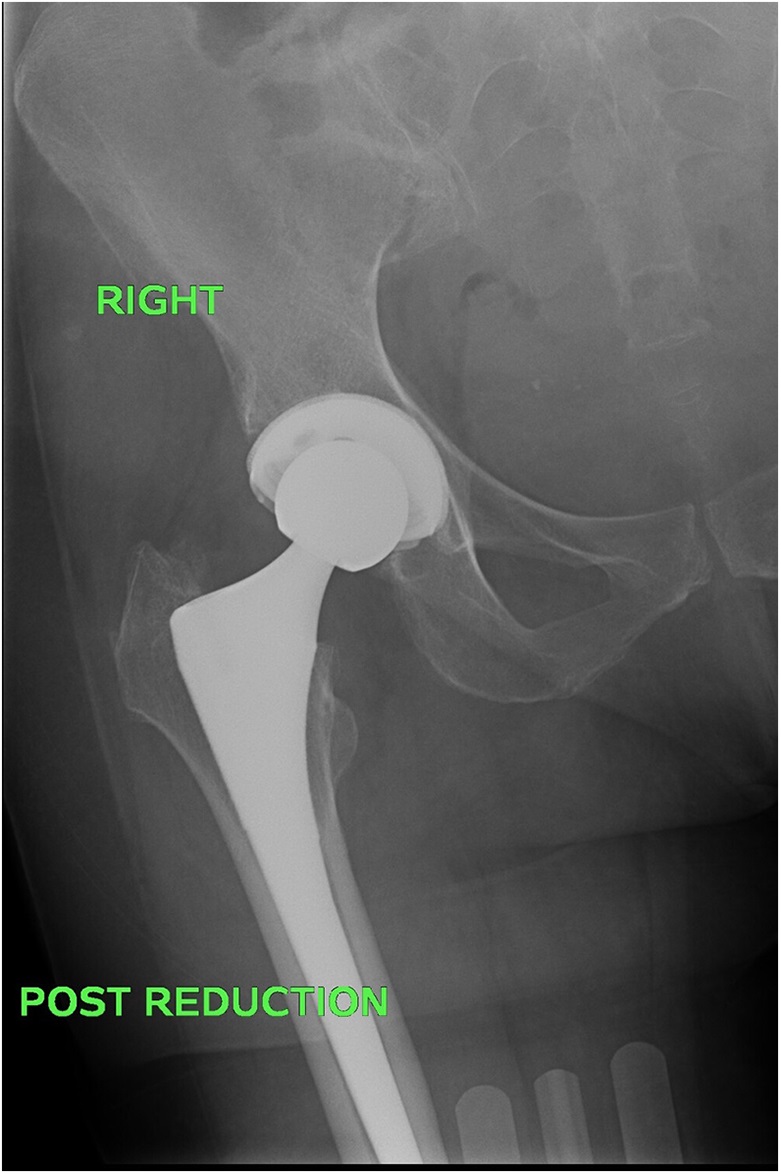
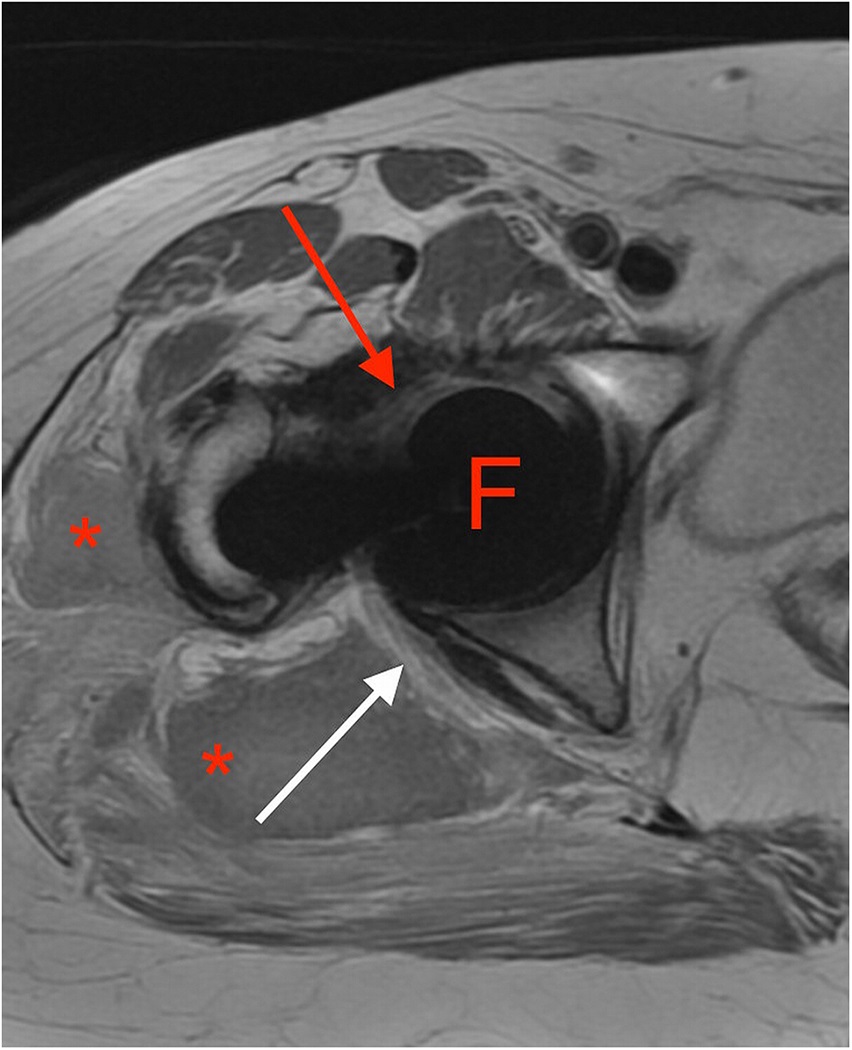


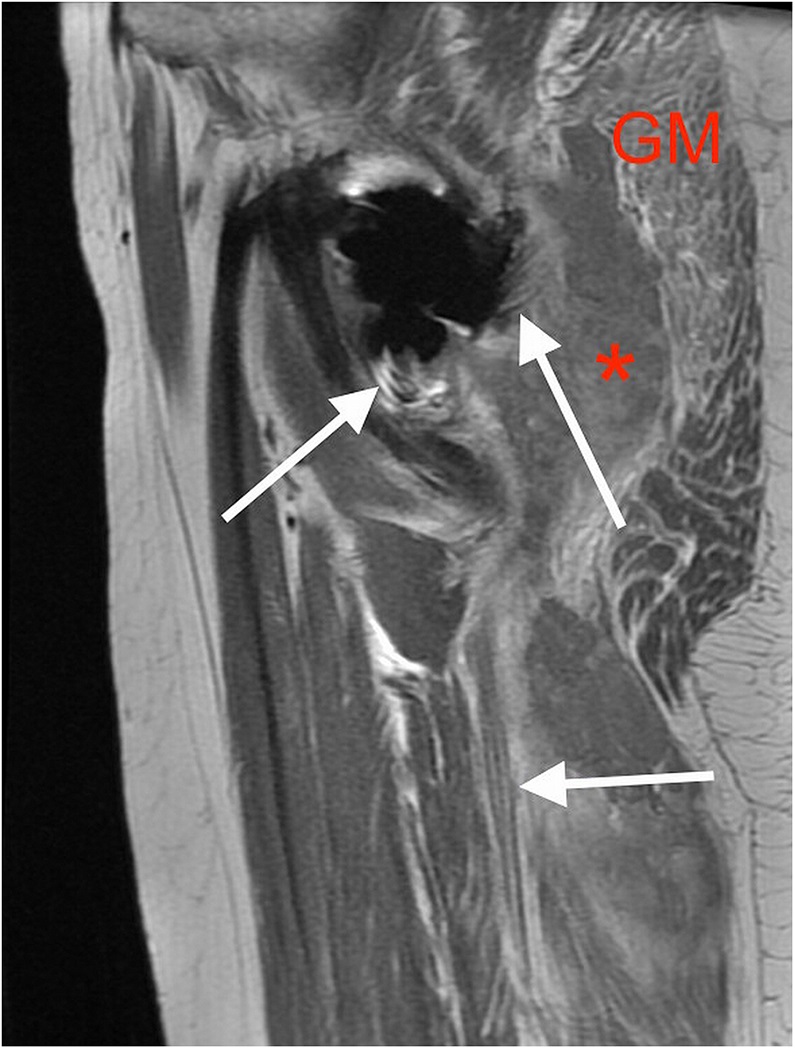
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B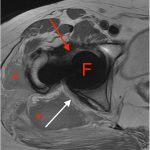 Fig. 2-A
Fig. 2-A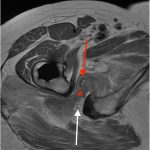 Fig. 2-B
Fig. 2-B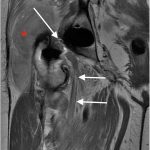 Fig. 2-C
Fig. 2-C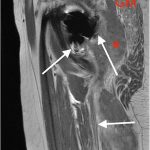 Fig. 2-D
Fig. 2-D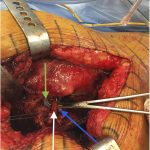 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B