An 18-year-old man with no major medical history presented to our sports medicine clinic with right hip pain. He had started experiencing pain 1.5 months before presentation, after he kicked a punching bag. The pain improved within a day but returned 5 days later, when it woke him from sleep and kept him out of sports. He continued to have pain overnight and into the morning that made it difficult to descend stairs. He scheduled a clinic appointment 2 weeks after pain onset but canceled the appointment and returned to baseball practice when the pain resolved spontaneously. One month after the initial event, the hip pain recurred after he swung a baseball bat. He presented to our clinic 3 days later after the pain began to wake him from sleep and started to radiate down the thigh toward the anterior aspect of the knee.
On presentation, the patient reported no associated fevers, night sweats, decreased appetite, current joint symptoms, rashes, or weight loss. He described experiencing back pain 4 months earlier that had resolved spontaneously. Medical history and family history were otherwise noncontributory. He had never undergone a surgical procedure and was not taking any medications. On physical examination, the patient had no soft-tissue swelling; no lymphadenopathy; no tenderness to palpation over the greater trochanter; limited active range of right hip flexion secondary to pain; no pain with resisted hip adduction; 3 of 5 muscle strength on hip flexion, limited by pain; and a negative log-roll test.
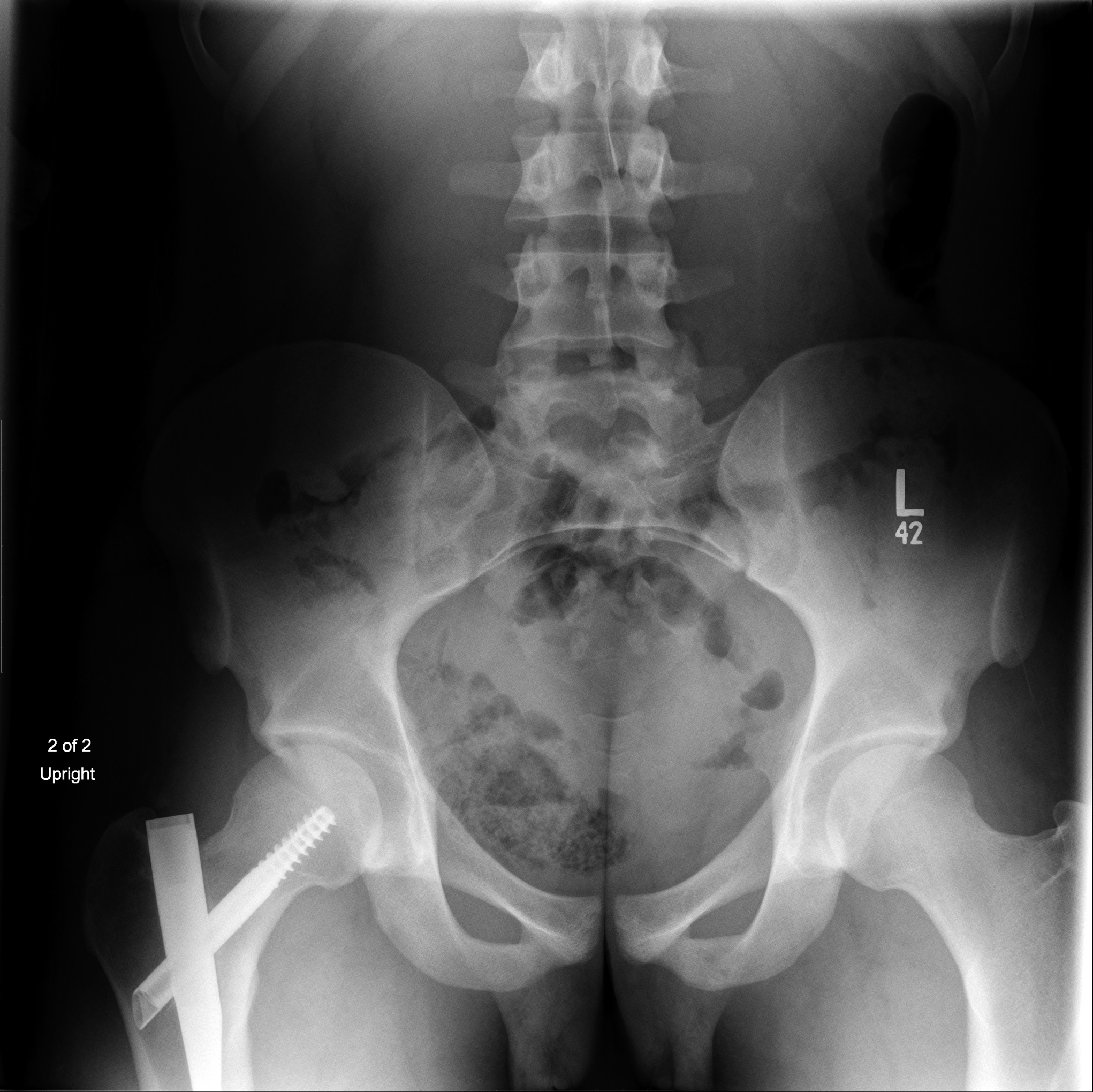
Anterior-posterior (Fig. 1) and lateral (Fig. 2) radiographs of the pelvis and right hip revealed a lytic lesion of the lesser trochanter of the right femur with cortical destruction and a lytic lesion of the left inferior pubic ramus with a possible pathologic fracture. Magnetic resonance imaging (MRI) scans of the pelvis, with and without contrast, showed 4 lesions. The largest (5 × 3.2 × 3.7 cm) was located in the lesser trochanter of the right femur (Figs. 3-A and 3-B). One lesion in the right femoral neck and one lesion in the posterior right sacral ala had been poorly visible on radiographs but were visible on MRI scans. A fourth lesion, in the left inferior pubic ramus, had radiographic findings otherwise consistent with an ischiopubic synostosis.
Bone scintigraphy was performed and showed increased radiotracer activity in the right femoral intertrochanteric region and the left ischium as well as mild, diffuse increased radiotracer uptake in the right femoral head and the acetabular pubic ramus. A computed tomographic (CT) scan of the chest without contrast showed lytic and sclerotic lesions of the T8 vertebral body, a smaller lesion of the L2 vertebral body, and multiple, small, indeterminate, pulmonary nodules.
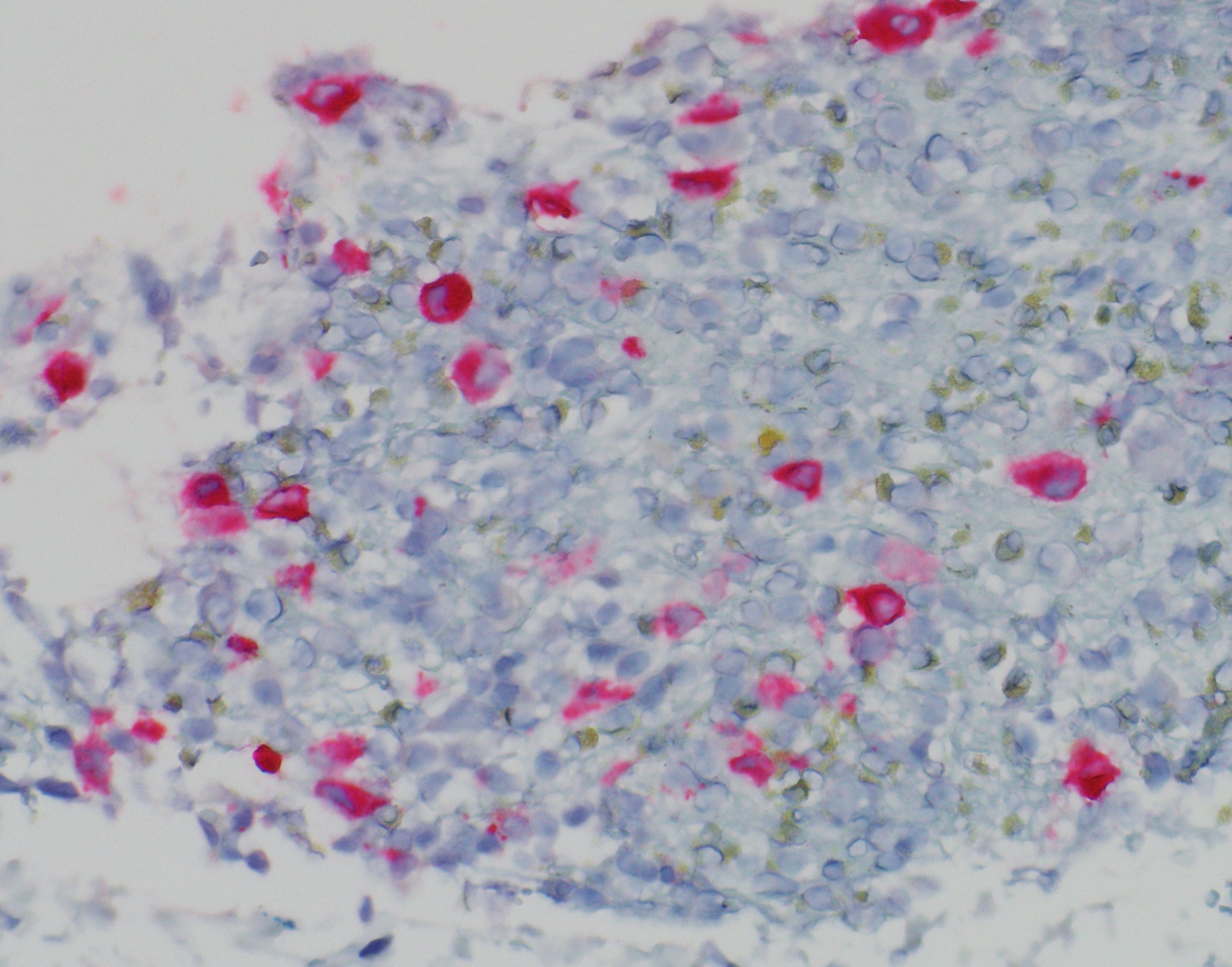
After initial imaging, a CT-guided biopsy of the right lesser trochanter was performed. Fine-needle aspiration cytopathology is shown in Figure 4.
Correct: Langerhans cell histiocytosis
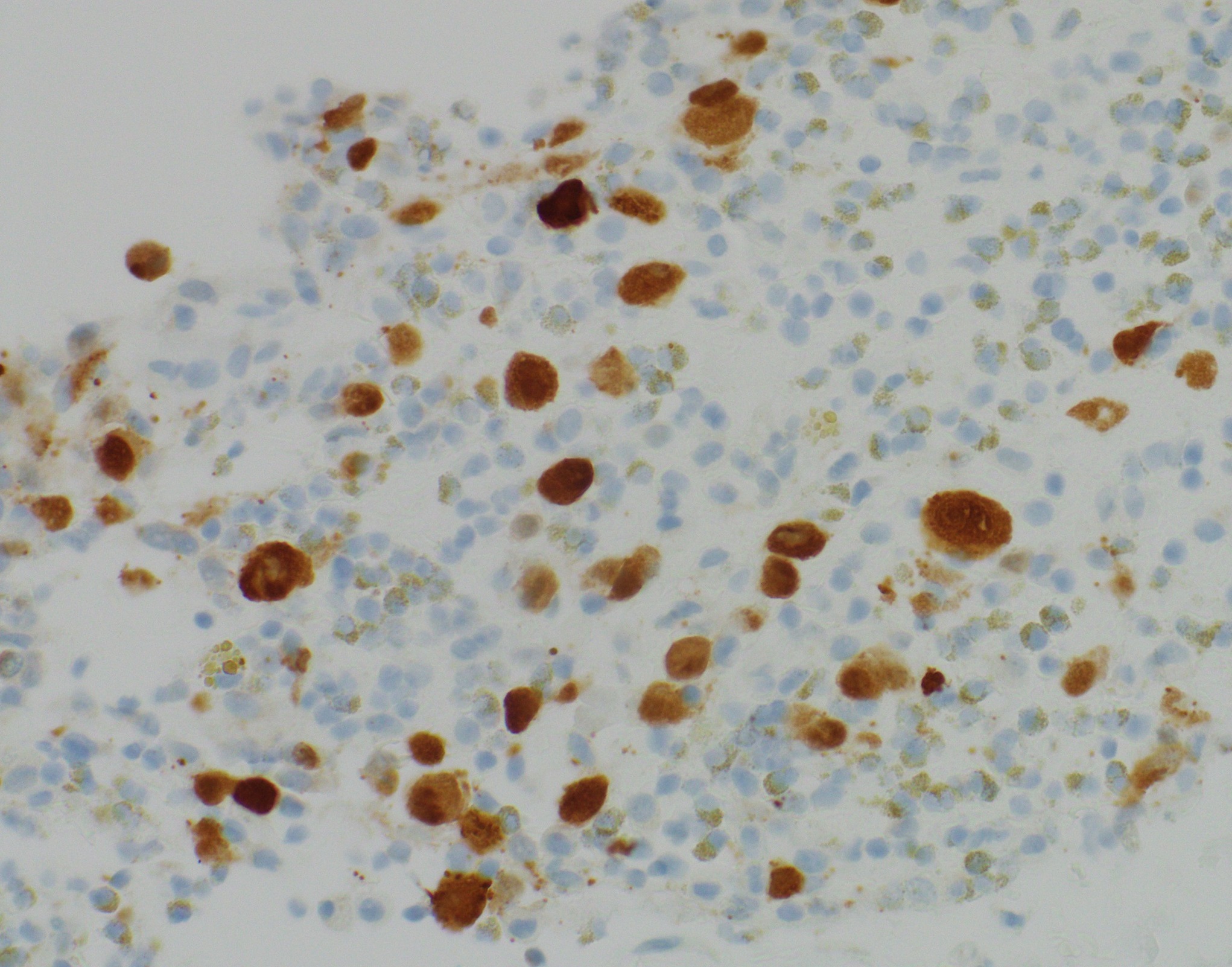
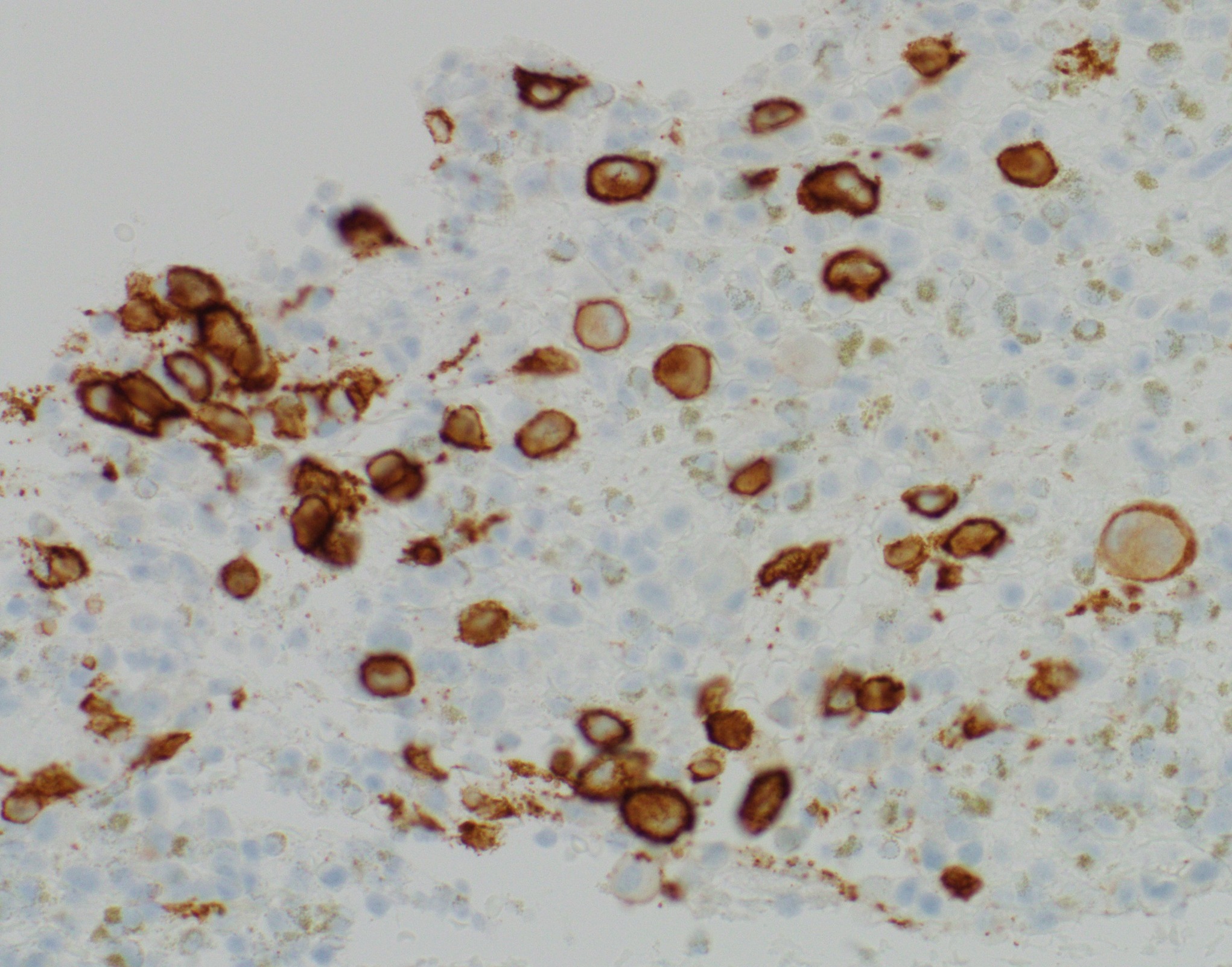
The immunohistochemical stains of the core needle biopsy specimen were positive for langerin (Fig. 5), S100 (Fig. 6), CD1a (Fig. 7), and CD68. Accompanied by the radiographic findings and the hematoxylin and eosin-stained biopsy, these findings indicate Langerhans cell histiocytosis.
The patient subsequently underwent prophylactic stabilization of the right proximal femur through the placement of an intramedullary nail, with curettage and cryoablation of the lesions of the femoral neck and lesser trochanter.
After discussion by a multidisciplinary tumor board, the patient underwent further imaging to evaluate for multisystem involvement. The 2-deoxy-2-[F-18]fluoro-D-glucose–positron emission tomography (FDG-PET)/CT scan showed focal, FDG-avid osseous lesions of the right femoral neck, right lesser trochanter, left inferior pubic ramus, and right posterior sacrum, as previously indicated on bone scan. In addition, the scan revealed photopenia in a mixed lytic-sclerotic lesion in the T8 vertebral body and no FDG uptake in a small radiolucent area in the anterior L2 vertebral body. No visceral FDG-avid lesions were identified. The patient underwent brain imaging, which showed no evidence of intracranial pathology. An oncologist treated the patient with a 6-week regimen of prednisone and weekly vinblastine according to the LCH-IV Stratum I, Group 2 protocol. On completion, radiographs and bone scintigraphy demonstrated an incomplete resolution of lesions. The treatment was repeated, and, on completion, the FDG-PET scan showed substantially decreased metabolic activity in the lesions. The patient progressed to taking monthly vinblastine and prednisone and undergoing bimonthly radiographs. After 3 months, a pelvic radiograph (Fig. 8) revealed an improvement of the lesions, and chemotherapy treatment was stopped. It was planned for the patient to undergo follow-up by an oncologist every 6 to 12 months for 5 years.
Proceed to Discussion >>Reference: McCambridge TM, Papakyrikos C, Levin A. Langerhans cell histiocytosis presenting as a lesser trochanter fracture in an adolescent: a case report. JBJS Case Connector. 2023 January-March;13(1):e21.00820.
Langerhans cell histiocytosis is an uncommon disease for which the epidemiology in children younger than 15 years of age has been well described. In a recent analysis by Salotti et al., 94 cases of Langerhans cell histiocytosis were identified in the United Kingdom during a 2-year period, representing an annual incidence of 4.1 cases per 1 million children <15 years of age. Although Langerhans cell histiocytosis occasionally presents in patients >15 years of age, its incidence in this group is far lower. We are aware of only 2 studies of the epidemiologic characteristics of Langerhans cell histiocytosis in adolescents and adults published in the past 25 years. The most recent study by Goyal et al. revealed an incidence of Langerhans cell histiocytosis in adults of 0.07 cases per 1 million per year.
In the present case, an 18-year-old man was diagnosed with multifocal, single-system Langerhans cell histiocytosis of bone. Although this diagnosis is highly uncommon at this patient’s age, his clinical presentation was otherwise not atypical of the diagnosis. A review of the initial symptoms showed that the patient had midthoracic discomfort, which largely resolved before presentation. Bone scan and PET/CT scan showed evidence of a lesion at that site that was no longer FDG-avid. Despite the highly variable presentation of Langerhans cell histiocytosis, one characteristic finding in the pediatric population is vertebra plana. This was not identified on chest CT imaging; however, lytic foci at risk of compression fracture were evident.
Another surprising finding was the patient’s lack of discomfort when sitting on firm surfaces, which would have been consistent with the lesion of the left inferior pubic ramus and ischium. Similarly, the site was otherwise not tender to palpation during examination, with no pain on resisted knee flexion, hip extension, and hip adduction on the left side. Imaging findings for this lesion resemble an ischiopubic synostosis, which would typically be closed by the patient age of 18 years, illustrating why Langerhans cell histiocytosis has been dubbed a “great mimicker.”
Langerhans cell histiocytosis has a wide spectrum of clinical presentations, ranging from solitary bone lesions to disseminated disease involving multiple organ systems. In the present case, the patient had multifocal bone disease. Bone is the most affected system, comprising 80% of patients diagnosed with Langerhans cell histiocytosis. Solitary, bone-only lesions can often be managed with intralesional curettage, with or without local adjuvant therapy, and close surveillance. For patients with multifocal bone-only disease, or multisystem involvement, systemic therapy is often indicated. Because our patient was experiencing pain and had a high risk of pathologic fracture, he underwent intralesional treatment with a local adjuvant, as well as prophylactic stabilization.
Although the skeleton is the most common organ involved in Langerhans cell histiocytosis, nearly 80% of children with this disease have cutaneous manifestations. In a limited series of adults with Langerhans cell histiocytosis, skin involvement was less prevalent, and the most common presenting symptom was localized pain caused by bone involvement, which occurred in 34% of patients. When analyzing the organ system involvement in pediatric patients >5 years of age, bone-only disease, either solitary or multifocal, is the most common presentation.
Given our patient’s age and clinical presentation, the symptoms that he experienced correspond well with the rare reports of presentations of Langerhans cell histiocytosis in adolescents. Although patients with oncologic illnesses do occasionally present to pediatric sports medicine practices, they are often evaluated initially by pediatricians. This patient’s previous visits to the sports medicine clinic and his established trust with the physician likely contributed to his decision to present there, rather than to a pediatric clinic. This case highlights the importance of sports medicine physicians maintaining a level of clinical suspicion and considering a broad differential diagnosis when evaluating hip pain in the adolescent athlete.
Reference: McCambridge TM, Papakyrikos C, Levin A. Langerhans cell histiocytosis presenting as a lesser trochanter fracture in an adolescent: a case report. JBJS Case Connector. 2023 January-March;13(1):e21.00820.
What is the diagnosis?
Lymphocytes and eosinophils suggestive of Hodgkin lymphoma
Small cell malignant neoplasm consistent with Ewing sarcoma
Large cell, non-Hodgkin lymphoma
Langerhans cell histiocytosis
Granulomatous inflammation suggestive of mycobacterial infection



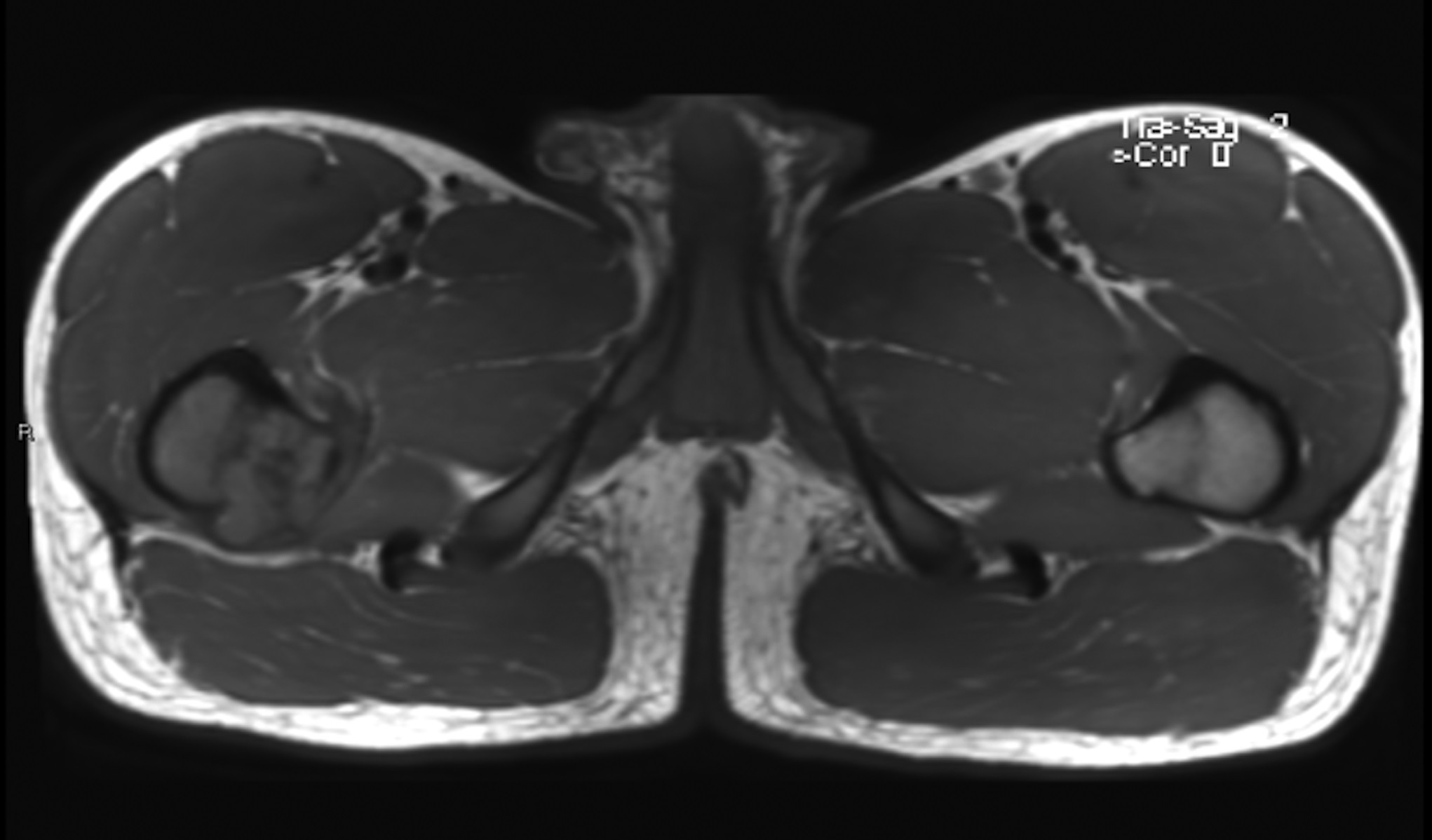
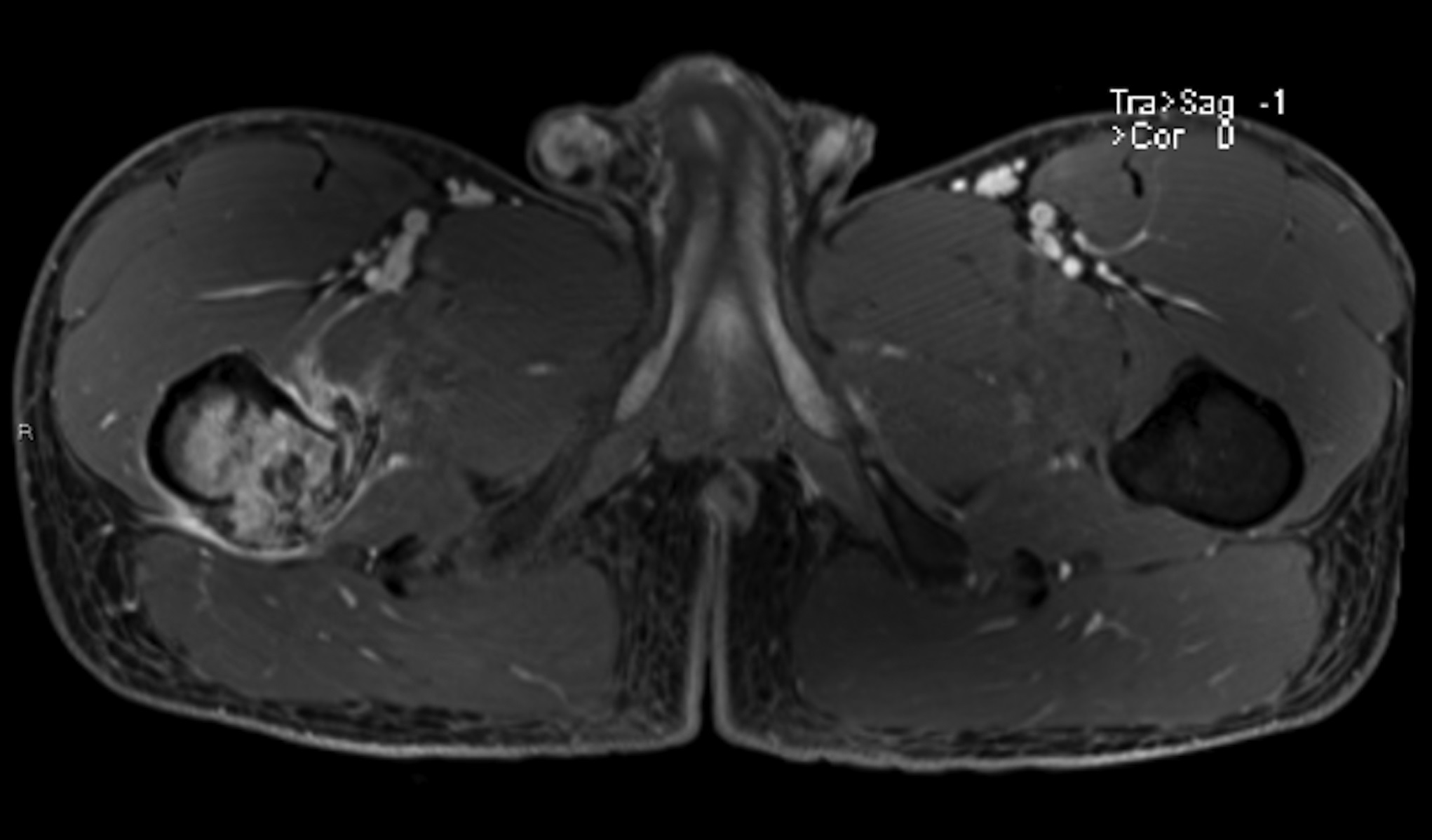
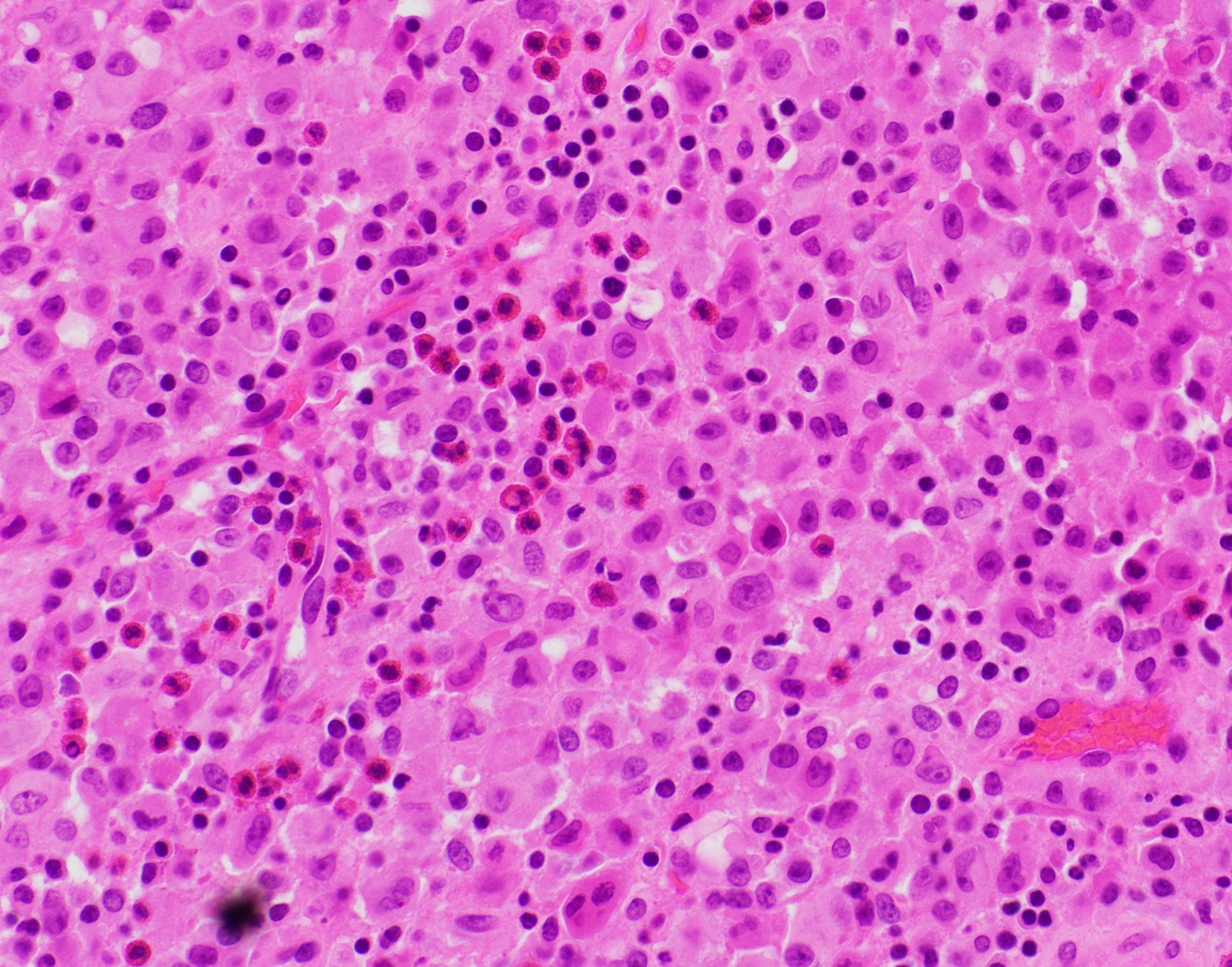
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A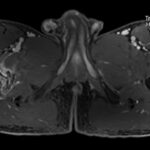 Fig. 3-B
Fig. 3-B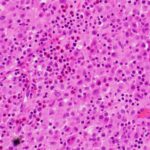 Fig. 4
Fig. 4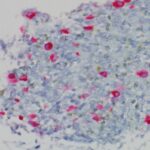 Fig. 5
Fig. 5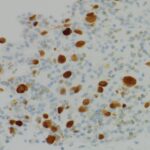 Fig. 6
Fig. 6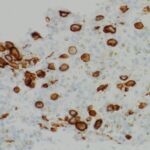 Fig. 7
Fig. 7 Fig. 8
Fig. 8