An 80-Year-Old Woman with Rash Surrounding Surgery Site
October 4, 2023
An 80-year-old woman with no prior skin conditions and a history of a left total knee replacement for osteoarthritis 2 years earlier presented with a 1-year history of a pruritic eruption adjacent to the surgical site. No operative complications had occurred, and the patient continued to have good function of the prosthesis, confirmed with imaging, despite rash onset. An examination revealed 1 to 4-cm brown plaques and round, erythematous scaly plaques on the left leg (Fig. 1). Before the dermatology evaluation, cutaneous fungal infection was suspected, but treatment with topical and oral antifungals led to minimal improvement. The histology of the skin biopsy is shown in Figure 2.
A biopsy revealed spongiotic (eczematous) dermatitis, clinically consistent with nummular dermatitis. Treatment with 0.05% halobetasol ointment provided sustained resolution with excellent function of the prosthesis 1 year later.
Proceed to Discussion >>Reference: Kost Y, Shokrian N, Nazarian RS, Mattis DM, Amin B, McLellan BN, Kamara E. An unexpected postsurgical phenomenon after total knee arthroplasty: nummular eczema. A case report and literature review. JBJS Case Connect. 2023 Jan 6;13(1):e22.00345.
We report a case of nummular eczema after total knee arthroplasty. The patient was an elderly woman who developed nummular eczema limited to the ipsilateral postoperative site 1 year after the surgical procedure. As in earlier reports describing postoperative nummular eczema with breast reconstruction, this patient lacked predisposing factors associated with nummular eczema, such as eczema, atopy, venous stasis, or precipitating medication. Outside of nummular eczema, cases of eczematous dermatitis of the operatively treated limb after total knee arthroplasty have been documented, first in 1975 and more recently in a case series of 30 patients. Of note, a case of a pruritic eczematous rash localized to the knee 5 weeks after ipsilateral total knee arthroplasty, later disseminated to the bilateral legs and trunk, has been described. In all patients, the lesions resolved with topical corticosteroid treatment. We highlight nummular eczema, a specific morphological subclass of eczema, which has not been described in association with arthroplasty.
There is a broad differential diagnosis of nummular eczema after orthopaedic surgery, including periprosthetic infection, cutaneous infections of tinea corporis or Majocchi granuloma, and implant-related allergic contact dermatitis. Nummular eczema may mimic periprosthetic infection because it similarly presents with erythematous, potentially edematous lesions that may be scaly and crusted because of cutaneous bacterial colonization commonly associated with nummular eczema. Infection tends to affect both sides of the vertical skin incision, whereas nummular eczema tends to be unilateral to the scar. Thorough clinical examination and screening for infection with C-reactive protein and erythrocyte sedimentation rate should be performed. If suspicion for infection is high, it should be ruled out appropriately with bacterial blood and wound cultures, as well as a joint aspiration. Microscopy preparation by a dermatologist may also be used to screen for fungal infection. If screening tests are negative, the diagnosis of nummular eczema is usually made clinically. If the patient does not respond to topical corticosteroids or if there is clinical doubt, a biopsy should be considered next.
In our case, the widespread distribution of lesions raised suspicion for infection, but clinical examination and biopsy supported nummular eczema diagnosis and treatment. Invasive measures such as knee joint aspiration for synovial white blood cell count and bacterial culture as well as hospitalization for antibiotic and surgical treatment were avoided, underscoring the importance of careful clinical examination.
Implant-related allergic contact dermatitis, a controversial entity that is believed to be a Type-IV delayed hypersensitivity reaction to immunologically active components of prostheses, may also mimic nummular eczema. The key distinction is made clinically. Although both present with an erythematous scaly rash, nummular eczema has a distinct coin-shaped morphology, whereas allergic hypersensitivity is not well-demarcated, presents symmetrically around the scar, and may be associated with swelling and pain. The 2 entities share similar features on histopathology. Workup includes testing to rule out infection as above and skin patch testing or the in vitro lymphocyte transformation test, although the latter 2 tests have been debated. Like in nummular eczema, radiologic imaging and joint aspiration are typically unremarkable. Nummular eczema should be considered before implant-related allergic contact dermatitis in such patients because the correct diagnosis of nummular eczema with appropriate topical corticosteroid treatment leads to excellent therapeutic outcomes without need for additional testing.
Numerous mechanisms underlying postoperative nummular eczema pathogenesis, including surgical manipulation of tissue resulting in transient ischemia, altered skin tension, and disruption of lymphatic channels that subsequently predisposes the skin to eczematous changes, have been proposed. Iwahira et al. suggested that transient intraoperative ischemia due to retractor use impairs sebaceous gland function, leading to disrupted skin barrier function and moisture retention, making the skin more susceptible to developing nummular eczema. In their earlier study, the group demonstrated atrophy of dermal appendages on a postoperative biopsy of breast skin in patients undergoing mastectomy, suggesting that the sebaceous gland function may be impaired postoperatively. The combination of these factors may ultimately render the skin more susceptible to developing nummular eczema. Iwahira et al. explained that compression of the skin with retractors during operations and coupled with reduced blood supply to the thoracic wall during a surgical procedure may lead to transient ischemia. Similarly, intraoperative cutaneous nerve damage leading to an altered barrier function of the epidermis and skin desiccation leading to eczematous dermatitis have been proposed to cause eczema in the first 3 to 6 months postoperatively. Our patient presented 12 months after total knee arthroplasty, demonstrating that nummular eczema can occur at varying time points.
In addition, increased skin tension postoperatively may underlie nummular eczema pathogenesis. Several reports have described recurrent nummular eczema eruption after substantial weight gain or a repeat surgical procedure in one area, both of which cause increased skin tension. Finally, it has been postulated that direct damage to blood vessels during surgery may lead to nummular eczema. Blood vessel damage is a predisposing factor for chronic venous hypertension; subsequent inflammatory changes in the vasculature result in eczematous changes appreciated clinically as stasis dermatitis. This theory is supported by the well-documented association between venous stasis dermatitis and nummular eczema. Disruption of lymphatic channels during a surgical procedure may contribute to eczematous dermatitis in knee arthroplasty. In addition to theories with regard to the etiology of postoperative eczematous eruptions, damage to the skin from lacerations, abrasions, or burns has been hypothesized to precipitate posttraumatic eczema.
Postoperative nummular eczema is a crucial diagnosis to establish because it may be misdiagnosed as surgical site infection or implant-related allergic contact dermatitis. Early and accurate diagnosis of nummular eczema in patients with orthopaedic prosthetics may prevent invasive testing and unnecessary interventions including antibiotic therapy or surgical revision, with optimal clinical outcomes and patient satisfaction. This case highlights the novel clinical presentation of postoperative nummular eczema and its varied presentation and exemplifies the wide differential diagnosis associated with postoperative nummular eczema. Given the variety of hypotheses with regard to postoperative nummular eczema pathogenesis identified in the literature, further research is required to definitively determine the etiology of postoperative nummular eczema.
Reference: Kost Y, Shokrian N, Nazarian RS, Mattis DM, Amin B, McLellan BN, Kamara E. An unexpected postsurgical phenomenon after total knee arthroplasty: nummular eczema. A case report and literature review. JBJS Case Connect. 2023 Jan 6;13(1):e22.00345.
What is the diagnosis?
Cutaneous candidiasis
Type-IV delayed hypersensitivity, most likely to nickel
Contact dermatitis, most likely related to cobalt
Eczematous dermatitis
Sézary syndrome (cutaneous T-cell lymphoma)

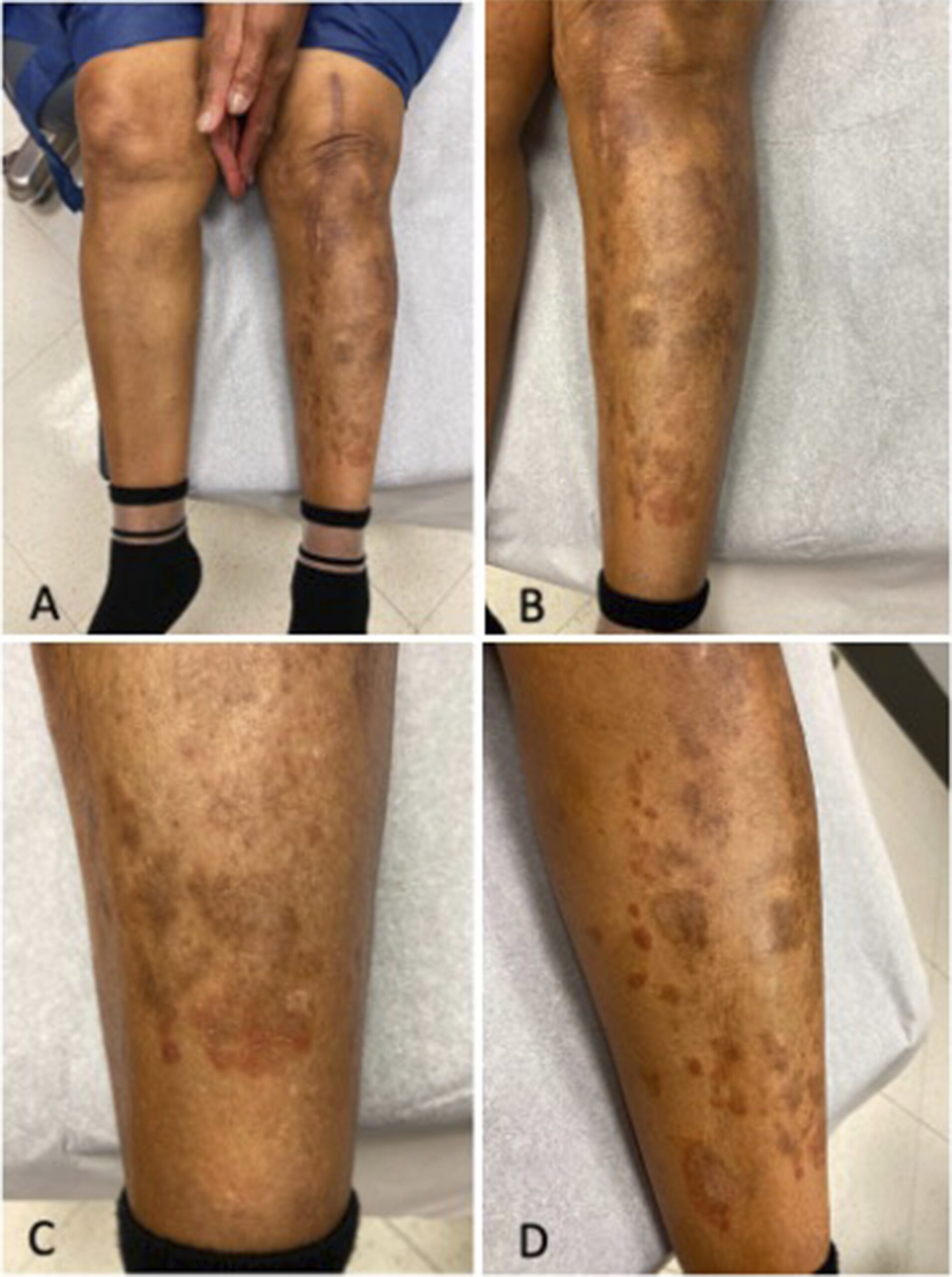
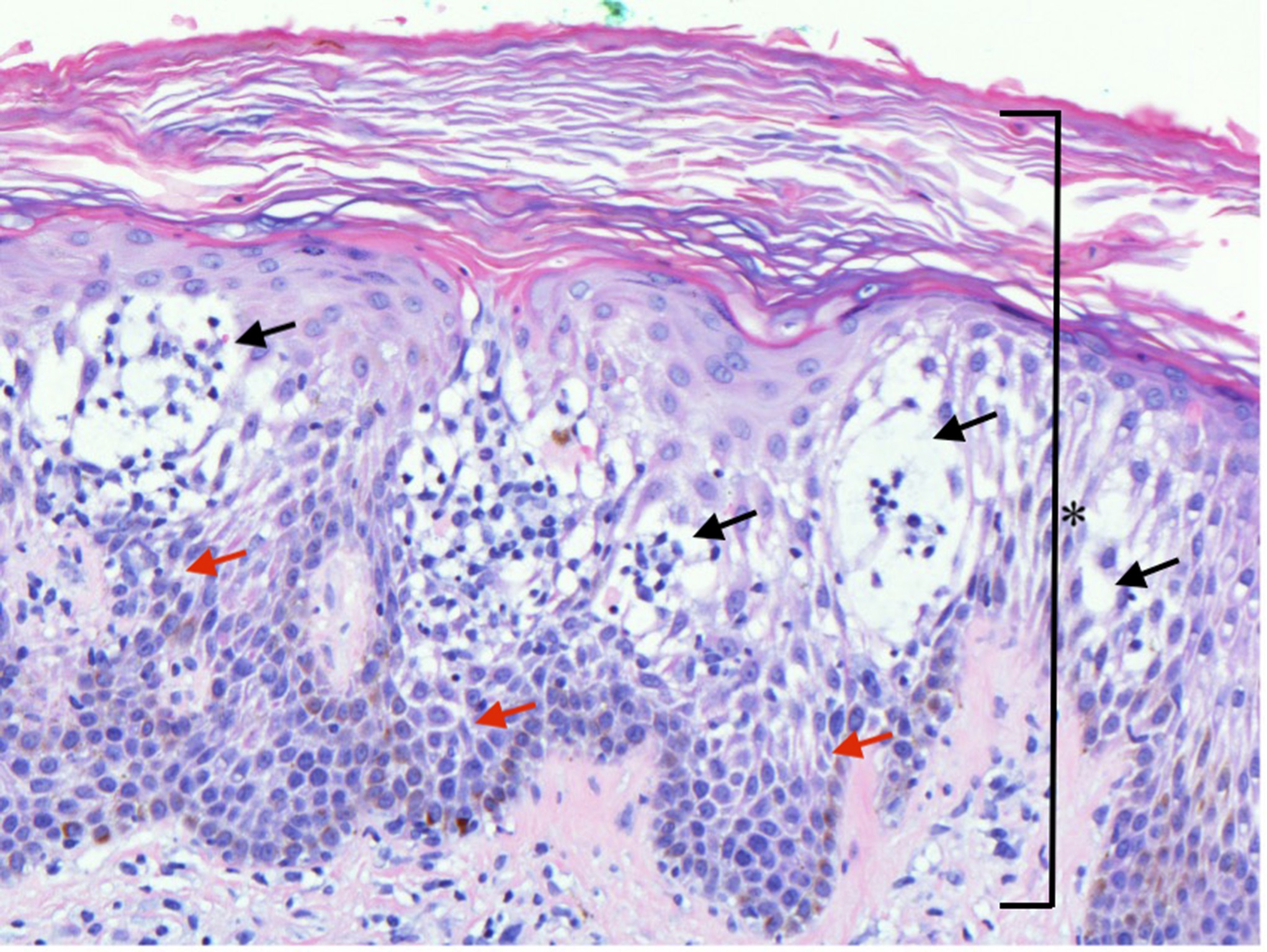
 Fig. 1
Fig. 1 Fig. 2
Fig. 2