This patient first presented at the age of 59 years with a 4-year history of right knee pain and a newly elevated alkaline phosphatase level. Magnetic resonance imaging (MRI) findings of a soft-tissue mass arising from the medial aspect of the distal femoral metaphysis prompted referral for orthopaedic oncology for evaluation for Paget osteosarcoma. The normal fatty marrow signal of the underlying distal femur was preserved, but the soft-tissue mass and thickened intracortical bone were predominantly bright on T2-weighted images, with intermediate signal on T1-weighted images. On open biopsy, it was determined to be Paget disease of bone with secondary myxoid stromal changes, with no indication of infectious processes (findings that could be interpreted as a Paget disease pseudotumor). The case illustrated the fact that maintenance of a normal fatty marrow MRI signal is a key feature to recognize non-neoplastic Paget bone despite other concerning findings. Subsequent treatment with pamidronate led to symptom resolution, normalization of the alkaline phosphatase level, and complete ossification of the affected bone and adjacent soft-tissue mass with follow-up 3 years later. Treatment was stopped after 4 infusions because of lack of patient follow-up.
Fifteen years after the initial presentation, the patient presented again with right knee pain. A radiograph and an MRI scan showed changes consistent with Paget disease and with the same extraosseous extension as previously seen. However, at this point, the region of involvement had increased to involve the distal 19 cm of the femur (Fig. 1). Abnormal and intracortical and surface signal within the anteromedial distal femoral metaphyseal cortex and surrounding associated periosteal bone was concerning for a neoplastic process (Fig. 2). In the same region, a computed tomographic (CT) scan showed cortical bone loss and periosteal new bone formation corresponding to the signal abnormality on MRI (Fig. 3). These findings were believed to be consistent with the simple progression of Paget disease. A 3-month follow-up radiograph showed maturation of the anteromedial distal femoral cortex, whereas the blade-of-grass leading edge extending proximally was suggestive of the lytic phase of Paget disease (Fig. 4). Another 3-month follow-up radiograph showed stabilization of bony changes, with lytic changes more proximal, and a focal area of sclerosis on the distal right femoral metaphysis, with no new lesions. Additional follow-up was recommended, but the patient did not return at that time.
Over the course of the next several years, the patient was treated for colonic adenocarcinoma and several other vascular and cardiovascular episodes. An alkaline phosphatase level of 373 U/L was recorded by the primary care physician 20 years after the initial presentation, but there was no record of bisphosphonate treatment.
At 24 years after the patient’s initial diagnosis and 20 years after the pseudotumor presentation, the patient’s primary care physician referred him to our clinic because of an elevated alkaline phosphatase level of 478 IU/L (reference range, 35 to 144 IU/L) and concurrent unintentional 25-pound (11-kg) weight loss over the preceding 5 years, in the context of the earlier atypical Paget behavior and concern for possible malignancy. The patient also described intermittent mild, medial-sided, distal right thigh pain. Radiographic imaging showed new lytic and sclerotic lesions in the distal third of the right femur, consistent with progression of Paget disease that the patient was experiencing (Fig. 5). Further CT imaging showed new periosteal changes in the distal 70% of the femur (Fig. 6). Upon comparison with the CT scan from 9 years prior, the bony expansion and high-grade trabecular and cortical thickening extended 33 cm from the knee joint line, showing an additional 14-cm proximal extension. The substantial proximal growth combined with the endosteal scalloping, the appearance of possible cortical destruction of the anterior medial cortex, and the periosteal reaction in the distal femoral diaphysis and anterior lateral distal femoral metaphysis once again caused concern for transformation to Paget sarcoma.
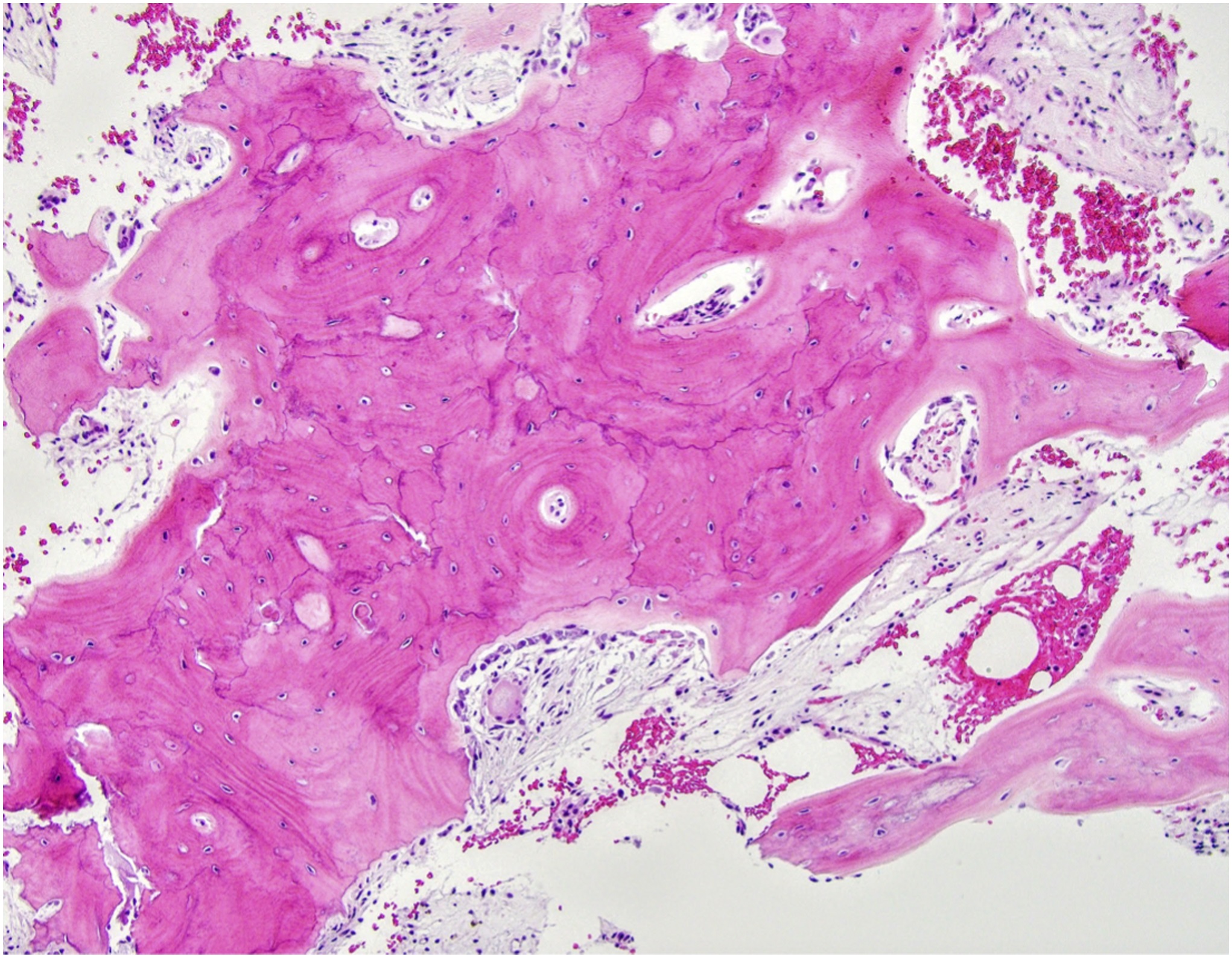
An MRI scan also showed the progressive craniocaudal involvement of the right femur, periosteal thickening and cortical irregularity with underlying intramedullary expansion, and extraosseous soft-tissue extension along the anterior surface of the mid-to-distal femoral shaft (Fig. 7). A bone-specific alkaline phosphatase level of 143.5 μg/L (reference range, 7.6 to 24.4 μg/L), C-telopeptide of 828 pg/mL (reference range, 38 to 724 pg/mL), propeptide type-1 collagen of 385 μg/L (reference range, 22 to 87 μg/L), and osteocalcin of 45.7 ng/mL (reference range, 3.2 to 39.6 ng/mL) were also elevated. To determine whether the clinical, laboratory, and radiographic changes were all consistent with uncomplicated but progressive Paget disease, a referral was made to an endocrinologist specializing in metabolic bone diseases. In the meantime, an interventional radiology-guided needle biopsy was conducted over the distal right femur, which showed normal bone elements consistent with Paget disease, and was negative for malignancy.
After consultation with a metabolic bone disease specialist, it was decided that, because of the imaging characteristics, continued pain, unintentional weight loss, and elevated alkaline phosphatase, an open biopsy should be performed in a different site from that sampled by needle biopsy to definitively exclude Paget sarcoma.
In the context of the clinical and radiographic findings, the biopsy was interpreted as showing only Paget disease with chronic inflammation and myxoid changes (Fig. 8). The bone marrow showed edema and fibrosis with no increased mitotic activity, necrosis, or acute inflammation. A follow-up radiograph, 4 months later, of the right femur showed minimal further proximal progression of the blade-of-grass leading edge toward the subtrochanteric bone (Fig. 9). However, subsequent radiographs made 1 year later showed no further progression of Paget disease (Fig. 10). Alkaline phosphatase bone-specific levels were lower, but still elevated at 124 μg/L (reference range, 7.6 to 24.4 μg/L). The patient was seen for follow-up in orthopaedics, and, at the last follow-up, continued to have chronic right lower-extremity pain. The patient continued follow-up with orthopaedics, physical therapy, and endocrinology.
Proceed to Discussion >>Reference: Bennett-Caso C, Kravtsov O, Damron TA. A case report of progressive Paget disease mimicking a malignancy: a second episode 21 years later. JBJS Case Connect. 2023 Jul 31;13(3).e.22.00694.
Paget disease is a chronic skeletal disorder with variable imaging and clinical manifestations. This report documents a 25-year follow-up of an aggressive-appearing and clinically progressive case of Paget disease of bone. This report is offered as a description of the degree to which Paget disease can progress over time and mimic malignant transformation as a pseudosarcoma. In this case, the aggressive appearance and progression may have resulted from a lack of treatment and, therefore, represent the natural progression of untreated disease, rare in this age in a developed country.
Malignant transformation of Paget disease to osteosarcoma occurs in <1% of patients. This malignancy typically presents with subacute onset of pain or increased intensity of pain, swelling, or soft-tissue extension, and it is often associated with pathological fractures and increased alkaline phosphatase. However, these features are not specific to osteosarcoma transformation and may also occur because of the progression of Paget disease, atypical manifestations, or pseudosarcomas. Other tumors reported to affect bone with Paget disease include metastatic disease, lymphoma, plasmacytoma, and giant cell tumor of bone.
Atypical manifestations of Paget disease include an unusual distribution of the lytic phase resulting in the appearance of a lytic lesion, massive lysis after immobilization, and soft-tissue extension of periosteal bone formation. Pseudosarcoma formation in patients with Paget disease can mimic malignant transformation. The localized nature of a periosteal new bone in pseudosarcomas, referred to as “pumice” bone, may be indistinguishable from malignant transformation by radiographs, especially when there is apparent soft-tissue involvement. In these cases, CT and MRI scans are indicated. On CT scans, irregular cortical penetration and destruction, bony spiculation, osteolysis, and soft-tissue mass extension favor sarcoma. Important MRI features that signal malignant development are transformation of the marrow fat signal showing a low signal on T1-weighted images and the presence of a soft-tissue mass. A normal fatty MRI marrow signal in Paget disease of bone helps to distinguish it from malignant transformation, as illustrated in this patient. Although imaging with scintigraphy or angiography to identify focally decreased bone blood flow has been suggested to identify sarcomatous transformation, these are rarely used now, and biopsy is the gold standard.
The Paget disease that this patient experienced advanced more quickly than usual, gaining 14 cm of femoral involvement over a 9-year period. Typical cases begin remodeling in the subchondral bone of the epiphysis and extend 1 cm per year into the metaphysis and diaphysis. The more rapid advancement in this patient may reflect an interruption of treatment. Although the patient was initially treated with 4 infusions of pamidronate, a second-generation bisphosphonate, missed follow-up and disruption of care because of interceding medical episodes led to an extended period of absent treatment. Hence, the atypical manifestations, in part, simply represent the natural history of untreated Paget disease. In difficult cases, such as this one, biopsy may be indicated to make the distinction. Differentiation of pseudosarcomatous change from actual malignant degeneration is obviously paramount, so the clinician should have a low threshold for biopsy.
Reference: Bennett-Caso C, Kravtsov O, Damron TA. A case report of progressive Paget disease mimicking a malignancy: a second episode 21 years later. JBJS Case Connect. 2023 Jul 31;13(3).e.22.00694.
What is the diagnosis?
Changes consistent with Paget disease
Osteosarcoma, consistent with Paget sarcoma
Atypical fracture consistent with bisphosphonate treatment
Fibrous dysplasia
High bone turnover, consistent with hyperparathyroidism


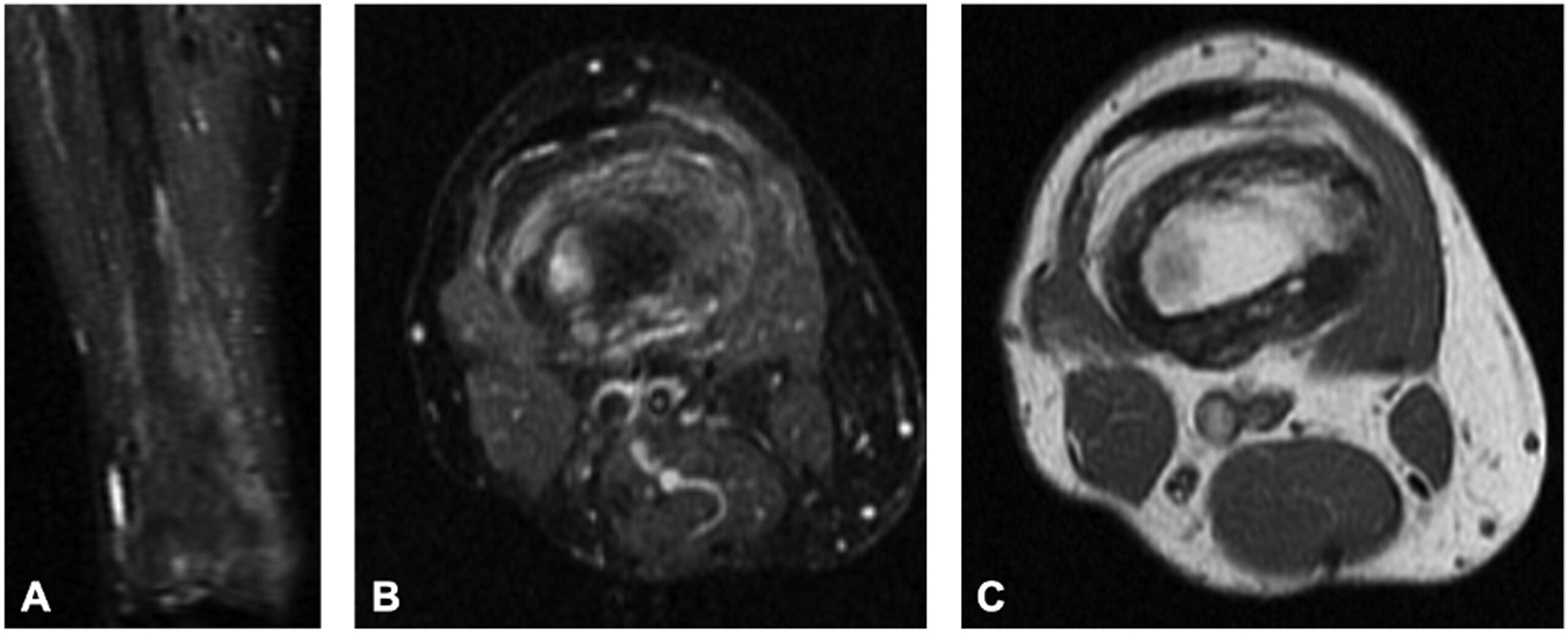
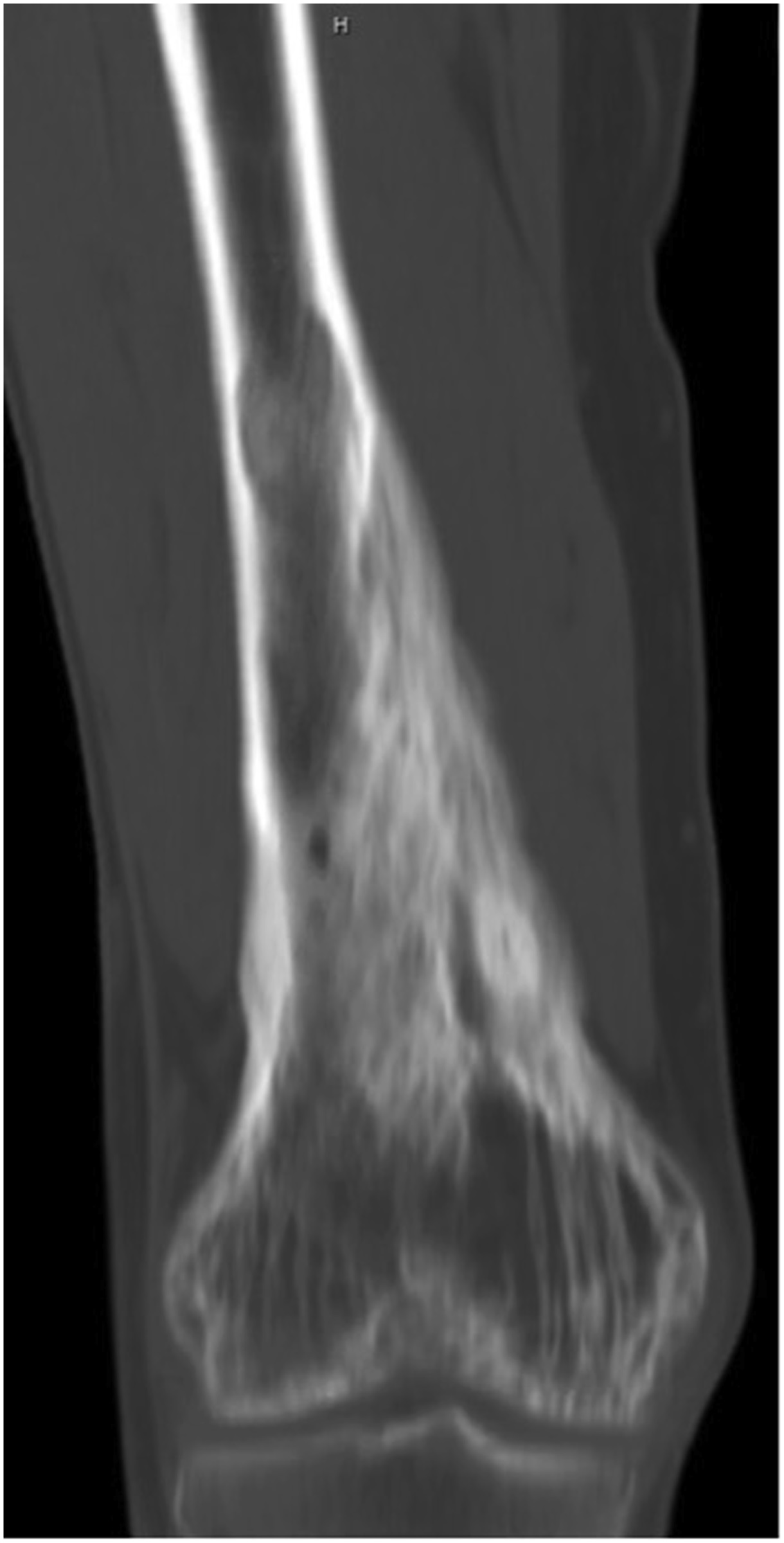

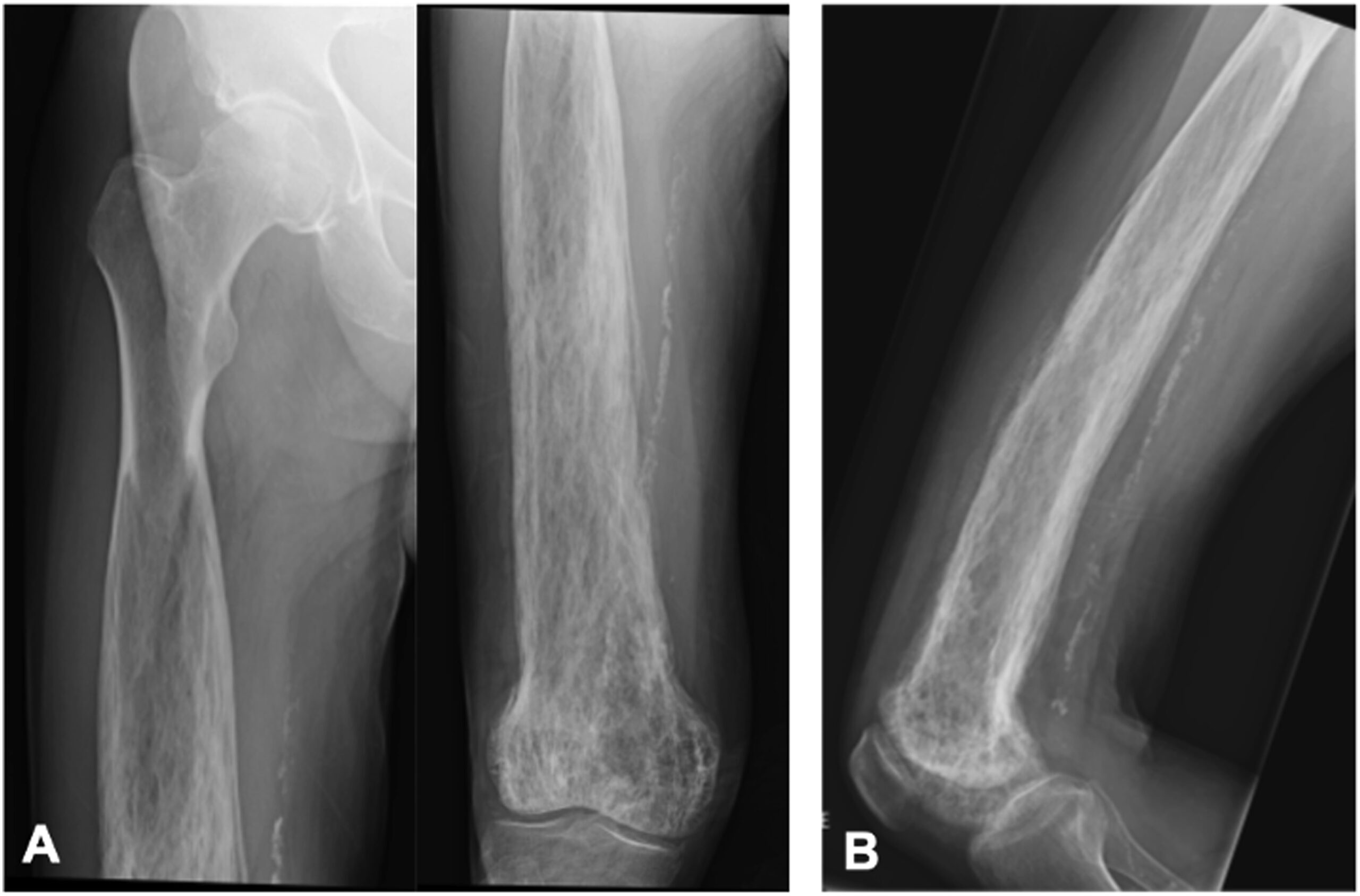

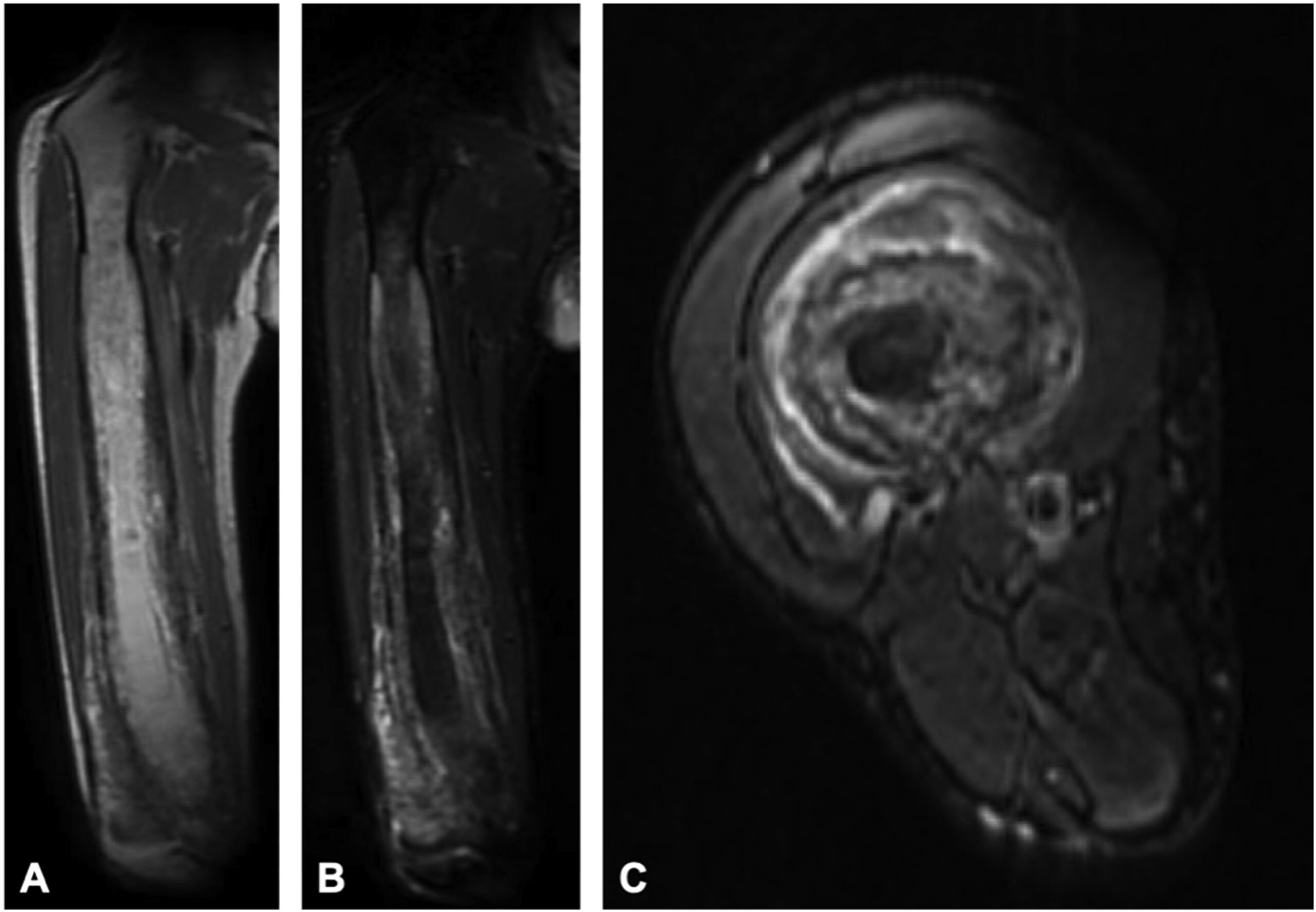
 Fig. 1
Fig. 1![Fig. 2 Fig. 2 Coronal short tau inversion recovery (STIR) (repetition time [TR]: 4,800, echo time [TE]: 14.72) (Fig. 2-A), axial STIR (TR: 6,500, TE: 13.44) (Fig. 2-B), and axial T1-weighted (TR: 516.67, TE: 8.74) (Fig. 2-C) distal femoral MRI scans show abnormal and intracortical and periosteal signal concerning for tumefactive soft-tissue extension as seen on previous images from before 2001. However, note the maintenance of the normal adjacent intramedullary marrow signal.](https://quiz.jbjs.org/wp-content/uploads/2023/12/iqdec-23-23_fig2-150x150.jpeg) Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4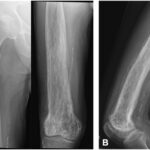 Fig. 5
Fig. 5 Fig. 6
Fig. 6![Fig. 7 Fig. 7 Coronal T2-weighted (repetition time [TR]: 5,022, echo time (TE): 64.51) (Fig. 7-A), coronal T2-weighted fast-spin echo (FSE) short tau inversion recovery (STIR) (TR: 12,303, TE: 72.38) (Fig. 7-B), and axial STIR (TR: 12,303, TE: 65.47) (Fig. 7-C) right femoral MRI scans showing proximal progression of periosteal thickening, cortical irregularity, intramedullary expansion, and tumefactive soft-tissue extension.](https://quiz.jbjs.org/wp-content/uploads/2023/12/iqdec-23-23_fig7-150x150.jpeg) Fig. 7
Fig. 7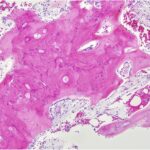 Fig. 8
Fig. 8 Fig. 9
Fig. 9 Fig. 10
Fig. 10