A 12-Year-Old Boy with Hip Pain Following a Fall
April 3, 2024
A 12-year-old adolescent boy with a medical history of sickle cell trait presented to the emergency department 1 day after tripping over a tree stump and catching himself on the foot, causing immediate left hip pain. He had not fallen or sustained any direct hip impact. After the injury, he reported being unable to bear weight on the involved extremity and he described severe groin pain with radiation down the medial thigh. The morning before presentation, the patient began feeling ill with coughing, congestion, and fever, which was 102.4°F (39.1°C) determined upon arrival. The patient’s father reported that the patient had not had any hip or groin symptoms previously, but stated that his siblings at home were experiencing cold-type symptoms over the previous few weeks and that the patient was completely up-to-date on all recommended vaccinations and had no endocrine history. The patient was not obese; he had a body mass index of 25 kg/m2.
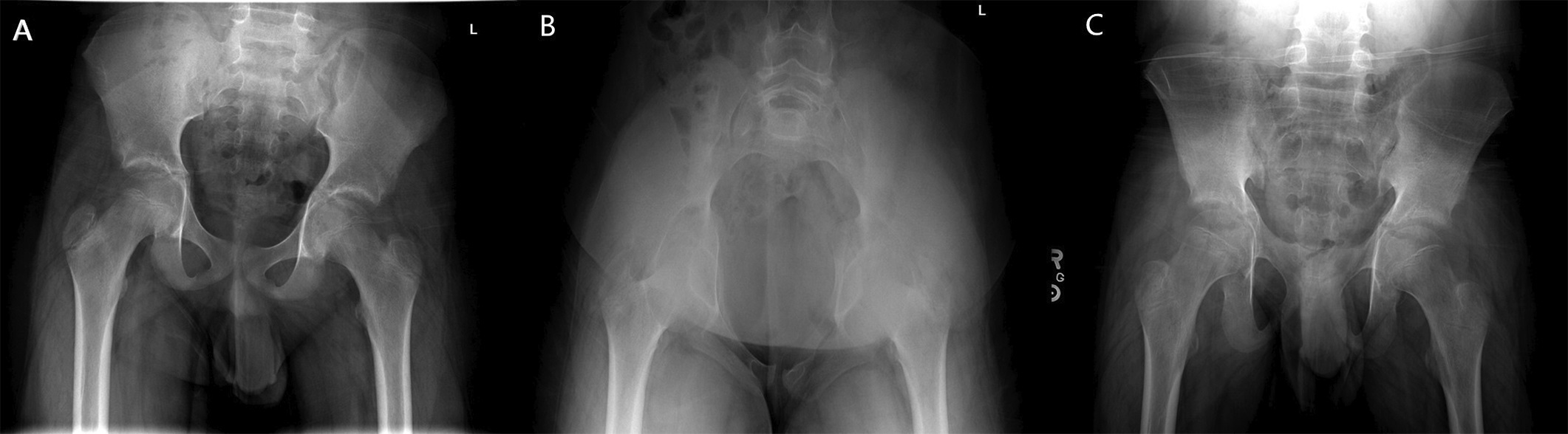
The initial inflammatory laboratory tests were mildly elevated, with a white blood cell count of 8,600 cells/mL, an erythrocyte sedimentation rate of 13 mm/hr, and a C-reactive protein of 6.8 mg/L; the patient also had a negative COVID-19 test. The examination did not reveal any obvious deformity, swelling, erythema, or warmth about the groin or the hip. Exquisite tenderness was elicited with passive internal and external rotation of the hip. The patient also reported pain with deep flexion of the hip and no pain with range of motion of the knee. Initial radiographs, including anteroposterior and lateral views of the femur and anteroposterior and frog-leg lateral views of the pelvis, were negative for fracture, instability, or slipped capital femoral epiphysis (Fig. 1).
The patient subsequently underwent magnetic resonance imaging (MRI) scans with contrast of the hip, which revealed an intact labrum and capsule with a robust, edema-like signal and postcontrast enhancement within the ischium and an effusion within the hip joint, concerning for osteomyelitis or septic arthritis (Fig. 2). Areas of low-signal intensity and nonenhancement were seen within the ischium along the acetabulum and were concerning for osteonecrosis (Fig. 2). Two sets of peripheral blood culture specimens were obtained, and the patient was scheduled to receive an ultrasound-guided aspiration and computed tomography (CT)-guided biopsy of the hip.
The ultrasound-guided aspiration revealed a hip effusion and returned 3 mL of sanguineous fluid. Substantial clotting was present, which precluded an accurate cell count. Culture specimens were held for 5 days, and no organisms grew on culture.
The patient then had a CT-guided biopsy (Fig. 3), followed by oblique Judet view radiographs of the pelvis (Fig. 4).
The CT scan made at the time of the biopsy was interpreted as showing a nondisplaced left posterior-wall acetabular fracture with extension into the triradiate cartilage. The subsequent pelvic radiographs also showed a nondisplaced posterior-wall acetabular fracture. The final biopsy results did not show any evidence of osteomyelitis.
After the patient experienced a resolution of fever, nonoperative management of the fracture was pursued. The patient was discharged 48 hours after admission with instructions for toe-touch weight-bearing of the left lower extremity and ibuprofen as needed for pain. Chemical venous thromboembolism prophylaxis was not prescribed.
The patient returned for follow-up 2 weeks later with decreased groin pain and improved active and passive range of motion of the hip with just slight discomfort with internal rotation. Interval radiographs revealed stable alignment of the posterior-wall fracture (Fig. 5). The patient then advanced to partial weight-bearing at 1 month after discharge and returned to full weight-bearing without complication at 3 months, with full range of motion and no reported pain.
Proceed to Discussion >>Reference: Compton T, Credille K, Loeffler T, Graf A, Van Valin S. Posterior wall acetabular fracture after low-energy trauma masquerading as infection: a case report. JBJS Case Connect. 2023 Aug 24;13(3).e23.00228.
Acetabular fractures are rare injuries in children and are most often seen in the setting of polytrauma. The most common mechanism is a motor vehicle collision, with 68% of pediatric acetabular fractures being associated with pelvic ring injury and 16% being associated with hip dislocation. Isolated acetabular fractures are even more uncommon and most often occur after ground-level falls or nonspecific sports injuries. These events can cause fracture from axial loading of the acetabulum, with or without hip dislocation. As seen in our patient, such isolated injuries after minimal trauma often cause only nonspecific symptoms such as groin pain and an inability to bear weight. Given their rarity and overlapping symptoms with other, more common causes of pediatric groin pain including infectious etiologies (e.g., septic arthritis, osteomyelitis, and transient synovitis), isolated acetabular fractures can be difficult to diagnose and require a high index of suspicion.
When doing a workup for a child with groin pain after a traumatic injury, we now recommend radiographs with Judet views in addition to radiographs with standard anteroposterior pelvic views to help to better visualize the pelvis and rule out an occult acetabular fracture. These views should be included with standard hip radiographs, including a frog-leg lateral view to rule out femoral neck fracture, slipped capital femoral epiphysis, and other traumatic etiologies of pediatric hip pain. Although these views often will not be made on the initial assessment, studies have shown that pediatric acetabular fractures can be missed on primary radiographs 22% to 80% of the time, highlighting their importance in this setting. Advanced imaging may be helpful in certain cases; however, it does present certain drawbacks, including cost and the potential need for anesthesia. MRI scans can help to identify occult fractures and to characterize physeal involvement of fractures, but nonspecific edema and enhancement can also mimic septic arthritis and osteomyelitis, as was seen in our case. CT scans can provide better details of bony anatomy for fractures not visualized on radiographs but come at the risk of radiation exposure and have previously been shown to affect management in only 3% of pediatric acetabular fractures. When considering CT-guided biopsy and aspiration, as was used in our case, many complications exist with undergoing anesthesia and the possibility of introducing a secondary infection into the joint. Interestingly, in our case, it was the CT-guided biopsy that ultimately led us to the correct diagnosis because the initial radiographs and MRI scans were falsely negative. Although the MRI scans could possibly have made the diagnosis with a different interpretation or MRI protocol, fractures can be challenging to detect on MRI scans if there is minimal or no displacement. Furthermore, the sensitivity of MRI in the detection of occult acetabular fractures and the use of different MRI protocols have not been studied in this setting because MRI is not part of the recommended evaluation for acetabular fractures.
The initial differential diagnosis for pediatric groin pain in the absence of substantial trauma typically includes slipped capital femoral epiphysis, septic arthritis, and transient synovitis. As a result of the patient having a fever and having an inability to bear weight, the patient met 2 of the 4 Kocher criteria, giving him roughly a 40% probability of having septic arthritis. In addition, the patient had slightly elevated inflammatory markers, although below the threshold to meet the Kocher criteria. Paired with an MRI scan concerning for infection and osteonecrosis, it can easily be understood why our most likely diagnosis at that point was an infectious hip etiology. However, on reviewing the patient’s history, many of his family members had been experiencing upper respiratory symptoms and fevers. The fact that the patient had immediate hip pain and an inability to bear weight after a traumatic event could have warranted further traumatic workup and consideration. In addition, there is a possible implicit bias toward ruling out an acetabular fracture in a differential when a lower-energy trauma occurs because of the scarcity of occurrences and lack of literature. However, there are several previously published case reports. In 1 combined case report, a 16-year-old adolescent boy who had sustained a fall on the buttock during soccer and an 11-year-old adolescent girl who had sustained a direct fall onto the hip both presented with acetabular fractures with extension into the triradiate cartilage, of which the 16-year-old adolescent boy was delayed in diagnosis because of the low-energy mechanism. Another case report, although in a skeletally mature individual, presented a 26-year-old man who sustained a posterior-wall acetabular fracture without falling, similar to our patient, after a cutting movement playing basketball likely directing the femoral head into the posterior wall like our patient’s planting movement of the left lower extremity to stabilize himself while stumbling. This further highlights the importance of putting patients’ orthopaedic symptoms in the context of their entire presenting history and maintaining a broad differential, especially with a recent traumatic mechanism.
In conclusion, acetabular fractures are rare injuries in the pediatric population that can often be difficult to diagnose. Diagnosis becomes even more difficult in patients without other associated injuries, minimal traumatic history, and symptoms of common pediatric illnesses such as upper respiratory infection. Therefore, one should include acetabular fracture on the differential diagnosis of pediatric groin pain and pursue dedicated radiographic Judet views to ensure prompt diagnosis and treatment when there is any suspicion for traumatic etiology.
Reference: Compton T, Credille K, Loeffler T, Graf A, Van Valin S. Posterior wall acetabular fracture after low-energy trauma masquerading as infection: a case report. JBJS Case Connect. 2023 Aug 24;13(3).e23.00228.
What is the diagnosis?
Osteonecrosis associated with sickle-cell trait
Posterior-wall acetabular fracture
Osteomyelitis
Septic arthritis
Changes suggestive of Langerhans cell histiocytosis

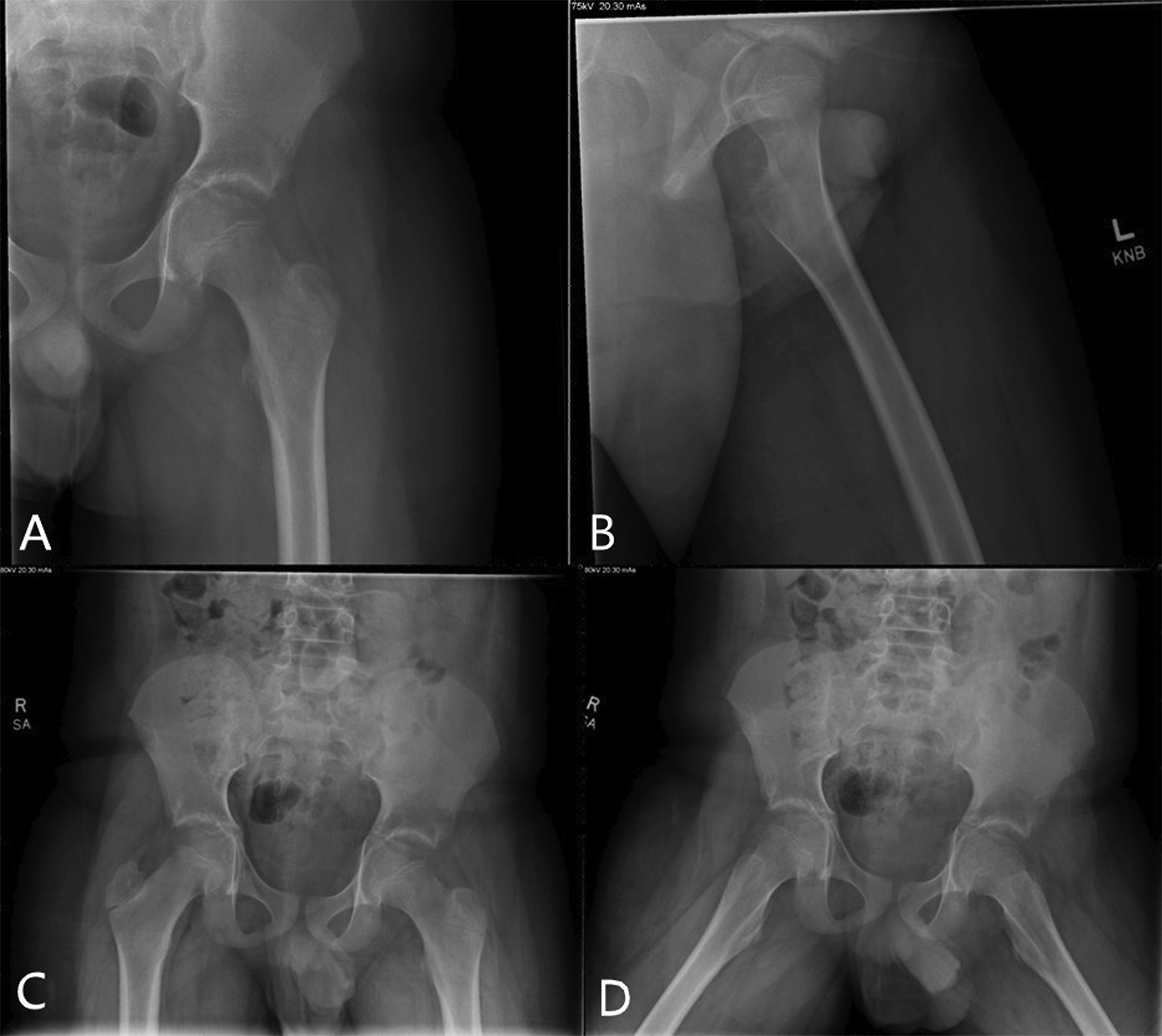
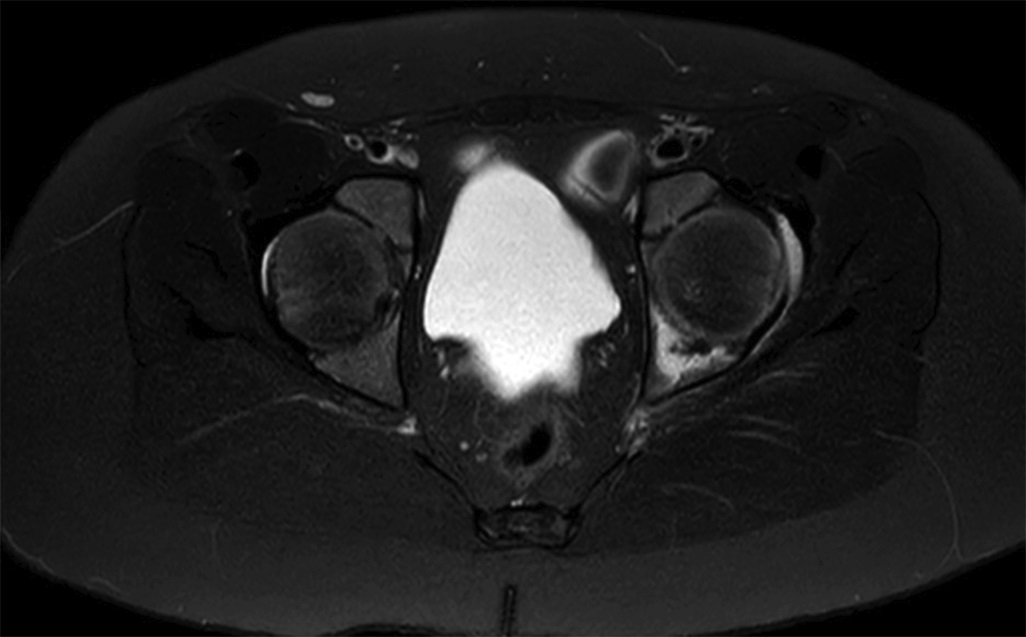
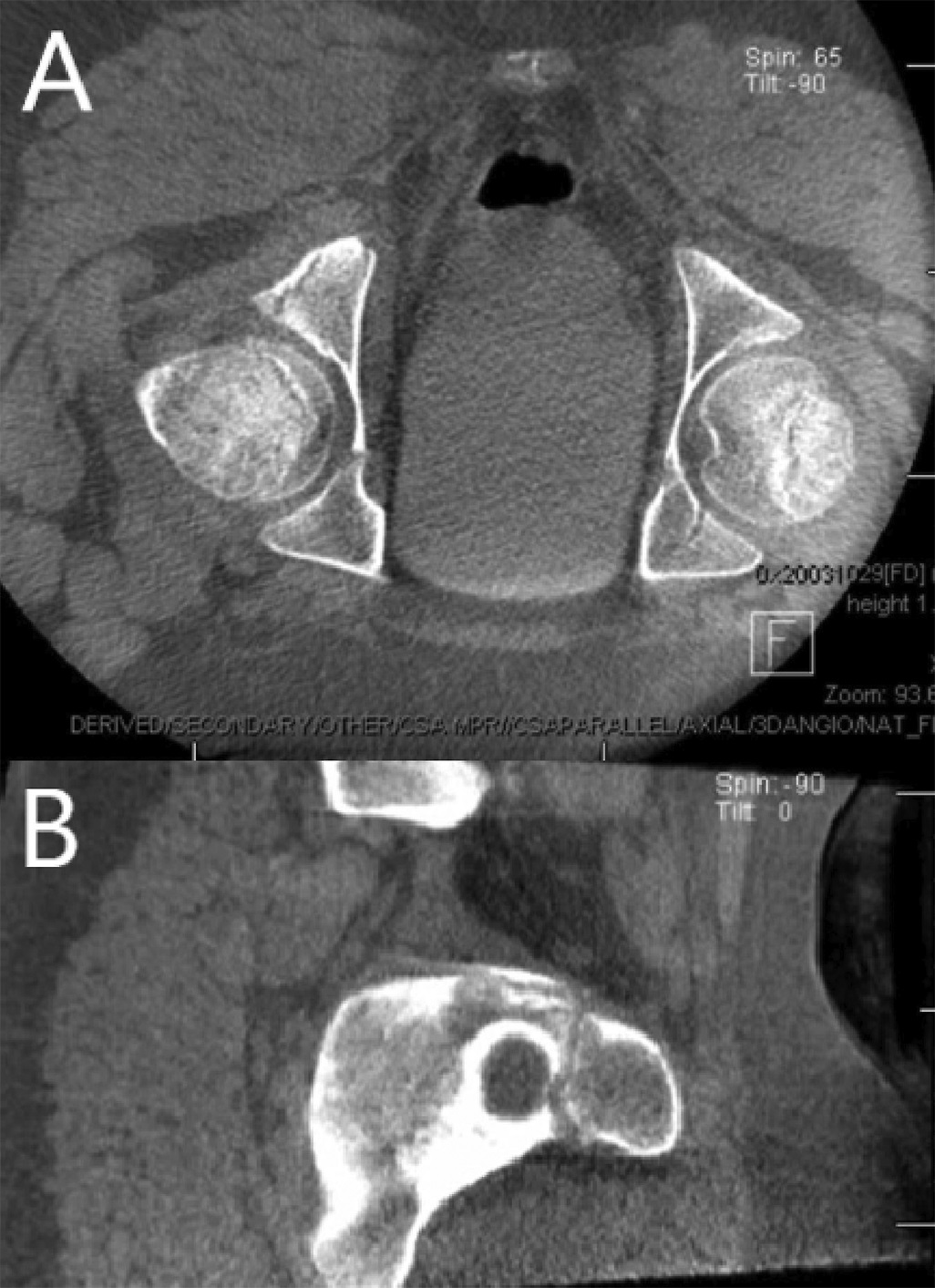
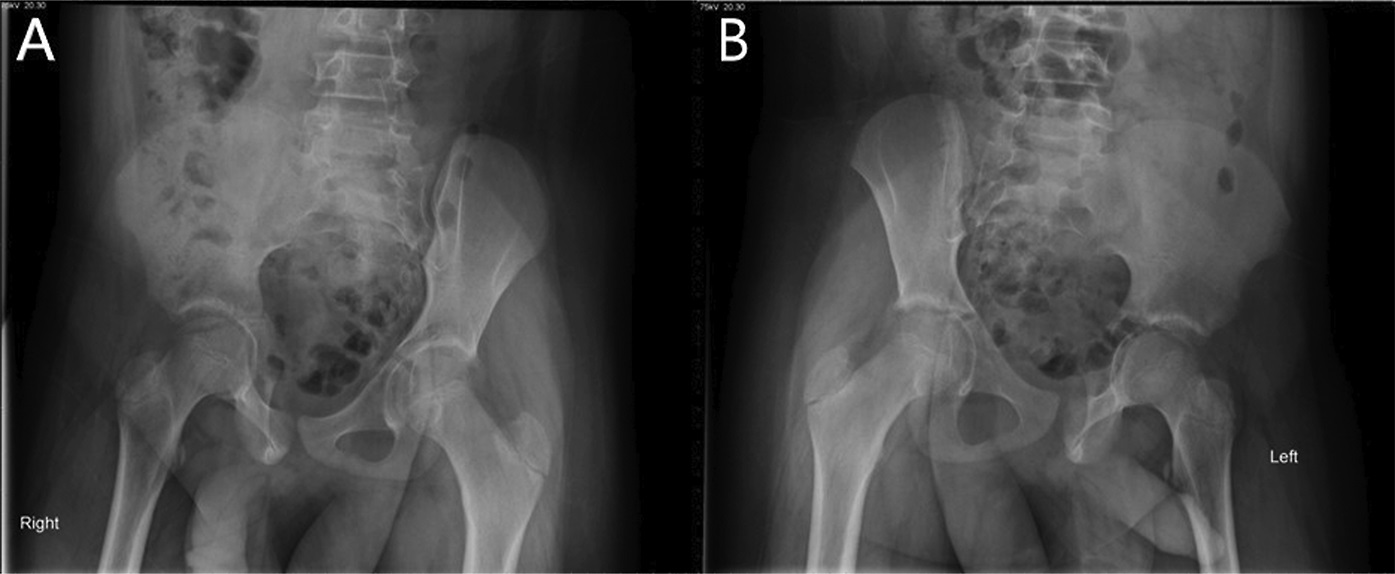
 Fig. 1
Fig. 1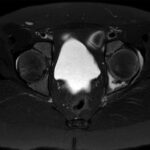 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5