A 26-year-old male health-care professional presented to the sports medicine department with right-sided distal medial thigh and knee pain after exercising. There was swelling of the medial side of the knee and pain with extreme flexion. Radiographs were interpreted as a suprapatellar joint effusion but, in retrospect, demonstrated a lytic lesion in the superomedial aspect of the distal part of the femur. The patient was diagnosed with anterior knee pain and was treated conservatively. He returned 4 weeks later, with partial improvement but persistence of pain, worse with prolonged standing. There were no systemic symptoms. Examination demonstrated improved swelling and knee motion. Radiographs (Fig. 1) demonstrated a lytic lesion superomedially in the distal part of the femur, with a surrounding border and associated joint effusion. A stress fracture was diagnosed because of a history of running, activity-related pain, and some improvement with activity modifications. Due to partial improvement, no further imaging was obtained, and the patient was prescribed physical therapy.
Six months later, the patient returned with continued pain. Radiographs demonstrated a cystic bone lesion (Fig. 2). A magnetic resonance imaging (MRI) scan showed an 8-cm sharply marginated, lobulated mass in the distal right femoral metaphysis, surrounding edema, and a heterogenous fluid collection in the soft tissue posterior to and communicating with the lesion (Figs. 3 and 4). The differential diagnosis included neoplastic processes, such as telangiectatic osteosarcoma, aneurysmal bone cyst, or an atypical giant cell tumor.
At the patient’s orthopaedic visit, the only notable finding was tenderness with palpation medially and posteriorly about the thigh. He had full motion of the knee and was able to ambulate without pain.
Computed tomography (CT)-guided intraosseous and soft-tissue core needle biopsies were performed posteromedially, which demonstrated benign inflammatory tissue, but was nondiagnostic because necrotic tissue was identified. Culture samples were not obtained, and blood was not drawn to determine erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels.
Subsequently, an open incisional bony biopsy was performed through an anteromedial approach. An incision was made over the vastus medialis oblique (VMO). The VMO was split, and subperiosteal dissection was performed to allow for a bony window. Curettes were used to remove intraosseous necrotic tissue. A frozen section showed necrotic tissue. One set of culture samples was obtained. The bony window was replaced, and the incision was irrigated and closed. The patient was instructed to not bear weight.
The pathology of permanent sections demonstrated necrotizing granulomatous inflammation. Stains for bacterial, fungal organisms, acid-fast bacilli, and intraoperative aerobic and anaerobic cultures were negative. An infectious disease consultation was obtained. The patient had previously tested negative for tuberculosis and had no known exposures. Further workup, including a chest radiograph, Bartonella and fungal antibody panels, complete blood count, acid-fast bacilli blood culture, and QuantiFERON Gold were negative. Due to uncertain etiology and negative culture and stains, no antimicrobials were prescribed. The sample was sent for mycobacterial and bacterial (16s) polymerase chain reaction (PCR) analysis. No mycobacterial or other bacterial DNA was detected. The plan was to follow his examination and acquire an MRI scan in the future. Return to activity was tolerated well. Radiographs at 1 month (Figs. 5 and 6) and 3 months (Fig. 7) demonstrated a healing cavitary lesion of the medial femoral condyle without any interval progression of the lesion. An MRI scan was not acquired because of clinical improvement.
Two months later, the patient’s distal thigh became swollen with associated fevers, chills, and night sweats. The site became indurated, warm, and tender. He presented to the emergency department where fluid was aspirated with a purulent appearance and sent for culture. The blood cultures were negative. The CRP was 60.8 mg/L (reference range, 0.0 to 6.0 mg/L), and the ESR was 8 mm/h (reference range, 0 to 10 mm/h). The patient’s peripheral white blood cell count had increased from 5,300 cells/μL at the time of his infectious disease consultation to 12,400 cells/μL during this presentation. Due to the abovementioned findings, an MRI scan was acquired, which demonstrated a lesion within the distal femoral metaphysis (Figs. 8 and 9).
Although cultures and molecular testing for mycobacterial infection were negative, the inflammatory process was interpreted as osteomyelitis.
The patient was admitted to the hospital and underwent open debridement the next day. The prior incision was reopened. A second incision was made posteriorly. Necrotic tissue was encountered subcutaneously. No gross purulence was noted in deep tissue and there was no evidence of an osseous break. Curettes were used to debride the femur through a cortical window. Vancomycin calcium sulfate beads were placed in the femur to provide local elution of antibiotics, augment systemic therapy, and fill the dead space, especially because the prior treatment failed. Vancomycin was chosen because of its broad spectrum of activity, heat stability, and low allergenicity. The culture samples from the aspirate the day earlier had not shown results at the start of the operation, but postoperatively Salmonella grew on culture. Radiographs were made postoperatively (Fig. 10). In the intraoperative samples, Salmonella grew on culture as well. Pathology showed granulomatous osteomyelitis. Further workup for human immunodeficiency virus (HIV) was negative. A stool sample was negative for Salmonella or other pathogens. The patient completed a 6-week course of ciprofloxacin 750 mg twice a day.
At 4 months postoperatively, the patient resumed full activity without symptoms. Radiographs demonstrated increased bone formation in the medial distal part of the femur without evidence of periosteal reaction (Figs. 11 and 12). Repeat values for ESR and CRP were not obtained due to his clinical improvement. The 6-week antibiotic course had been completed, and he was to follow up as needed. Two years after the initial surgical procedure, the patient reported only a symptom of mild scar sensitivity. At the time of this writing, he was active, playing soccer and lifting weights without pain or limitation.
Proceed to Discussion >>Reference: Willen J, Mayer J, Habeck C, Weiner S. Chronic Salmonella osteomyelitis in a healthy, immunocompetent man: a case report. JBJS Case Connect. 2021 Dec 22;11(4):e21.00356.
Salmonella causes a variety of diseases, including gastroenteritis and typhoid fever. Salmonella osteomyelitis is well known in individuals with hemoglobinopathies and individuals who are immunocompromised. When evaluating patients with sickle cell anemia, differentiation between vaso-occlusive pain and osteomyelitis may be difficult, but the presenting signs and symptoms of osteomyelitis include vague bone pain, difficulty ambulating, fever, elevated CRP and white cell count, and soft-tissue edema.
Salmonella species most commonly involve the femur and humerus and typically only involve 1 bone. The presentation can mimic a bone tumor, including giant cell tumor, fibrous dysplasia, and lymphoma. It has been suggested that Salmonella osteomyelitis occurs after a traumatic injury. Szilagyi et al. discussed 2 cases of Salmonella osteomyelitis (1 with concomitant tuberculosis) with formation of caseating granulomas on histological specimens. They concluded that, although caseating granulomas are typical for tuberculosis, they can be found in Salmonella osteomyelitis. Muranaka et al. reported a case of a granulomatous lesion of the left ankle, and, on subsequent samples, Salmonella grew on culture. Wu et al. discussed a case of Salmonella septicemia from lumbar spine and left knee osteomyelitis. They suggested that Salmonella should be considered in cases of granulomatous osteomyelitis, especially in patients who were immunosuppressed or had hemoglobinopathies. Therefore, in cases with necrotizing granulomatous inflammation and negative tuberculosis results, Salmonella should be considered. If cultures and stains for Mycobacterium remain negative, one should consider further PCR or genomic testing for Salmonella.
Our case is one of a few cases of Salmonella osteomyelitis in a healthy individual between 20 and 40 years of age who did not have risk factors, such as travel or exposure to known animal reservoirs. Multiple risk factors for Salmonella osteomyelitis have been reported, including exposure to reptiles and travel. As far as we know, this is the first case report in which the patient was a health-care professional.
Sia et al. stated that children with culture-negative osteomyelitis are less likely to have antecedent trauma and overlying skin changes. If cultures are negative, the tissue can be sent for PCR analysis. Fihman et al. reported an overall PCR sensitivity of 73.3% and a specificity of 95.2%, whereas culture specificity was only 85.7%. Sia et al. recommended broad, empiric antibiotic coverage for culture-negative osteomyelitis.
Management of osteomyelitis due to Salmonella is not well-defined but may include surgical debridement and treatment with a beta-lactam, third-generation cephalosporin or fluoroquinolone. We recommend surgical debridement and a 6-week course of antibiotics. This allows for a tissue diagnosis, from which antibiotic sensitivities can be obtained, and for an adequate debridement. Occasionally, a radical debridement with delayed bone grafting and reconstruction may be necessary depending on the amount of tissue involved. In this case, treatment with debridement alone was ineffective and resolution occurred only after vancomycin bead placement and a 6-week course of oral ciprofloxacin. Failure to identify an organism delayed the diagnosis and treatment after 2 biopsy attempts. Therefore, consideration for culture-negative osteomyelitis should remain as a differential diagnosis for osseous lesions even with negative cultures. Sequencing should be used if the cultures remain negative and there are signs or symptoms of infection.
In patients with a suspected metaphyseal infectious or neoplastic process, osteomyelitis due to the Salmonella species should be included among the differential diagnoses, especially if there is a history of trauma to the extremity. We hope that this case report can offer an outline for providers to work up and treat cases of Salmonella osteomyelitis in healthy individuals.
Reference: Willen J, Mayer J, Habeck C, Weiner S. Chronic Salmonella osteomyelitis in a healthy, immunocompetent man: a case report. JBJS Case Connect. 2021 Dec 22;11(4):e21.00356.
What is the diagnosis?
Osteomyelitis
Granulomatous inflammation consistent with sarcoidosis
Foreign-body granulomas with bone resorption
Giant cell tumor of bone
Aneurysmal bone cyst



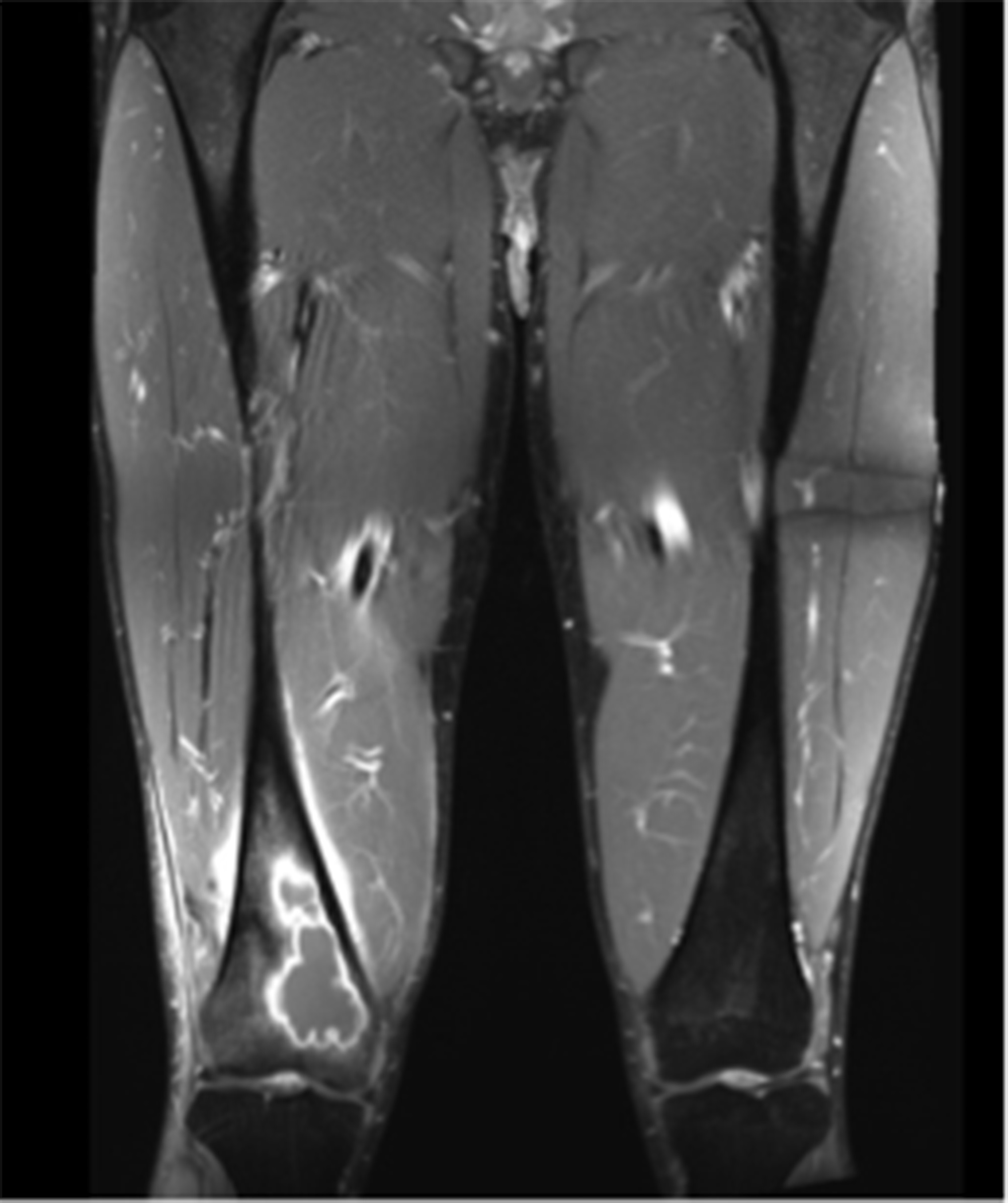
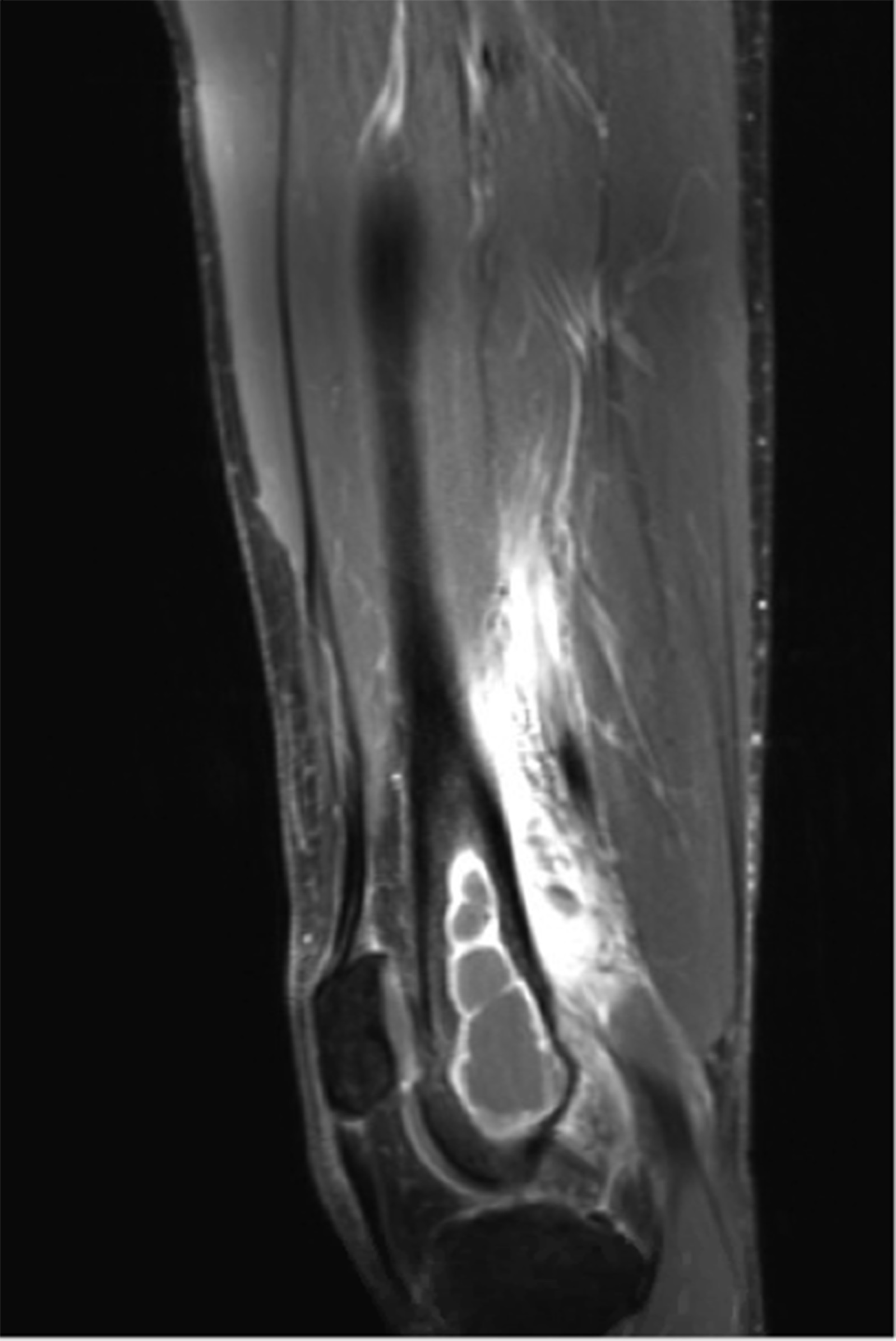



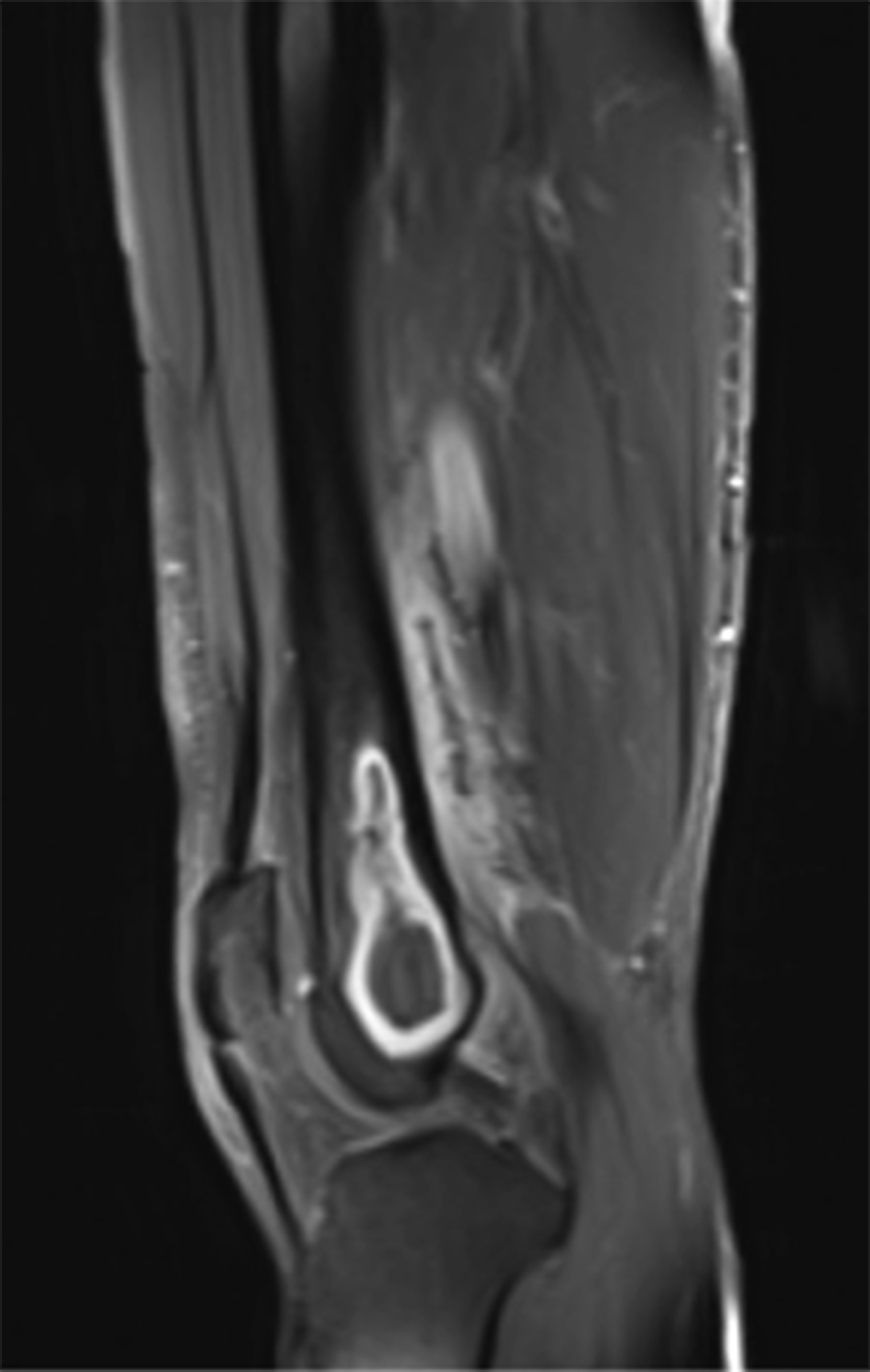
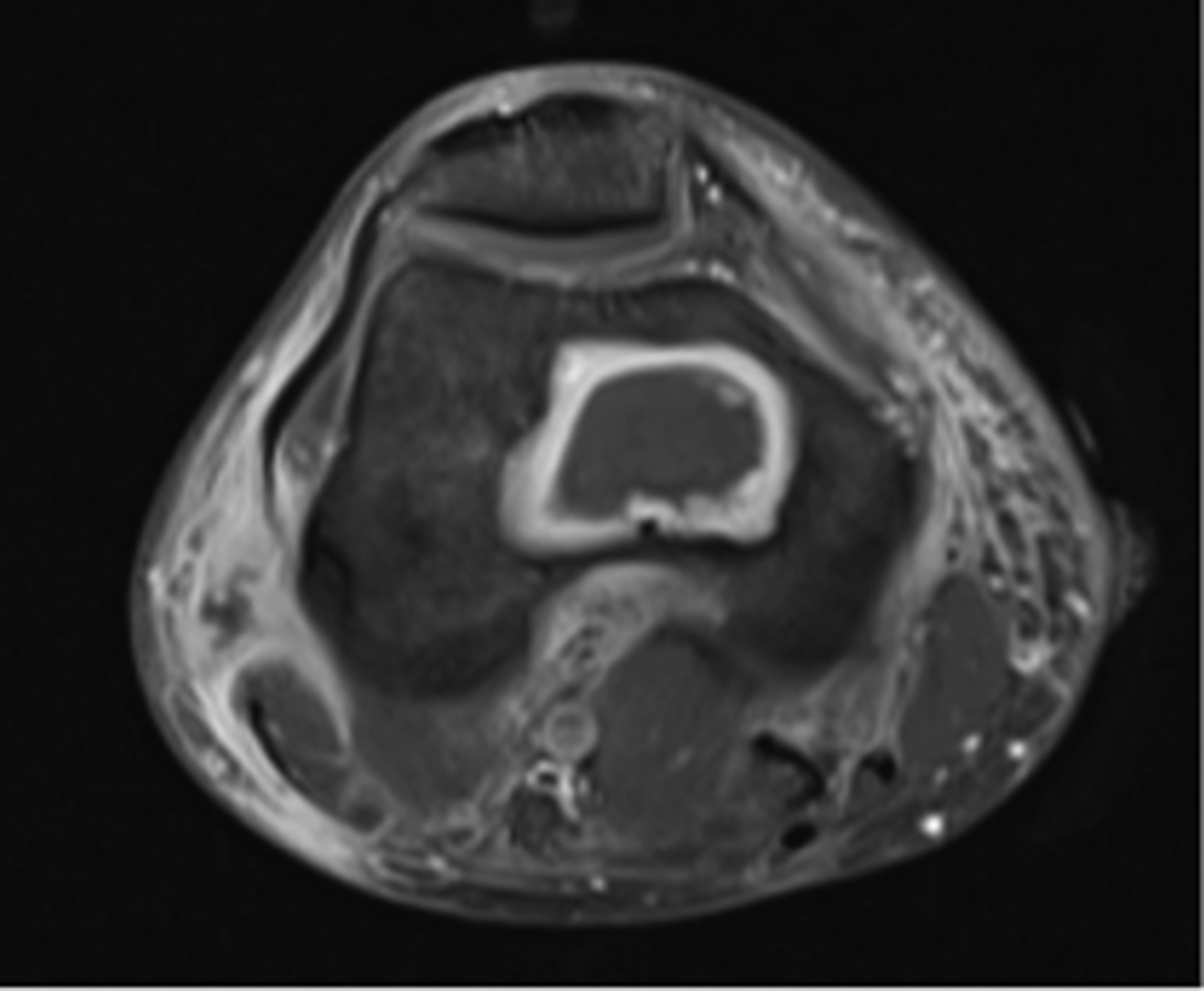
 Fig. 1
Fig. 1 Fig. 2
Fig. 2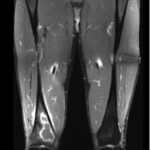 Fig. 3
Fig. 3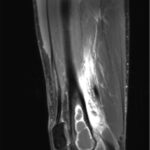 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7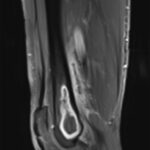 Fig. 8
Fig. 8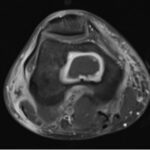 Fig. 9
Fig. 9 Fig. 10
Fig. 10 Fig. 11
Fig. 11 Fig. 12
Fig. 12

