A 23-Year-Old Woman with Foot Pain Following a Fall
November 1, 2023
A 23-year-old woman, with a medical history of recurring unicameral bone cysts in the humerus, presented to the clinic with left foot pain. She had tripped on a sidewalk 6 months previously and had been seen immediately after the initial injury at an outside institution. Radiographs made at that time showed an incidental oval lucent lesion within the cuboid bone with subtle cortical irregularity along the lateral and plantar aspects of the cuboid (Fig. 1). A follow-up magnetic resonance imaging (MRI) scan acquired 3 weeks after the initial radiographs and injury demonstrated a nondisplaced, probable pathologic fracture of the cuboid through a somewhat heterogenous circumscribed lesion (Fig. 2). Although this advanced imaging had some concerning findings, no additional evaluation was undertaken. The patient was initially managed with a controlled ankle motion walker boot, and she experienced pain relief. Six months later, the patient began feeling pain again in the left foot, and another MRI scan was acquired at an outside institution. These images showed progression of the cuboid lesion with mixed T2 signal characteristics and relatively homogeneous moderate T1 signal hypointensity (Fig. 3). At this point, the patient was referred to our department for evaluation.
On physical examination, there was no swelling, tenderness, deformity, or ecchymosis of the left foot. Radiographs of the left foot and left humerus were both made. The radiograph of the left humerus demonstrated a fully healed unicameral bone cyst. The radiographs of the left foot revealed progression of the lesion in the cuboid bone when compared with the earlier images (Fig. 4).
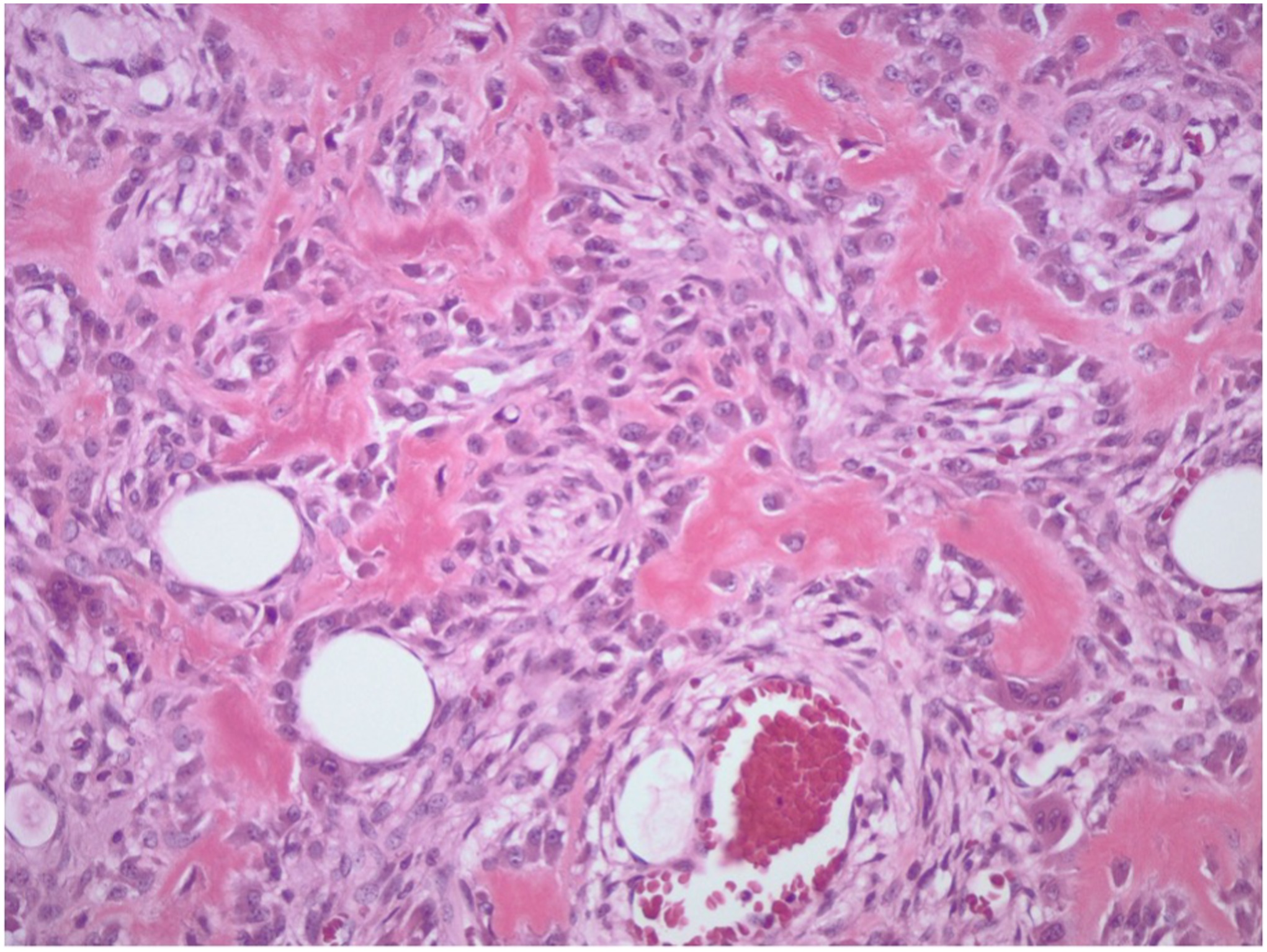
An open incisional biopsy with a frozen section was performed (Fig. 5).
The frozen section of the tumor was consistent with an aggressive tumor ranging anywhere from an osteoblastoma to an osteosarcoma. Permanent sections revealed a final diagnosis of osteosarcoma (Fig. 6). Staging with computed tomographic (CT) scans of the chest, abdomen, and pelvis as well as positron emission tomography and CT scans revealed stage-IIA (cT1, cN0, cM0, and G3) osteosarcoma with no evidence of metastatic disease.
After discussion with the patient, a treatment plan of neoadjuvant chemotherapy, including a 10-week treatment course of doxorubicin, cisplatin, and high-dose methotrexate was initiated. After chemotherapy, the size and appearance of the lesion radiographically remained stable, and we discussed local control options, including amputation level, with the patient and her family. After these discussions, the decision was made to proceed with a below-the-knee amputation over more distal options for a lower chance of wound complications and pressure-induced skin breakdown in the setting of required postoperative chemotherapy. A below-the-knee amputation was performed and followed by plastic surgical closure and reconstruction for distal lower-extremity nerves. This procedure was performed 10 months after the initial presentation with left foot pain. The final pathology report after the below-the-knee amputation described a 2.4-cm conventional osteosarcoma in the cuboid bone with 10% necrosis, no lymphovascular invasion, and negative margins of resection.
Two weeks after the below-the-knee amputation, the patient experienced delayed wound-healing and drainage from the incision site that prevented postoperative chemotherapy from being initiated. This was initially managed with simple wound care; however, drainage persisted for an additional 4 weeks, prompting debridement of the left lower below-the-knee amputation wound. One week after surgical debridement, the patient began a third cycle of doxorubicin, cisplatin, and high-dose methotrexate. At the 6-month follow-up, the patient demonstrated stable postoperative changes in the left leg, with no lesions present in the left leg. At the 1-year follow-up, the patient had no evidence of local recurrence and metastatic disease. The patient had also returned to daily activities with a below-the-knee prosthetic without requiring other assistive devices.
Proceed to Discussion >>Reference: Dhillon N, Vijayakumar G, Tepper SC, Braun A, Blank AT. A rare location of osteosarcoma in the cuboid bone: a case report. JBJS Case Connect. 2023 Aug 3;13(3).e22.00690.
Osteosarcoma is a malignant primary bone tumor in which tumor cells produce an osteoid or bony matrix. Most intraosseous osteosarcomas are high-grade malignant tumors that develop between the ages of 10 and 30 years. The incidence of osteosarcoma is common in adolescence, associated with the pubertal growth spurt, or, in older adulthood, related to Paget disease or previous exposure to radiation.
Osteosarcoma of the foot is an exceptionally rare presentation of a primary bone malignancy. Because of the infrequency of osteosarcoma of the foot, the literature consists of only case reports and very few small cohort studies. In a review of 52 patients at the Mayo Clinic with osteosarcoma of the foot, Choong et al. found 1 case involving the cuboid bone. Chou et al. reviewed 153 cases of foot and ankle tumors seen at a tertiary referral center specializing in orthopaedic oncology over a 20-year span, with 2 (1.3%) of the 153 tumors originating in the cuboid bone. Biscaglia et al. reviewed 1,929 cases of osteosarcoma between 1911 and 1992 at the Rizzoli Orthopaedic Institute, and only 12 cases (0.6%) were in the foot, with the calcaneus being the most common site reported. To the best of our knowledge, there have been 7 published cases of osteosarcoma originating in the cuboid bone.
Osteosarcoma of the foot differs slightly from osteosarcoma of the long bone. Patients with osteosarcoma of the foot typically are older on the initial presentation, with a mean age of 32 years (range, 6 to 89 years) at the time of diagnosis. In patients with conventional osteosarcoma, the peak age of presentation is between 15 and 20 years, which is closer to the age of our patient. Although patients with osteosarcoma of the long bones are diagnosed within months of the symptom onset, patients with osteosarcoma of the foot commonly have a long interval from the initial symptoms to the diagnosis. This may be related to the rarity of the disease in this location and the plethora of musculoskeletal sources of pain that can occur in the foot and ankle. In addition, osteosarcomas of the foot are often lower-grade than typical osteosarcomas affecting long bones, which can lead to less symptomatic but more chronic presentation.
For surgical resection of the osteosarcoma, amputation levels were discussed with the multidisciplinary tumor board as well as the patient and her family. In the cancer population, there is conflicting literature with regard to whether the Syme amputation or the below-the-knee amputation offers a higher risk profile. Our institutional experience anecdotally has shown a number of wound issues involving Syme amputation and a very successful outcome clinically with below-the-knee amputation; therefore, below-the-knee amputation is our institutional preference in these lower-extremity sarcoma cases. At the last follow-up, this patient had returned to daily activities with a below-the-knee prosthetic and had not required additional assistive devices.
In this case report, we present a rare case of osteosarcoma originating in the cuboid bone. The initial evaluation and treatment were performed at an outside institution; however, in hindsight, based on the initial MRI scan, we would have recommended histopathologic tissue diagnosis due to the appearance of the lesion. To the best of our knowledge, fewer than 10 cases have been documented to date of osteosarcoma originating in the cuboid bone. This case demonstrates the importance of biopsy to investigate problematic lesions. Generally speaking, bony lesions that are heterogeneous on imaging, especially if they involve a pathologic fracture, often require a biopsy in a timely fashion. In addition, an important learning point from this case report is that when musculoskeletal sources of pain do not heal in a typical time frame, red flags should be raised that there may be something pathologic in nature in etiology. We recommend that pathologic fractures of bone and concerning lesions be investigated properly by a trained musculoskeletal tumor team to best determine the correct diagnosis in these challenging histopathologic cases.
Reference: Dhillon N, Vijayakumar G, Tepper SC, Braun A, Blank AT. A rare location of osteosarcoma in the cuboid bone: a case report. JBJS Case Connect. 2023 Aug 3;13(3).e22.00690.
What is the diagnosis?
Osteosarcoma
Osteoblastoma
Osteoid osteoma
Changes consistent with stress fracture
Metastatic clear cell carcinoma


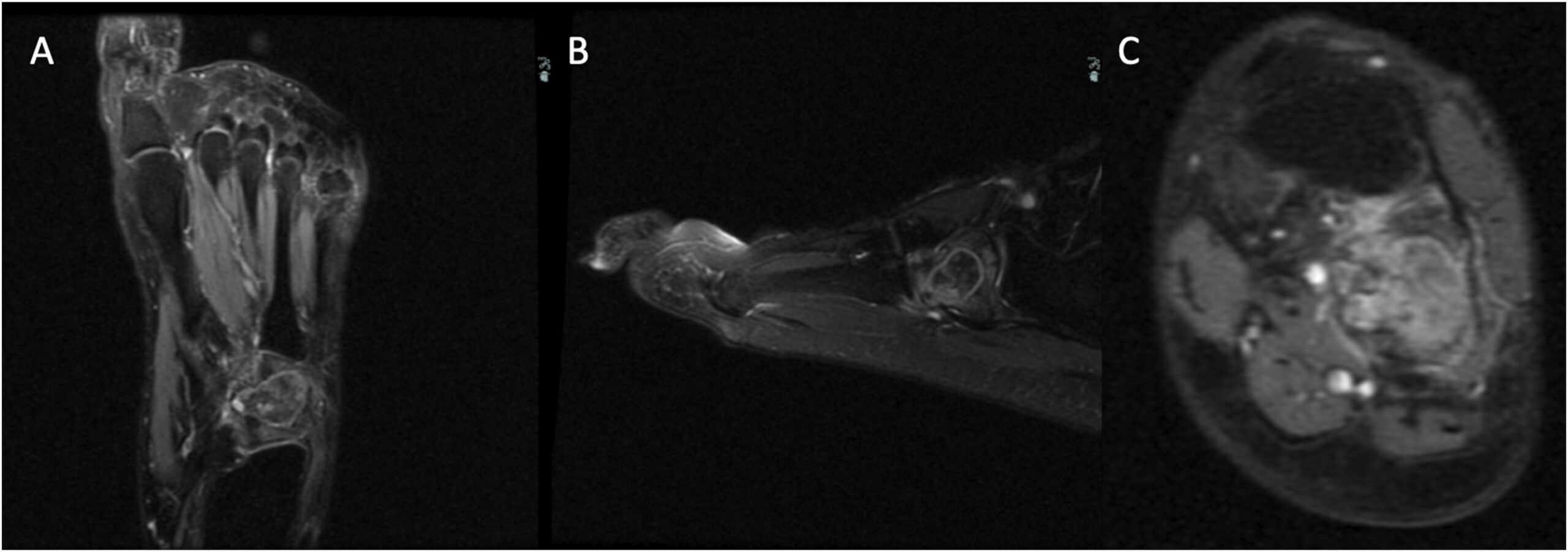
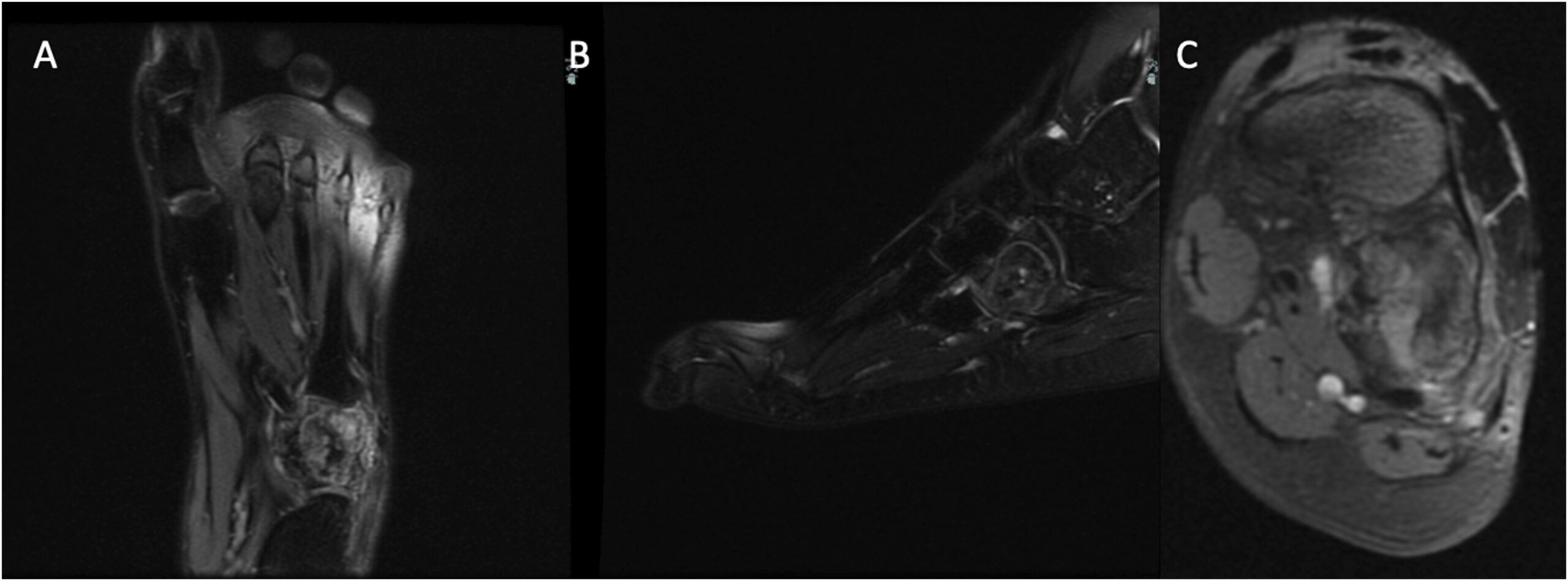

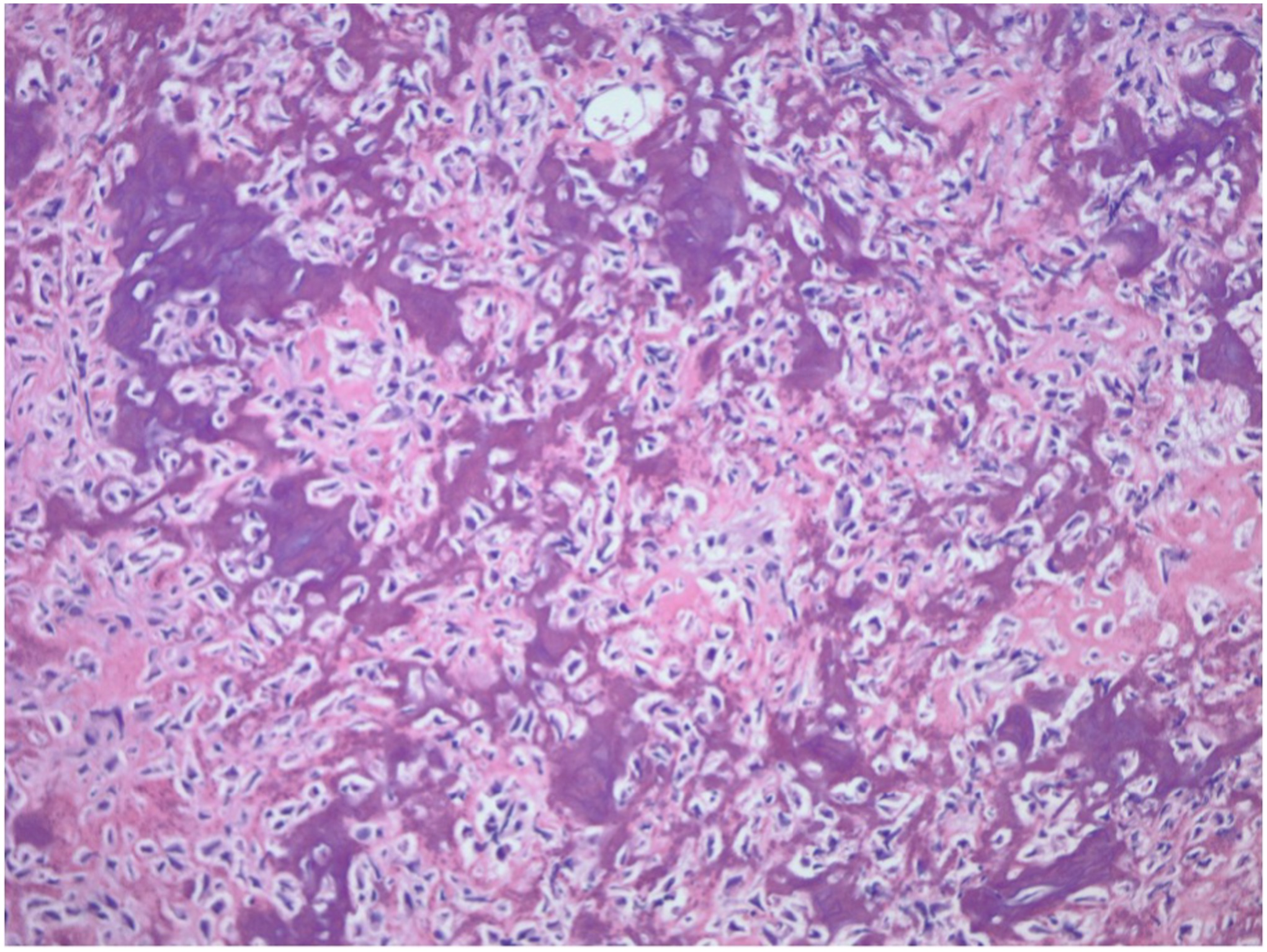
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4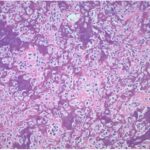 Fig. 5
Fig. 5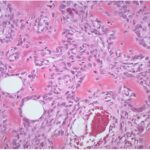 Fig. 6
Fig. 6