A 23-year-old, right-hand–dominant man presented to the emergency department with worsening left shoulder pain after a fall. Six months earlier, he had been seen at another hospital after a snowboarding accident that incited severe pain in the left shoulder, which was believed to represent an acromioclavicular separation. Although he reported having no antecedent pain before that accident, the shoulder pain and restricted range of motion had never improved to baseline after physical therapy. The day before his presentation at our institution, the patient experienced a major exacerbation of the chronic shoulder pain after a fall onto the posterior left shoulder. The injury caused progressively worsening range of motion and acute pain that radiated distally down the left upper extremity without erythema or induration at the glenohumeral joint. Radiographs illustrated a lesion involving the left humeral head (Figs. 1-A and 1-B).
The patient was employed as an industrial manual overhead laborer. He had a medical history significant only for a right-sided, congenital solitary kidney. He reported that he did not use tobacco. The patient’s oncologic and family medical history was otherwise noncontributory.
A computed tomographic (CT) scan confirmed a soft-tissue mass with destruction of the proximal left humeral metaphysis and lateral humeral head with extension into the glenohumeral joint space, suspicious for osteosarcoma (Fig. 2-A). A magnetic resonance imaging (MRI) scan with gadolinium contrast revealed a 5.0 × 4.9 × 5.5 cm lesion of the left humeral head with intra-articular involvement, circumferential biceps tendon sheath extension, and soft-tissue extension deep to the deltoid muscle (Fig. 2-B).
The patient underwent an open biopsy of the left proximal humerus (Fig. 3).
The combination of imaging studies and biopsy was interpreted as a conventional giant cell tumor of bone.
The patient underwent en bloc resection with wide margins of the left proximal humerus with extra-articular shoulder excision, including the glenoid and shoulder capsule. Reconstruction was completed with an allograft-prosthetic composite shoulder hemiarthroplasty with capsular reconstruction (Fig. 4). The soft-tissue mass abutted the axillary and musculocutaneous nerves, which were preserved. The patient tolerated the procedure well with no perioperative complications. The postoperative course was uneventful.
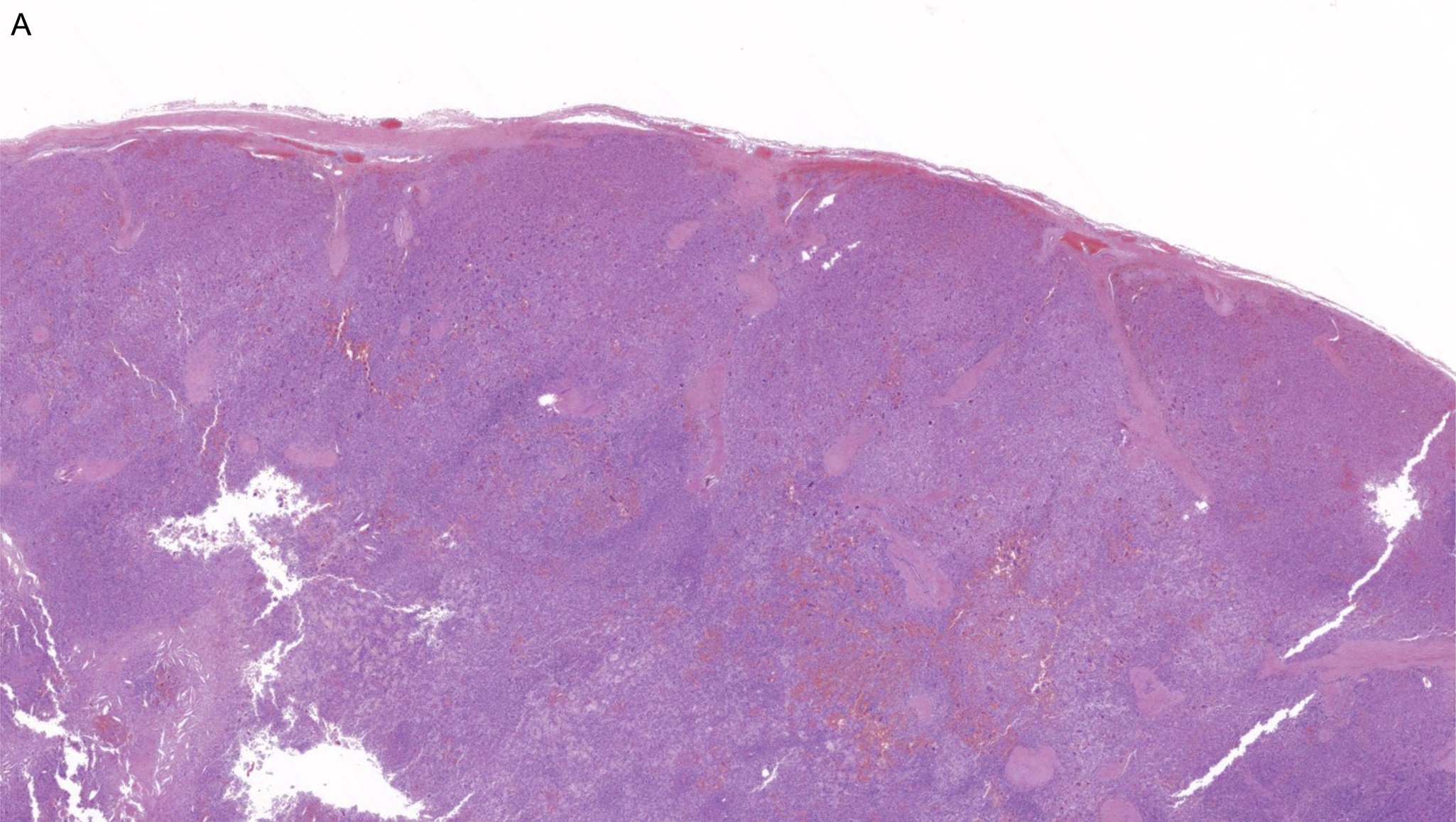
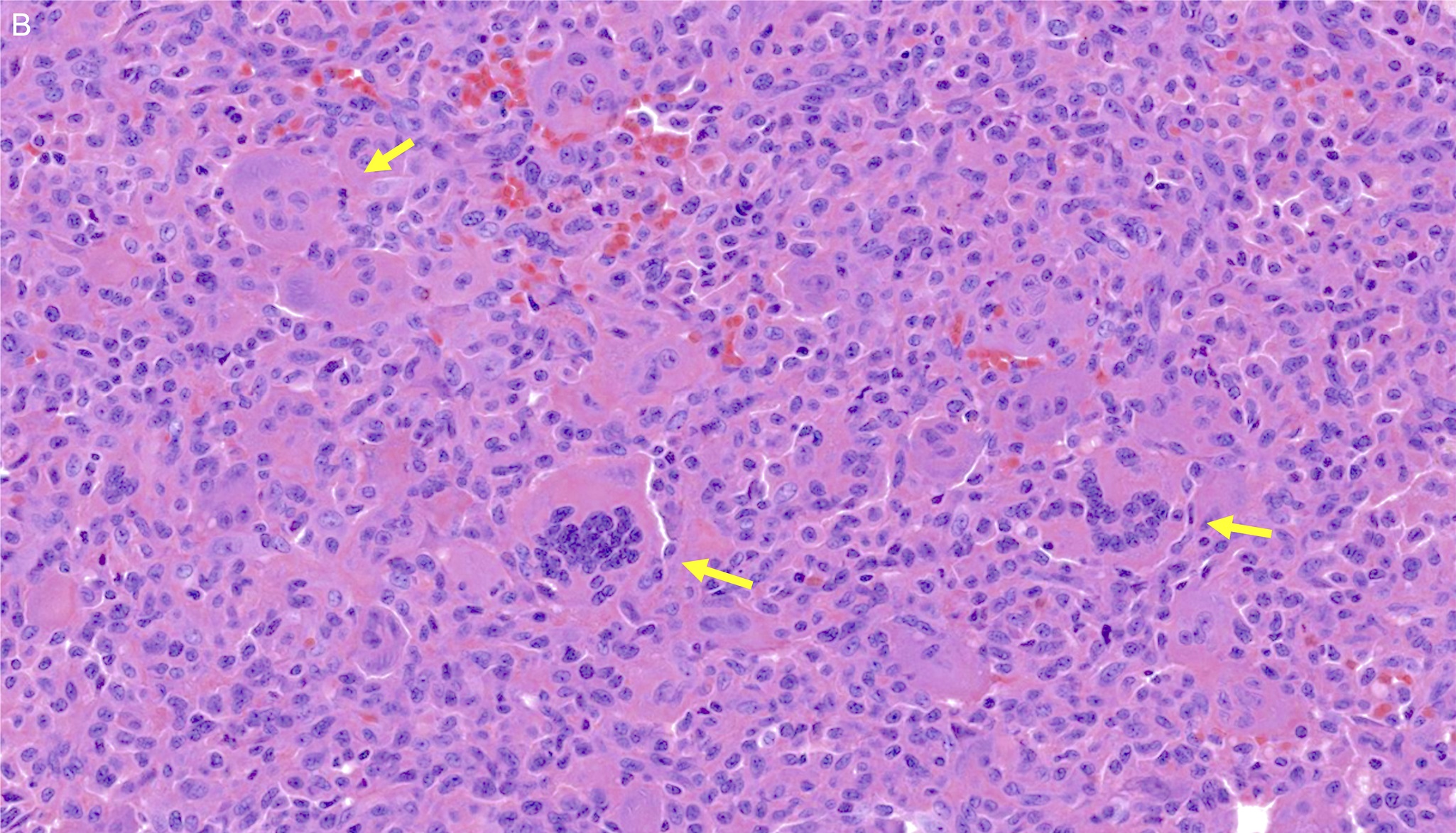
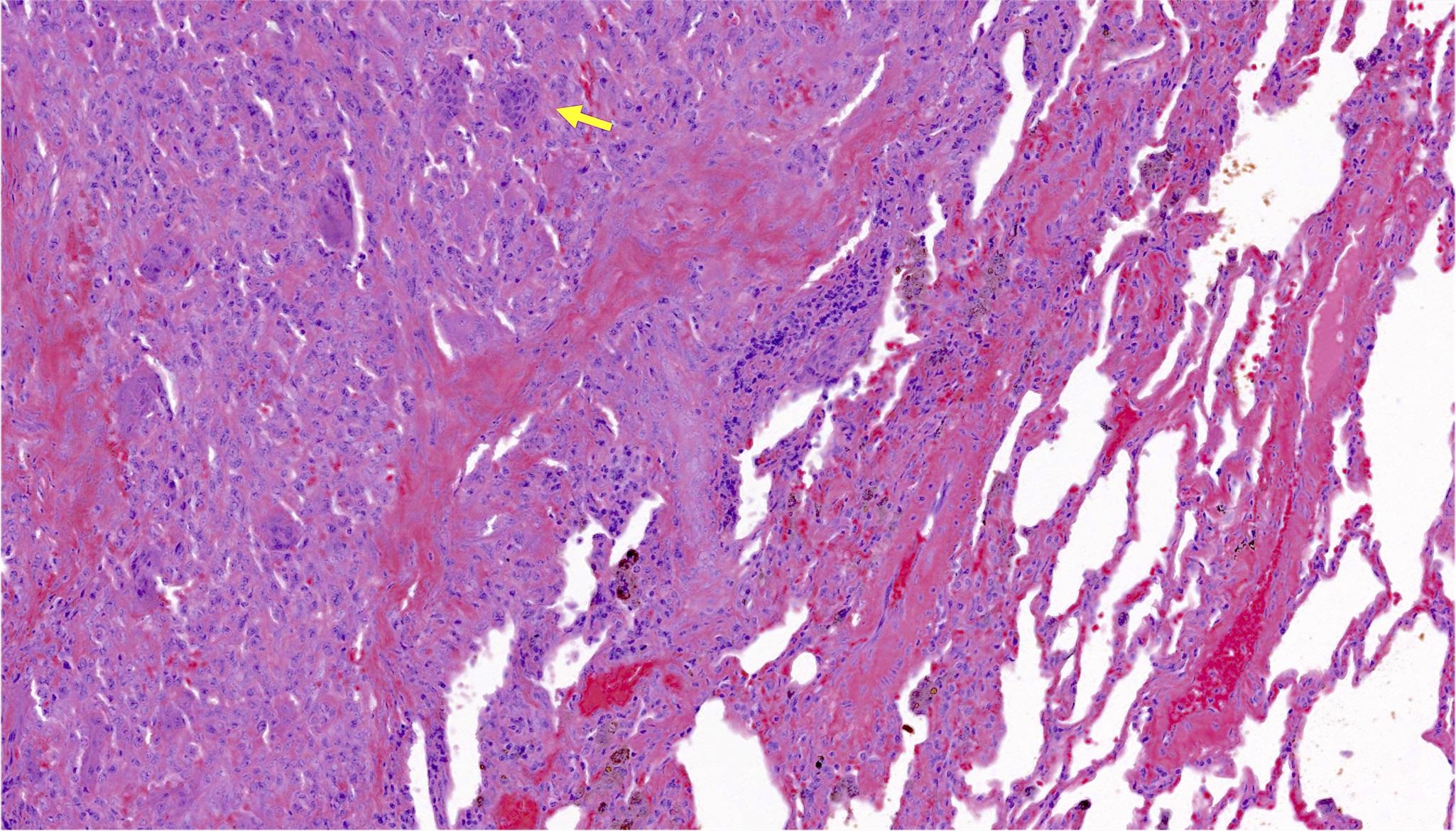
A histologic review of the surgical resection specimen again revealed a highly cellular tumor composed of neoplastic mononuclear cells extending beyond the confines of the bone into the surrounding soft tissues (Fig. 5-A). Careful, close inspection again demonstrated classic histologic features of giant cell tumor of bone without involving areas of high-grade sarcomatous dedifferentiation (Fig. 5-B).
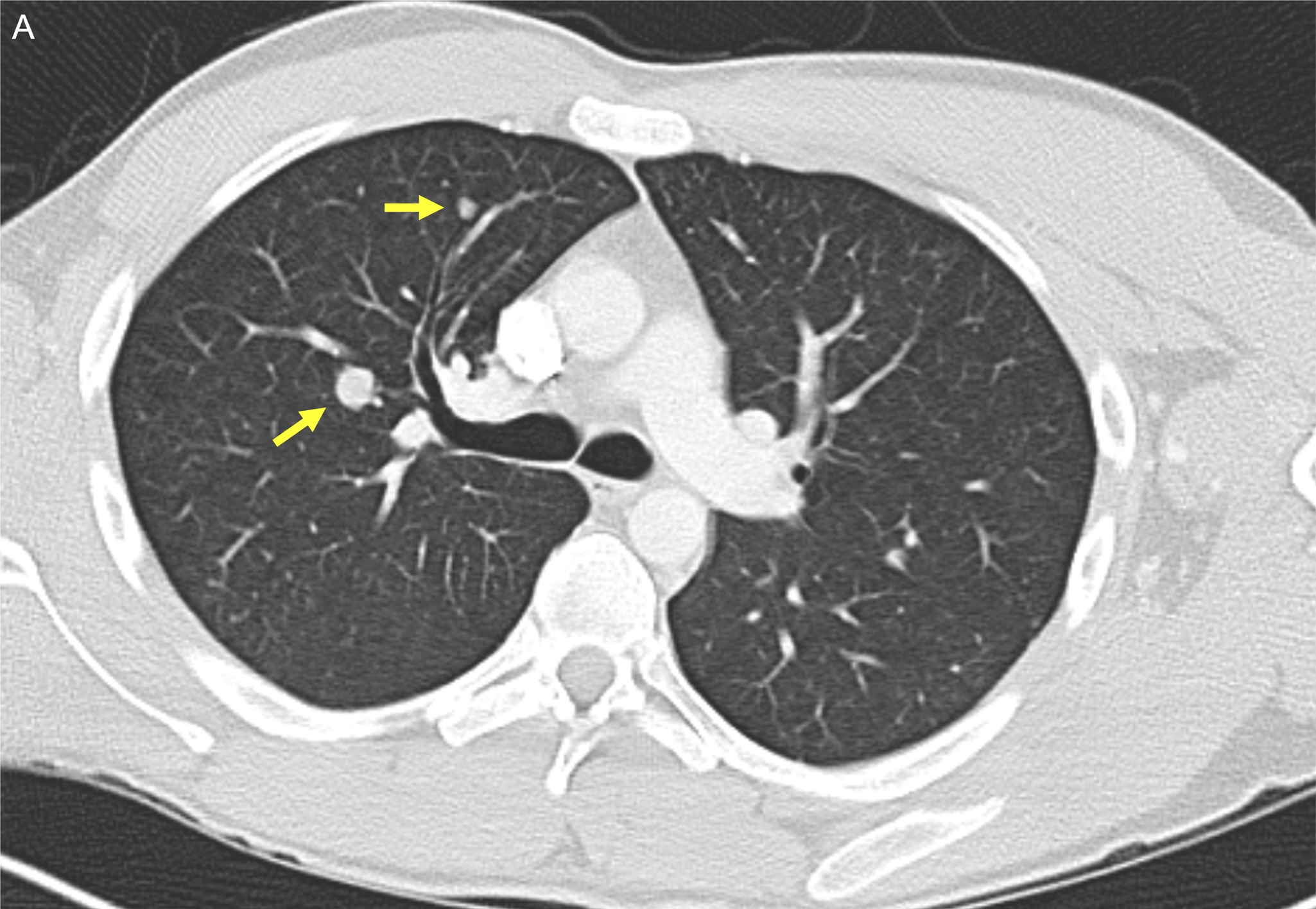
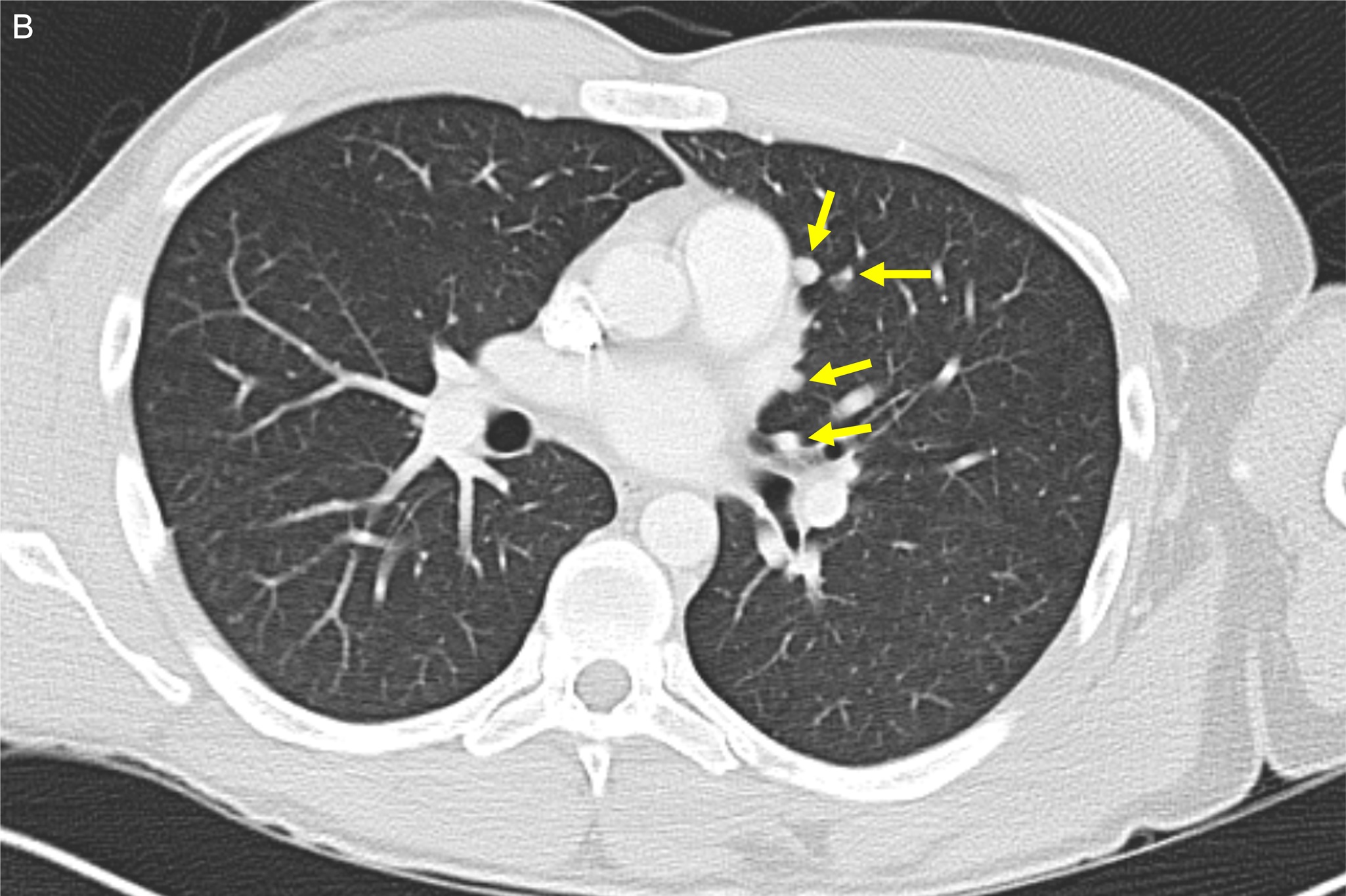
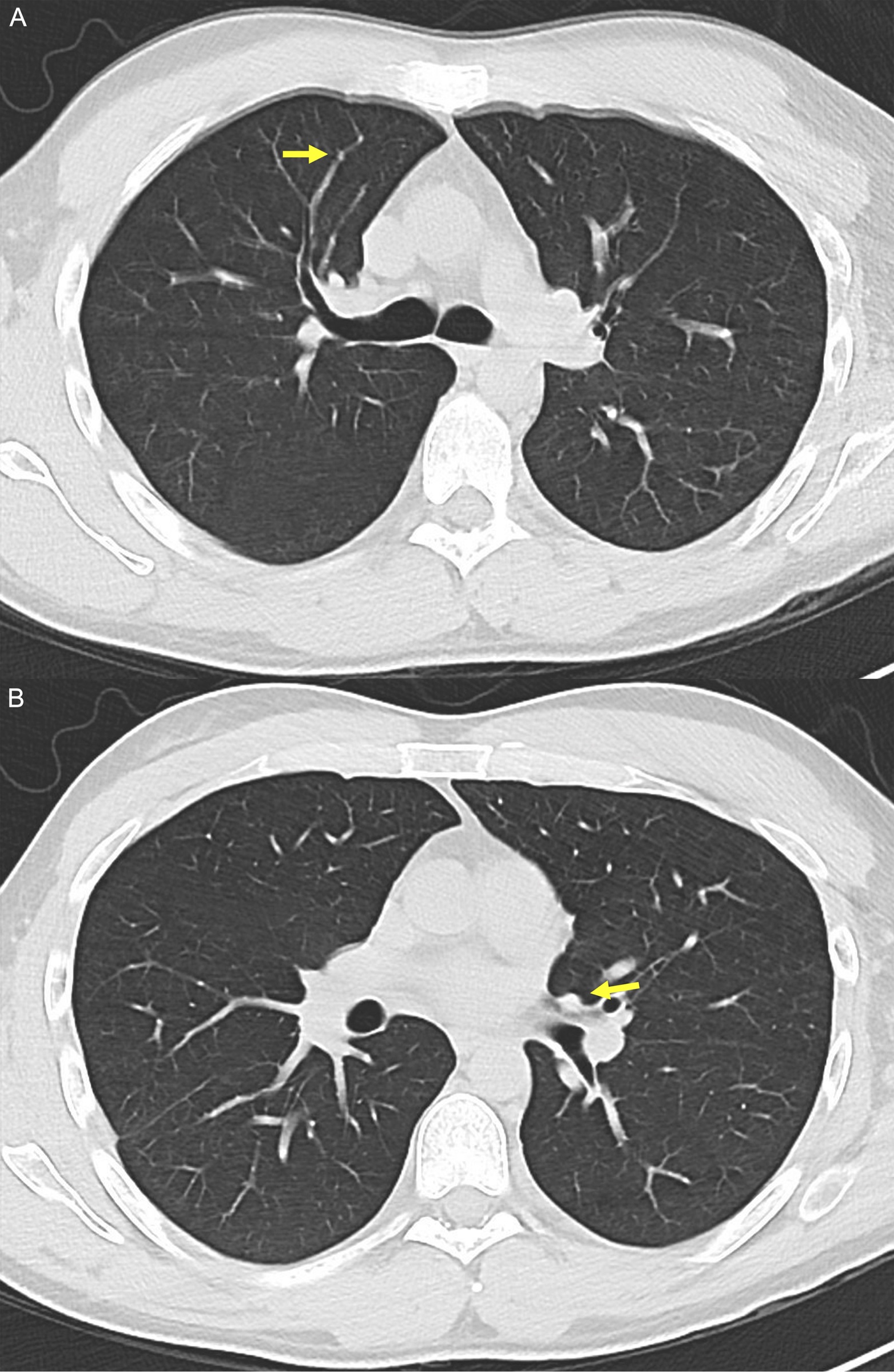
A contrast-enhanced chest CT scan made during the initial evaluation demonstrated diffuse (>20) bilateral pulmonary nodules, worrisome for metastatic disease (Figs. 6-A and 6-B). These nodules ranged in size from 5 to 11 mm in the longest dimension.
At 6 weeks after reconstruction of the shoulder, the patient underwent a video-assisted thoracoscopic surgical procedure for a definitive diagnosis of the pulmonary nodules by the left lower-lobe wedge resection. A histologic review of this wedge resection confirmed the presence of metastatic conventional giant cell tumor of bone without evidence of sarcomatous dedifferentiation (Fig. 7).
At the time of this writing, the patient had been followed regularly for >6 years. In collaboration with pediatric oncology and the multidisciplinary sarcoma tumor board, close monitoring with serial imaging, without systemic therapy was recommended for the benign pulmonary metastases. The patient underwent thoracic CT scans every 3 months in the first year and then underwent annual scans thereafter. On the most recent surveillance imaging, the nodules demonstrated modest spontaneous regression over time, measuring 2 to 3 mm in the longest dimension (Fig. 8). At the most recent follow-up, the patient had no evidence of local recurrence, further progression of the pulmonary nodules, or impairment to pulmonary function, and he had remained active by walking 10 to 15 miles per week, running 1 mile per week, and climbing over 3 flights of stairs without shortness of breath. He had returned to work as an overhead laborer and had competed in CrossFit training after his initial recovery.
Proceed to Discussion >>Reference: Leland CR, Pratilas CA, Gross JM, Levin AS. Diffuse pulmonary metastases at presentation of giant cell tumor of bone: a case report and synthesis of literature. JBJS Case Connector. 2023 January-March;13(1):e22.00496.
Giant cell tumor of bone is an osteolytic neoplasm that may have a locally aggressive radiologic appearance with worsening ostealgia or pathologic fracture at presentation. Between 3% and 7% of patients develop metastatic lung disease with features of conventional giant cell tumor of bone. Such events are difficult to predict on the basis of histology, and they most commonly present late in a disease course after local recurrence. Most often, giant cell tumor of bone is treated locally with curettage or resection and reconstruction, if appropriate. Previous studies have documented a frequency of local recurrence of >50% when giant cell tumor of bone is treated exclusively with curettage, and this rate was lower after wide excision. We elected to operatively manage the primary giant cell tumor of bone in this patient by resection with wide margins due to the tumor’s aggressive appearance and sarcoma-like masquerade.
Previous case series have documented pulmonary metastases arising after primary tumor resection and at or after the time of local recurrence. The management of pulmonary metastases generally follows surgical resection, if possible, if patients are actively or potentially symptomatic from the disease due to tumor-related pulmonary morbidity. For unresectable or recurrent metastases, locoregional radiation therapy and denosumab are nonoperative options, although a long-term use of the latter may have undesirable side effects such as osteonecrosis of the jaw, atypical femoral fractures, and potential sarcomatous transformation. Because of the indolent nature of giant cell tumor of bone, pulmonary metastases may also be managed with regular surveillance, which was chosen for our patient.
After an extensive review of the literature, we identified 9 studies showing at least 1 patient with pulmonary metastases at presentation. These studies identified 2,115 primary giant cell tumors of bone and included 1,669 of those for review. There were 114 cases of pulmonary metastases, 14 of which were diagnosed at the initial presentation. Excluding 1 study that exclusively reported on patients with pulmonary metastases, the pooled incidence of pulmonary metastases at presentation was 0.7% (range, 0.6% to 1.7%), and the pooled incidence of all pulmonary metastases was 5.5% (range, 2.3% to 8.5%). In studies describing the management of patients with pulmonary metastases diagnosed at presentation, wedge resection or metastasectomy was performed in 6 patients, with 3 patients each undergoing systemic therapy and radiotherapy. One patient died due to unrelated causes, and 1 patient experienced a progression of nodules requiring subsequent resection. Four patients underwent observation, with 1 patient lost to follow-up and the remaining 3 patients alive with stable disease.
Our case is atypical in that this locally aggressive tumor presented with diffuse pulmonary metastases at the initial presentation, with spontaneous regression of the masses without systemic or locoregional therapy. The overall findings of an aggressive tumor with diffuse pulmonary metastases raised strong suspicion at presentation that this represented dedifferentiated giant cell tumor of bone, although histologic evaluation and subsequent long-term follow-up confirmed its indolent behavior. Furthermore, although prior case series have advocated metastasectomy in such patients, our patient demonstrated spontaneous regression, even in advanced presentations. This case further supports routine thoracic CT scans for appropriate staging at presentation of all primary giant cell tumors of bone because synchronous pulmonary metastases may already be present.
Although pulmonary metastatic disease in giant cell tumor of bone is rare, it is well-recognized in the literature, and it most commonly occurs in the setting of local recurrence. Far less common is a finding of either lung metastases at the initial presentation or spontaneous regression of pulmonary metastatic disease without systemic therapy. Although exceedingly rare, occasional patients have synchronous pulmonary metastases at the time of identification of a giant cell tumor of bone. We added a case to the literature demonstrating that, although extensive synchronous metastases may be present at the time of identification of an aggressive primary lesion, they may follow an indolent clinical course with spontaneous regression over time.
Reference: Leland CR, Pratilas CA, Gross JM, Levin AS. Diffuse pulmonary metastases at presentation of giant cell tumor of bone: a case report and synthesis of literature. JBJS Case Connector. 2023 January-March;13(1):e22.00496.
What is the diagnosis?
Conventional giant cell tumor of bone
Dedifferentiated giant cell tumor
Giant cell-rich osteosarcoma
Granulomatous inflammation suggestive of mycobacterial infection
Solid aneurysmal bone cyst



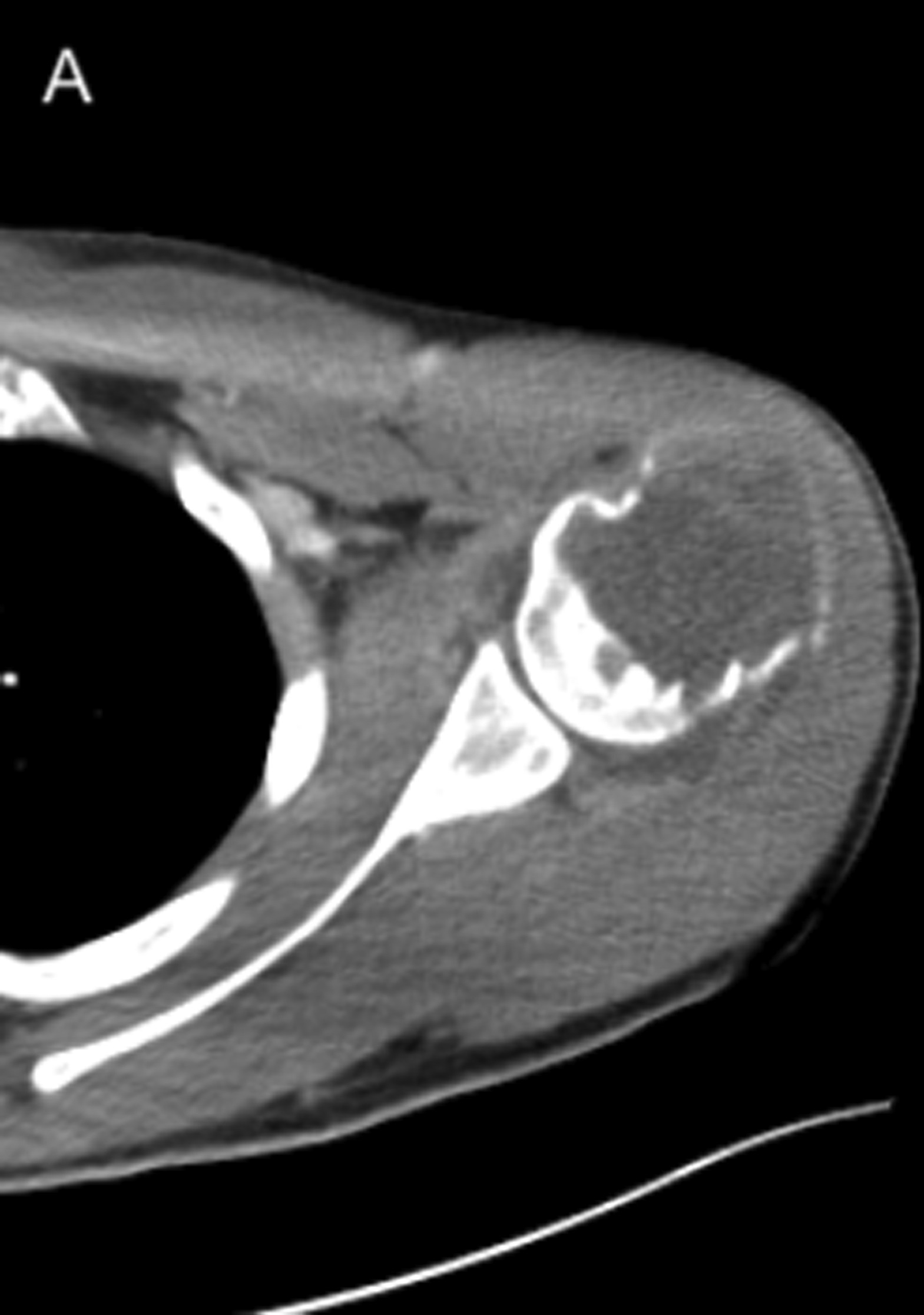
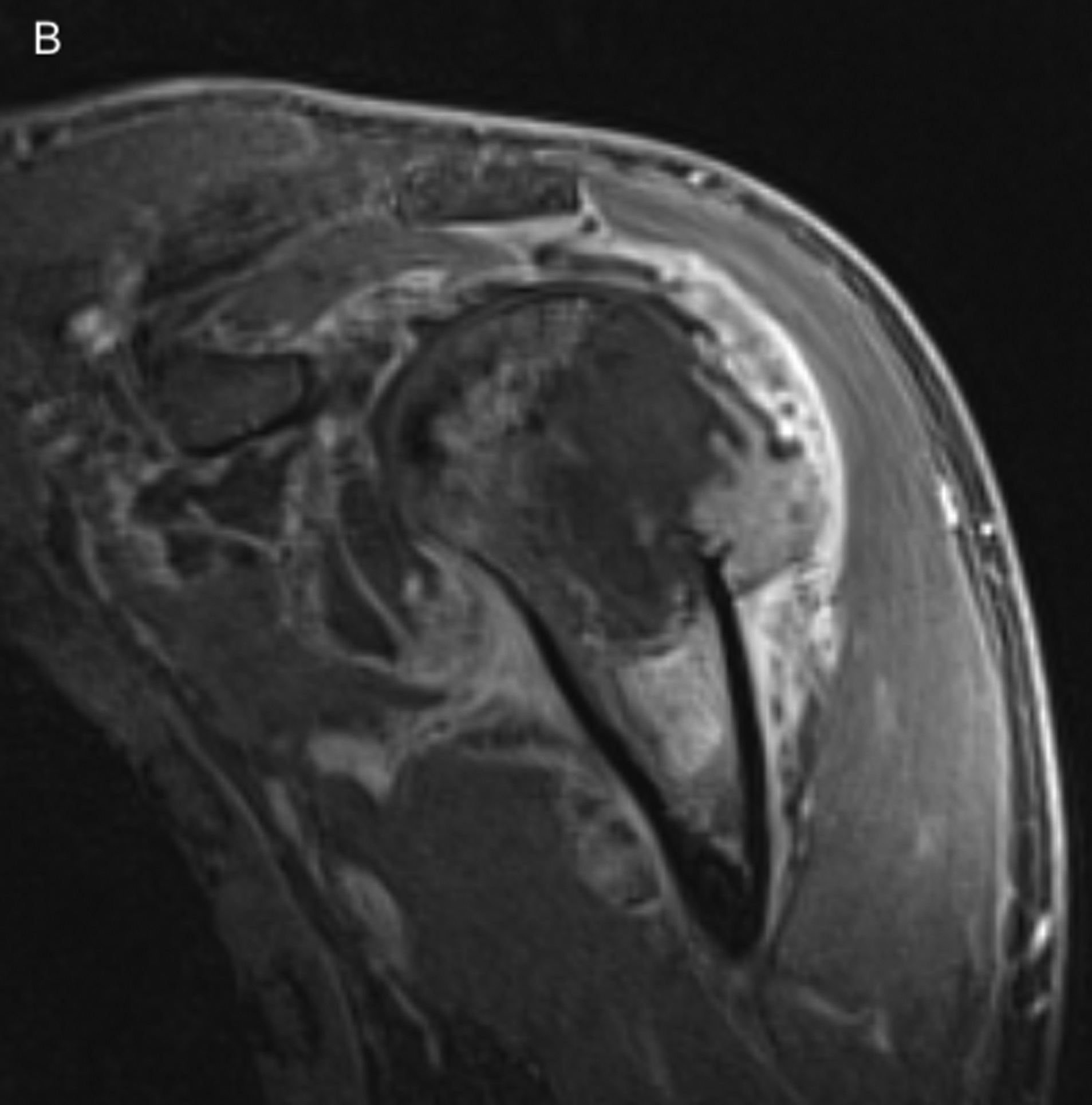
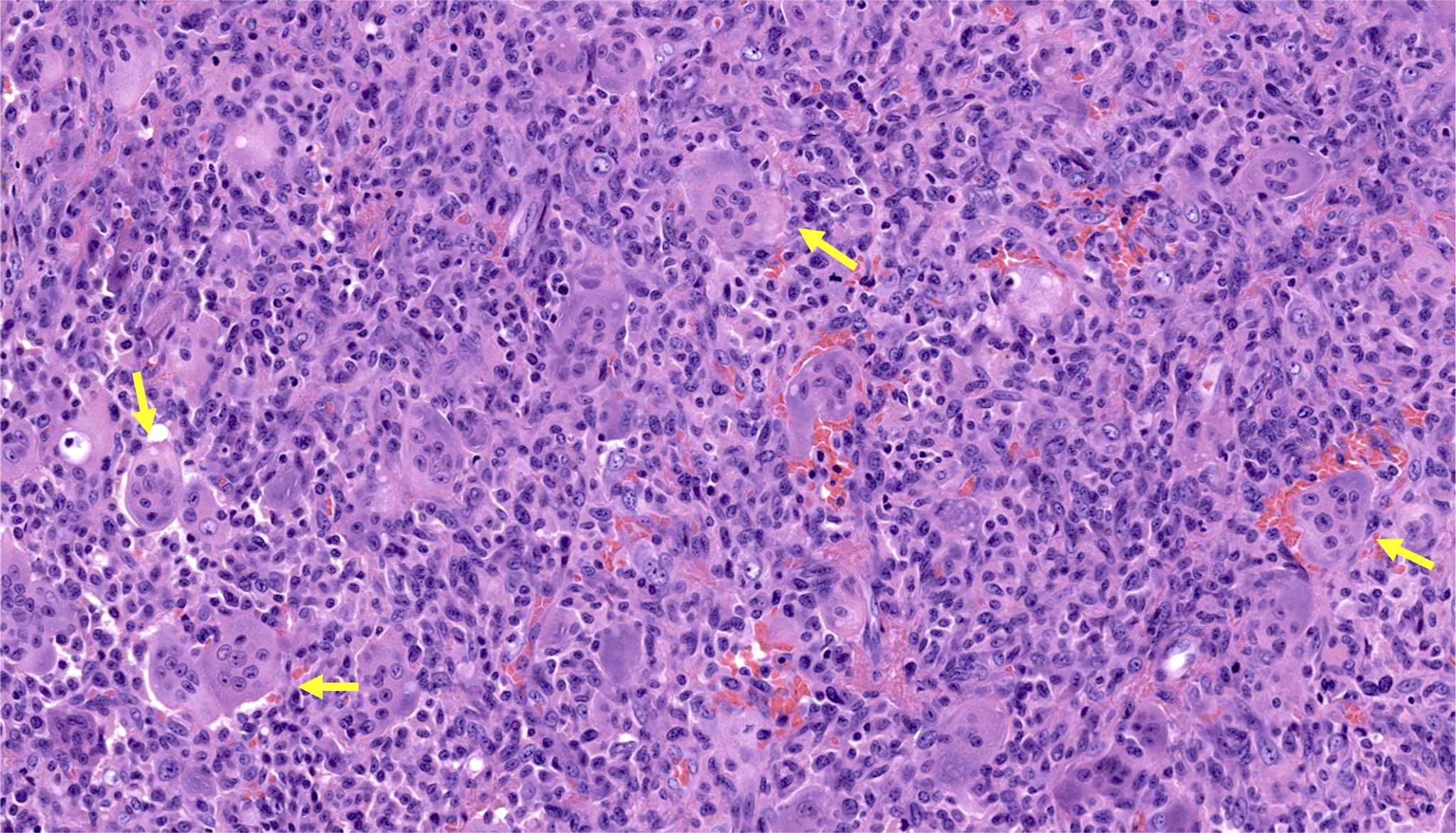
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5-A
Fig. 5-A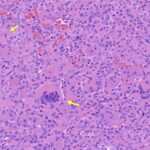 FIg. 5-B
FIg. 5-B Fig. 6-A
Fig. 6-A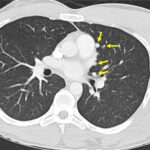 Fig. 6-B
Fig. 6-B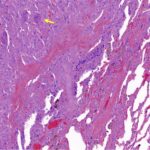 Fig. 7
Fig. 7 Fig. 8
Fig. 8