A 75-Year-Old Man with Debilitating Leg Pain Following a Fall
December 19, 2018
A 75-year-old, fit, healthy, and active man had undergone a Birmingham Hip Resurfacing arthroplasty at the age of 61 years for painful osteoarthritis. For 14 years after the procedure, the resurfaced hip did not have any symptoms, and he was able to lead a physically active lifestyle, which included going to the gym and cycling for long distances. The medical history included a previous cardiac angiogram for atrial fibrillation, and the patient was on warfarin therapy.
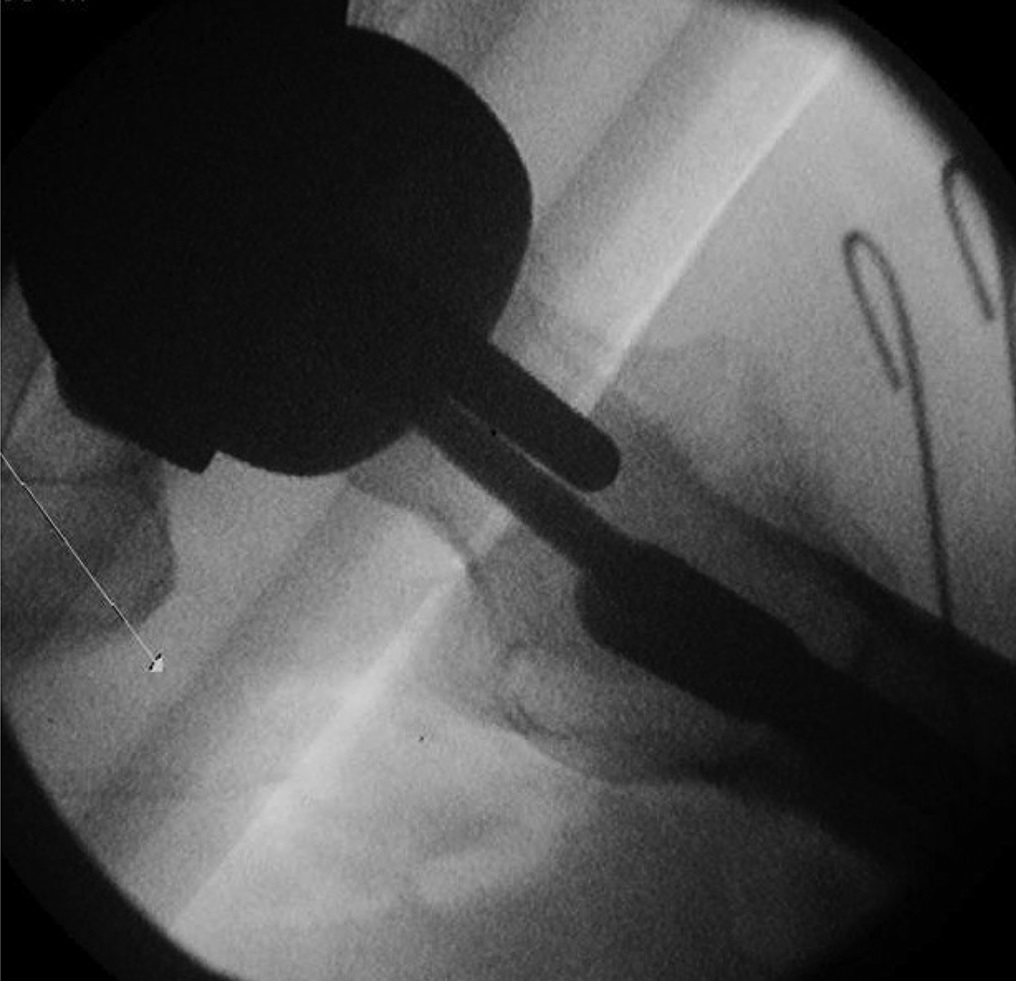
At the age of 75 years, the patient fell. On clinical examination, the left leg was extremely painful, and he was unable to bear weight or actively perform a straight leg raise. Radiographs are shown in Figs 1-A and 1-B.
Radiographs were interpreted as demonstrating an undisplaced periprosthetic trochanteric fracture of the proximal aspect of the femur. The Birmingham Hip Resurfacing implant was in a good position, was well-fixed, and had no evidence of loosening.
Because this was a minimally displaced femoral fracture of the proximal aspect of the femur, distal to a well-fixed and functioning resurfacing femoral component, in a relatively healthy 75-year-old man, we decided to attempt internal fixation with a reconstruction intramedullary nail. We recommended internal fixation with retention of the femoral component so that the patient could achieve immediate ambulation with the simplest operation, and anticipated that the fracture would heal in a good position and the implant would continue to function well. We did inform the patient that if this procedure were to fail, he would require a much more extensive revision total hip replacement procedure.
In the operating room, the patient was placed on a traction table. A Trochanteric Antegrade Recon femoral nail (Smith & Nephew) was inserted in the conventional manner. Under image intensifier guidance, the 2 proximal hip screws were placed in a way so as to avoid abutting the stem or undersurface of the femoral component (Figs. 2-A and 2-B). The preoperative assessment of the location of the prosthetic femoral stem was slightly posterior to the middle of the femoral neck. Therefore, the plan was to externally rotate the femoral nail by 5° during insertion so that the proximal locking screws placed through the nail would be in the anterior aspect of the femoral neck and avoid the Birmingham femoral stem.
Postoperatively, the patient described almost complete resolution of pain; he was able to mobilize with partial weight-bearing at 24 hours after surgery. At the 6-week follow-up, the patient was able to bear weight fully with no use of walking aids. At the 6-month follow-up, radiographs demonstrated good alignment with no collapse or fracture displacement (Figs. 3-A and 3-B). The 6-month and 1-year follow-ups confirmed excellent clinical and radiographic results. The patient had pain-free function, had full range of hip movements, and had returned to his previous active lifestyle.
Proceed to Discussion >>Reference: Chou DTS, Davis B. Trochanteric femoral fracture around a Birmingham hip resurfacing prosthesis: a case report and review of the literature. JBJS Case Connect. 2017 Jan-Mar;7(1):e7.
As a consequence of recent failures of some metal-on-metal hip arthroplasties, there has been a reduction in the number of Birmingham Hip Resurfacing procedures. Nonetheless, some surgeons still consider the Birmingham Hip Resurfacing prosthesis to be an excellent choice when used with the right patient, and these procedures continue to be performed.
Periprosthetic fractures around hip implants can be difficult to manage, and are likely to become more frequent because of the increased number of hip arthroplasties that are being performed. In principle, such fractures can be managed with either open reduction and internal fixation or revision hip arthroplasty, based on the integrity of the implants. Other factors to consider when deciding on the best treatment option include age, functional status, comorbidities, available surgical expertise, and equipment.
Mauffrey described 2 cases of successful nonoperative management of patients with minimally displaced trochanteric fractures below a Birmingham Hip Resurfacing implant. Skin traction was used for 6 weeks with both patients; they were allowed to partially bear weight at 6 weeks postoperatively, and fully bear weight at 4 months. Despite a slight malunion in 1 case, both of the patients had a good final outcome.
To our knowledge, there have been 5 reports of surgical fixation of trochanteric femoral fractures beneath a Birmingham Hip Resurfacing implant. Aning et al. used a reconstruction nail (similar to the one that we used) to fix a complex multifragmentary fracture of the proximal aspect of the femur, which was augmented with cables. The fracture united, and the patient did very well without the need for additional surgery. Our patient had an implant that would allow hip screws that could pass around the stem of the prosthesis into the femoral head.
Whittingham-Jones et al. described using a contoured, broad AO (Arbeitsgemeinschaft für Osteosynthesefragen) dynamic compression plate (DCP) to fix a comminuted subtrochanteric femoral shaft fracture below a well-fixed Birmingham hip implant. After an initial period of non-weight-bearing, the patient achieved full union at 5 months, and was then able to return to sporting activity. However, during this period, she developed a deep vein thrombosis that required medical treatment.
In the cases of periprosthetic fracture described above, the authors felt that maintenance of the existing, well-functioning hip resurfacing implant was likely to provide a better long-term outcome for the patient than revision hip arthroplasty. They highlighted the importance of avoiding the stem and cement mantle when inserting screws into the femoral head. This is complicated by the metal interference of the resurfacing implant as seen on the image intensifier. However, if performed with care, attention, and a preoperative plan, avoiding the stem and cement mantle can be easily achieved without causing damage to the prosthesis. With our patient, the preoperative assessment found the location of the prosthetic femoral stem to be slightly posterior to the middle of the femoral neck. Therefore, our plan was to externally rotate the femoral nail by 5° during insertion so that the proximal locking screws placed through the nail would be in the anterior aspect of the femoral neck, thereby missing the femoral stem of the prosthesis. Aning et al. suggested that tactile and audio feedback can assist in performing this part of the procedure.
In conclusion, due to the inherent active nature of many of these patients, it is likely that traumatic periprosthetic fractures around a Birmingham Hip Resurfacing implant may become more prevalent. In a patient with a previously well-functioning hip resurfacing implant, we feel that internal fixation rather than revision hip arthroplasty offers good clinical and radiographic outcome.
Reference: Chou DTS, Davis B. Trochanteric femoral fracture around a Birmingham hip resurfacing prosthesis: a case report and review of the literature. JBJS Case Connect. 2017 Jan-Mar;7(1):e7.
What is the diagnosis?
Osteonecrosis beneath the resurfacing implant
Periprosthetic osteolysis likely due to metal wear debris
Periprosthetic femoral neck fracture
Periprosthetic trochanteric fracture
Metal-on-metal pseudotumor


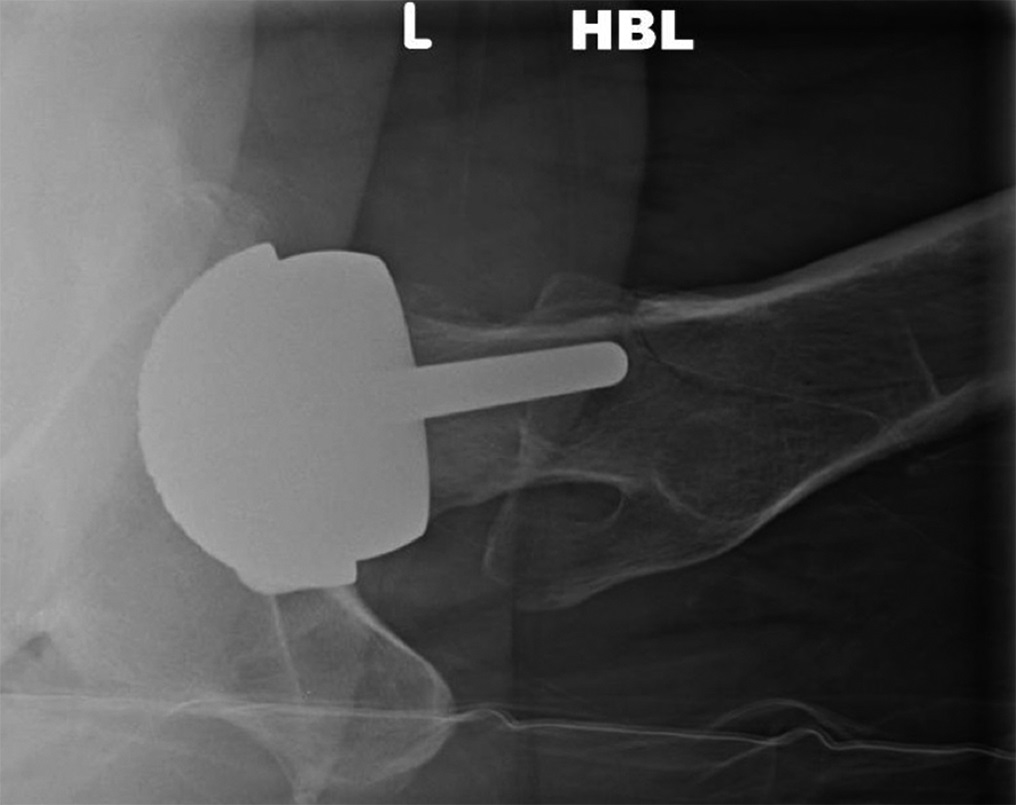
 Fig 1-A
Fig 1-A Fig 1-B
Fig 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B