A 39-year-old, left-hand-dominant, male police officer presented to the outpatient clinic 3 weeks after sustaining an injury to the right wrist. During a recreational softball game, the patient had run into a fence while attempting to make a catch with his gloved right hand. Immediately, he experienced pain and swelling about the ulnar aspect of the wrist. He was evaluated in a local emergency department, where radiographs of the right hand were read as negative (Figs. 1-A, 1-B, and 1-C). Subsequently, he was referred to our outpatient orthopaedic clinic for follow-up.
On presentation to our clinic, the patient noted persistent volar, ulnar-sided pain in the right wrist. Physical examination revealed tenderness to palpation of the hook of the hamate; however, there was no pain with resisted small finger flexion. He had equivocal tenderness about the triangular fibrocartilage complex (TFCC) but had a positive TFCC grind. Motor function and sensation were intact to the radial, ulnar, and median nerves. The radial and ulnar pulses were palpable with good digital capillary refill.
Radiographs were concerning for a fracture. Computed tomography (CT) scans with axial, coronal, and sagittal reconstructions were obtained (Figs. 2-A through 2-F) and showed a comminuted fracture.
After diagnosis by CT, magnetic resonance imaging (MRI) was acquired to further characterize the acuity of the fracture and to identify any surrounding soft-tissue injury (Figs. 3-A, 3-B, and 3-C). On MRI, the bone and its soft-tissue attachments demonstrated edema that was consistent with a subacute injury. Otherwise, the contents of the carpal tunnel were normal.
Imaging showed that the body of the hamate did not show the osseous edema that might be expected in the setting of a fractured hook of the hamate. Instead, the imaging studies were interpreted as showing a comminuted fracture of the os hamulus.
Given the persistent ulnar-sided hand pain and unsuccessful nonoperative management with splinting for 8 weeks, the patient elected to undergo an open surgical excision of the os hamulus. With use of a volar approach, all of the fragments of the fractured os were isolated and completely excised. The ulnar nerve was found to be intimately involved with the fragments, and a neurolysis of the nerve was performed.
Postoperatively, the wrist was immobilized for 2 weeks. The pain improved, and at 2 months after surgery, the patient returned to full-duty work as a police officer. At the latest follow-up, at 6 years after surgery, he was asymptomatic and had achieved a full functional recovery.
Proceed to Discussion >>Reference: Graham JG, Matzon JL, Czachor B, Lucenti L, Beredjiklian PK. Fracture of an os hamulus proprium: a case report. JBJS Case Connect. 2019 Jan-Mar;9(1):e16.
Accessory bones are usually the result of a secondary ossification center that does not fuse with its associated bone. O’Rahilly and Gardner reported the prevalence of accessory ossicles in the carpus to be between 0.4% and 1.6%, and little information exists in the literature regarding these carpal abnormalities.
To our knowledge, few studies have examined the os hamulus. These accessory bones, which are associated with the hamate, include the os hamulus proprium, the os hamulare basale, the os hypotriquetrum, the os epitriquetrum, the os ulnare externum, the os vesalianum manus, the os gruberi, and the os capitatum secundarium. The os hamulus proprium is a secondary ossification center in the hook of the hamate that does not fuse with the hamate body. It is located in the palmar aspect of the mid-body, where the hook is usually positioned. For this reason, it can easily be confused with a hook of the hamate fracture or a nonunion. Bianchi et al. described an os hamulus that appeared to be a fractured hook of the hamate, and emphasized the importance of advanced imaging in making the correct diagnosis. More recently, Kobayashi and Mara reported a case of a symptomatic unilateral os hamulus proprium that was diagnosed by CT of the wrist.
Regarding the timing of the splinting with our patient, we believe that 8 weeks was a sufficient time frame for nonoperative treatment, with the understanding that this was a subjective decision based on the rarity of the case and the lack of literature for guidance. While repeat CT would have rendered some information regarding fracture-healing, we felt that the cost and exposure to radiation of repeat CT would not change the management of the patient, especially given the ongoing symptomatology. Based on the intraoperative findings and the degree of nerve involvement, we felt that a neurolysis was necessary. We performed a simple epineural neurolysis, and there were no complications secondary to the procedure.
We have described a patient with the unusual diagnosis of a fractured os hamulus proprium. We were unable to identify other reports in the literature detailing this rare clinical problem. Following unsuccessful nonoperative management, surgical excision of the fractured fragments and an ulnar neurolysis led to complete and sustained symptom resolution.
Reference: Graham JG, Matzon JL, Czachor B, Lucenti L, Beredjiklian PK. Fracture of an os hamulus proprium: a case report. JBJS Case Connect. 2019 Jan-Mar;9(1):e16.
What is the diagnosis?
Fracture of the scaphoid
Fracture of an os hamulus
Fracture of the hook of the hamate
An os paratrapezium
Fracture of the lunate




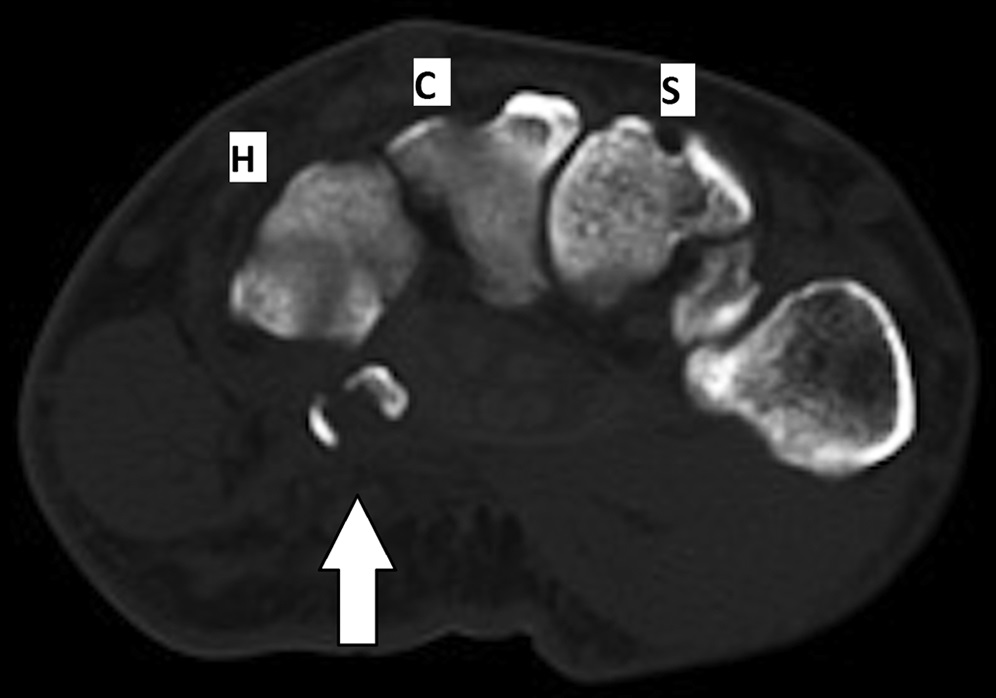

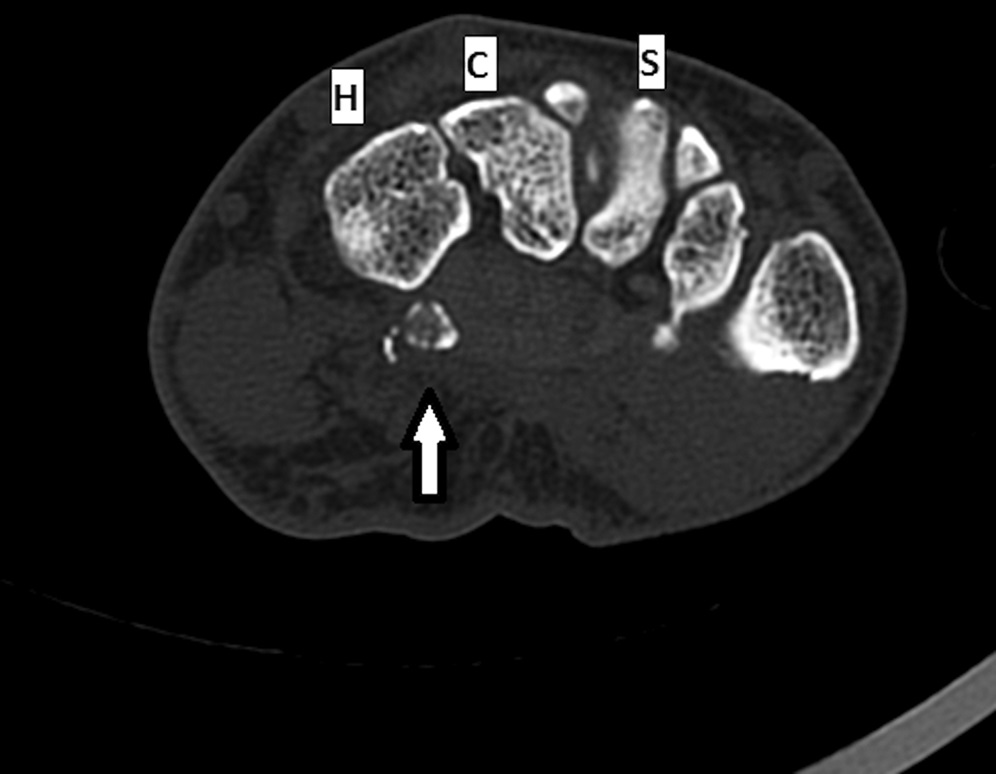


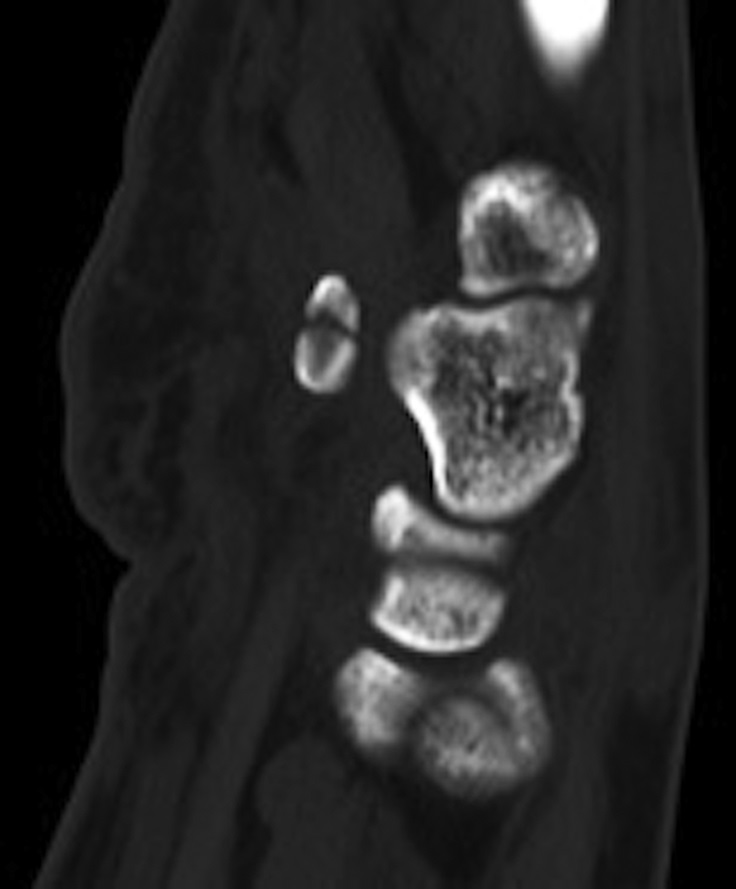
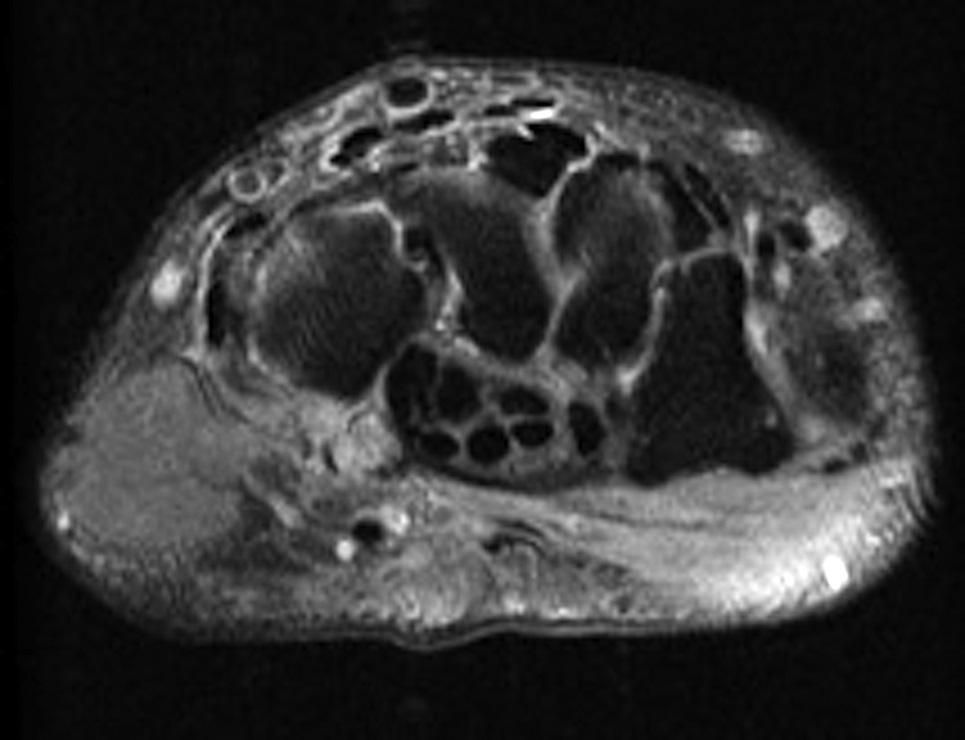
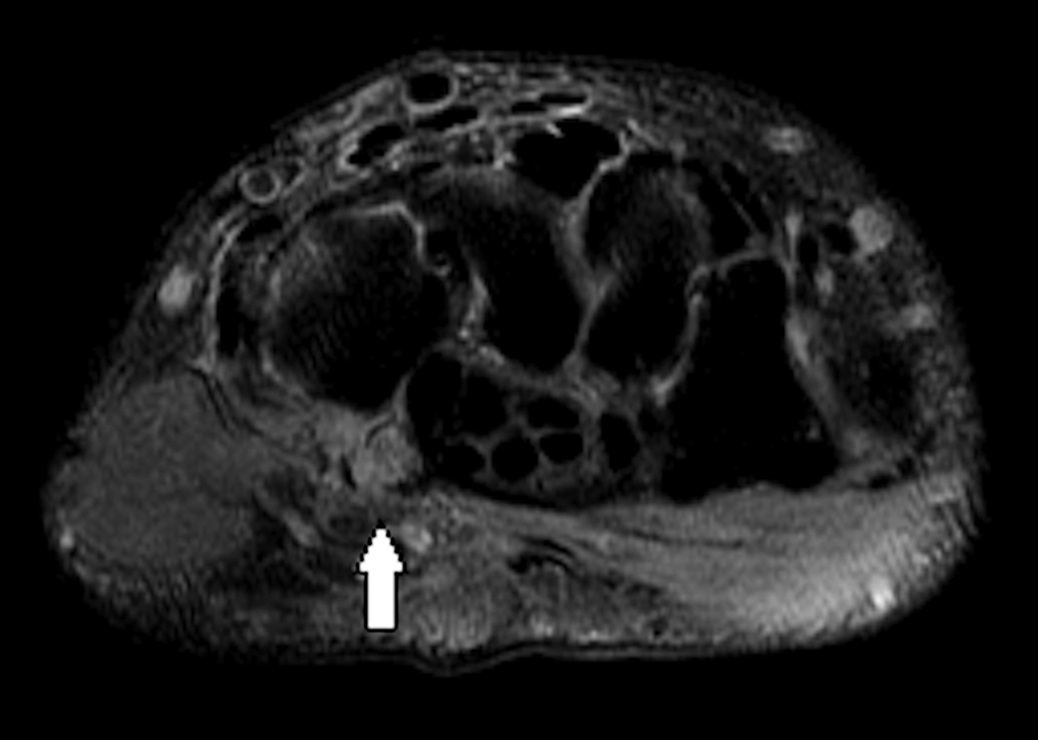
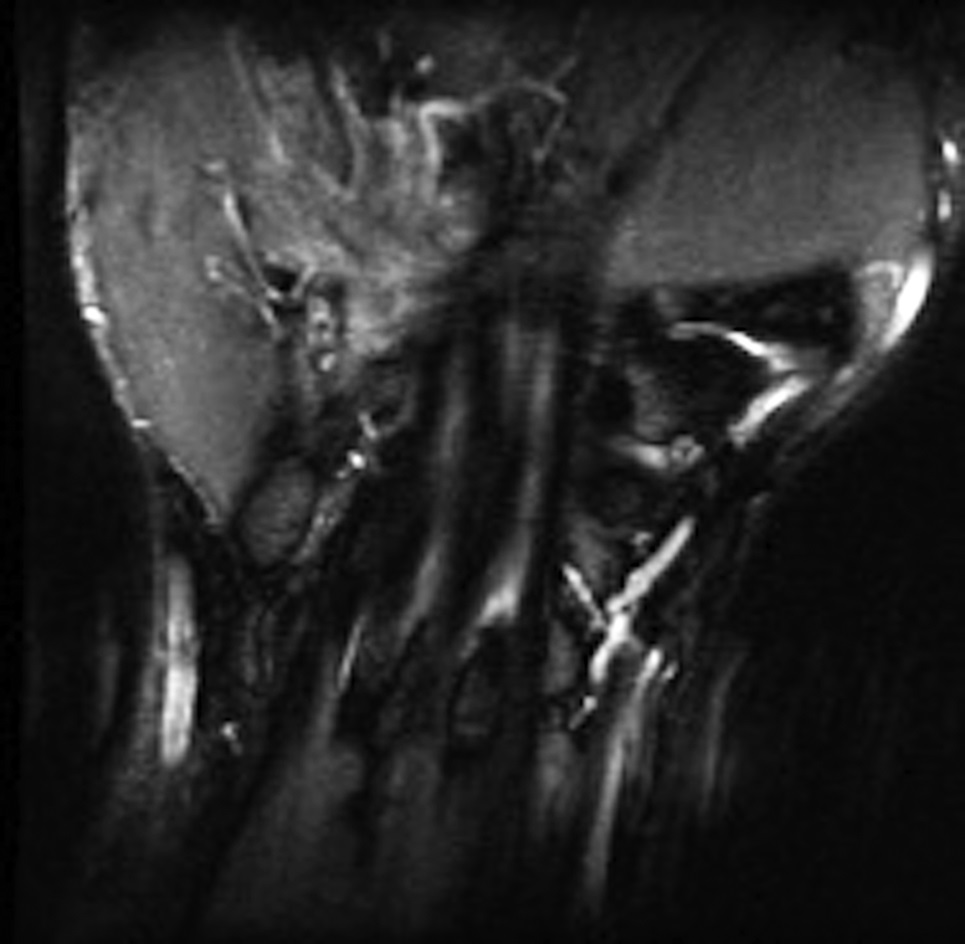
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 2-C
Fig. 2-C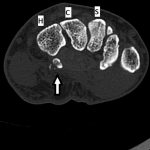 Fig. 2-D
Fig. 2-D Fig. 2-E
Fig. 2-E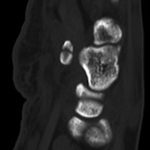 Fig. 2-F
Fig. 2-F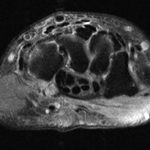 Fig. 3-A
Fig. 3-A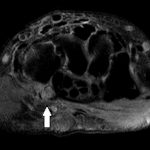 Fig. 3-B
Fig. 3-B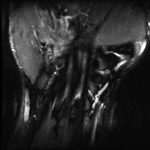 Fig. 3-C
Fig. 3-C