A 35-Year-Old Man with a History of Leg Discomfort and Limp
May 4, 2022
A 35-year-old salesman was referred for treatment of a leg-length discrepancy and a limp. He was otherwise healthy, with no history of any systemic illness. He remembered having had discomfort and deformity in the right lower limb, primarily in the hip and ankle areas, around the age of 6 years. A surgical procedure had been suggested, but his parents declined the surgical procedure when the possibility of recurrence had been explained to them. The patient had never sought additional treatment.
The patient was healthy-looking and well-built (height, 180 cm; weight, 90 kg). Except for the right lower limb, the general physical examination was normal. The right lower limb was 6 cm longer than the left one, with no vascular abnormality, skin color change, or abnormality in the size of the foot or toes. When he stood and walked, the knee was in valgus, the hip was abducted, and the ankle was in equinus. The examination of the right hip revealed a flexion contracture of 60° and total flexion of 90°, along with no rotation and 30° of abduction contracture. The Harris hip score was 43. The right knee had stable, near-full range of motion. The right ankle was in 40° of plantar flexion and 5° to 10° of dorsiflexion from that position. There was no subtalar motion.
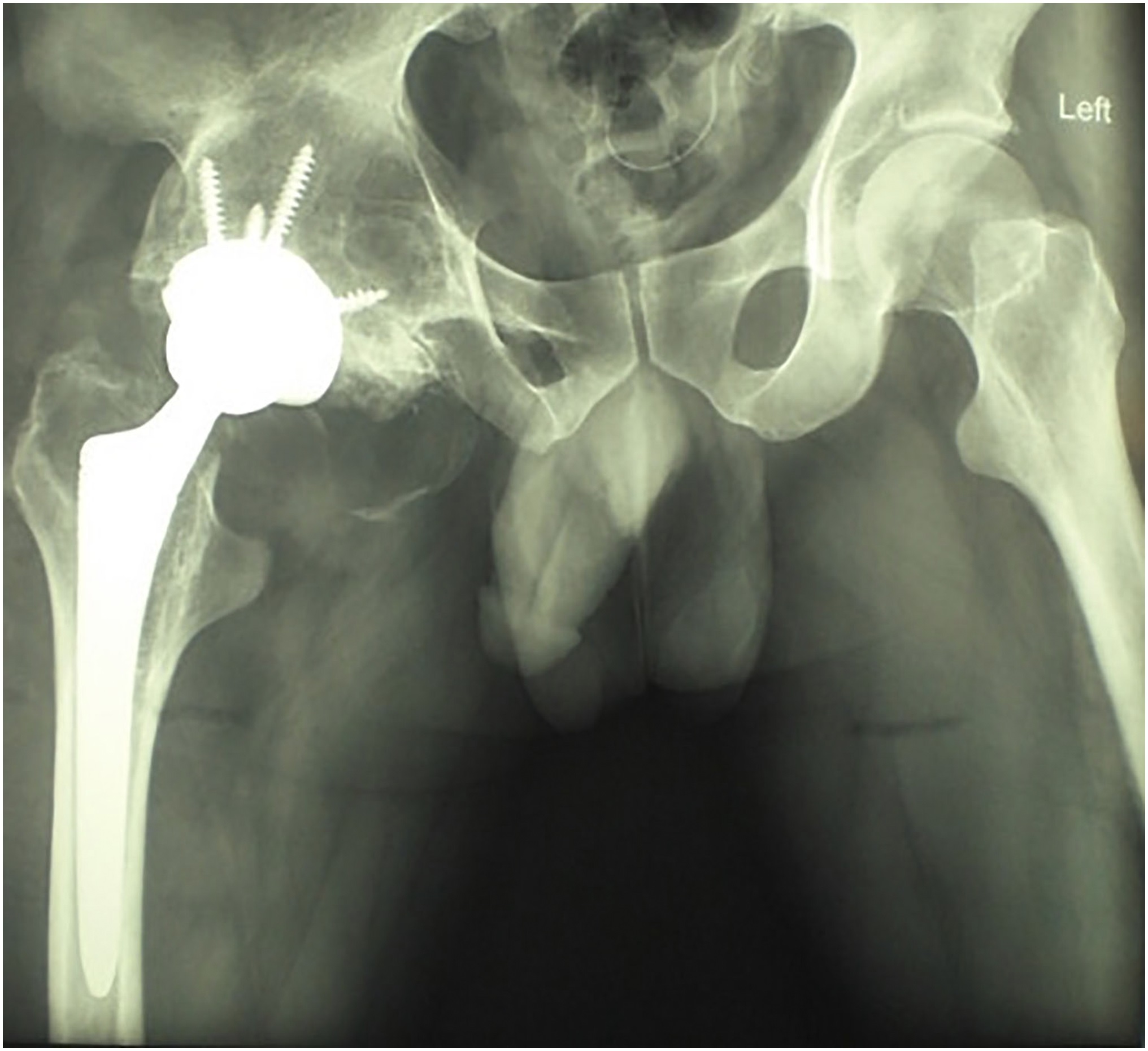
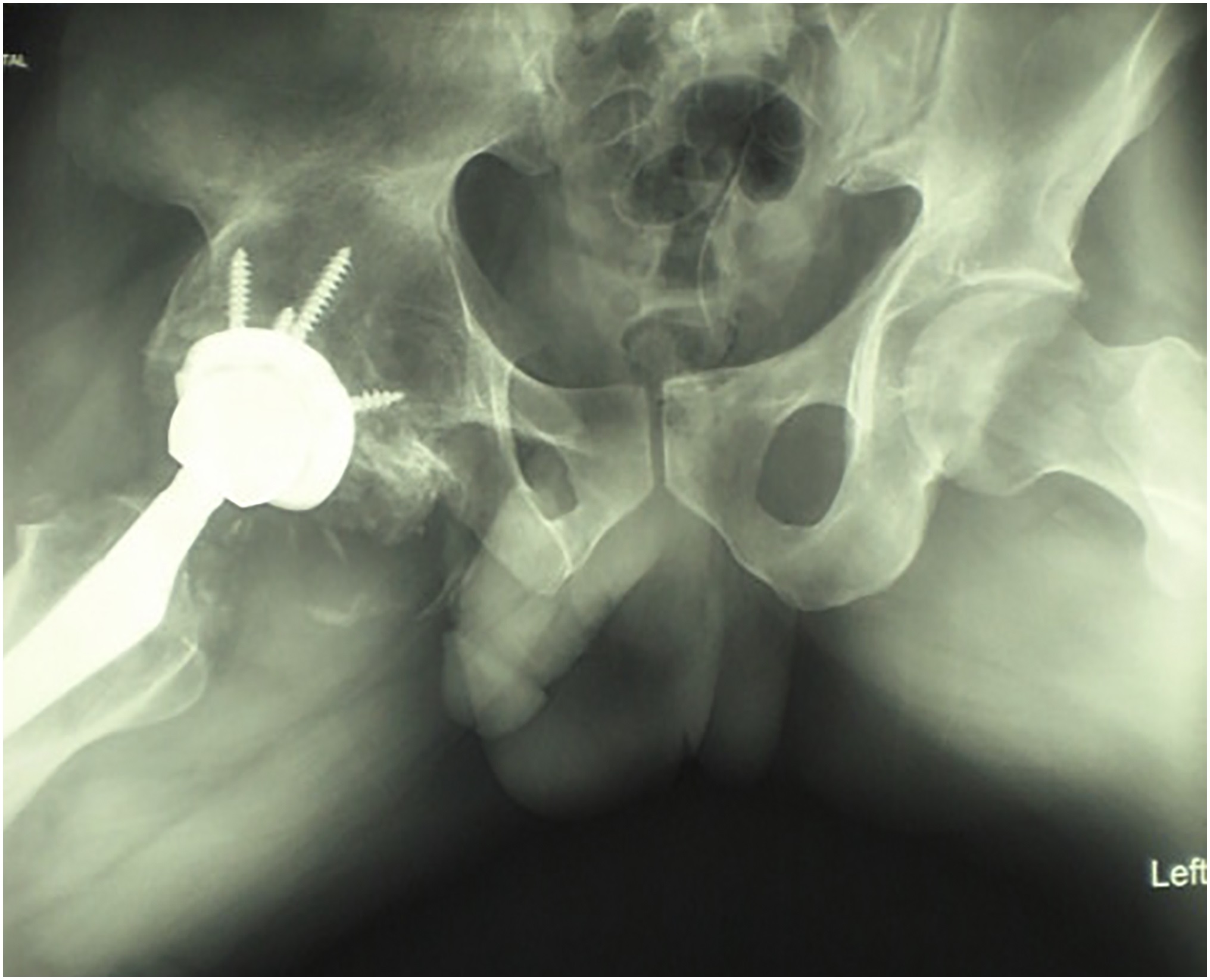
The hip radiograph showed an almost reverse ball-and-socket or flat-on-flat joint with a protuberant acetabulum, a huge, deformed femoral head, and a narrow joint space (Figs. 1-A and 1-B). Although the knee radiograph showed normal features, the ankle radiograph showed a deformed talus and tibia, with multiple huge exostoses and a fused subtalar joint (Fig. 1-C).
The gradual enlargement and the development of the deformity can be seen in the 2 poor-quality radiographs that had been made when the patient was much younger. The oldest available radiograph was made when the patient was around the age of 9 years; only the acetabular outpouching is visible (Fig. 2-A). A radiograph made when the patient was around 16 years of age demonstrates that the growing mass had started to show in the femoral head (Fig. 2-B), and the acetabular lesion was also visible. It is possible that the acetabular cartilage had been the site of the original lesions and the femoral head had become secondarily deformed, or the femoral head pathology might have appeared at a later date.
A review of radiographs made when the patient was 9 and 16 years of age helped to establish the diagnosis of dysplasia epiphysealis hemimelica (Trevor disease).
A total hip arthroplasty was planned, as well as an ankle arthrodesis that would be performed at a later date. One reason for performing the hip surgery prior to the ankle arthrodesis was the presence of the primary symptom, a painful, stiff hip. The second reason was to achieve good tissue tension and stability with the total hip prosthesis rather than equalizing the limb-length inequality at the time of the arthroplasty.
We performed the total hip arthroplasty through an anterolateral approach. During the surgical procedure, the main problems that we encountered were finding the joint, finding the base of the femoral neck for resection, deciding how much bone to remove, and deciding how deep to ream into the acetabulum. The acetabular borders and depth were hard to define. An intraoperative radiograph was made to orient us toward the acetabular center. There was no covering of cartilage on the large, flat, femoral head, which had bumpy corners, or on the protruded acetabulum, which was also bumpy at the corners. The amount of bone that was removed filled a large basin.
Following the preparation of the acetabulum and the femur, and adjusting the tension with frequent reductions with a trial prosthesis with various femoral neck lengths, a cementless hip arthroplasty was performed. We achieved very good screw fixation of the acetabular shell and a tight fit in the femoral stem, with good, stable range of motion (Figs. 3-A and 3-B). The histologic evaluation of the specimen showed normal bone and severe osteoarthritic changes, with only minimal fragmented and fibrillated cartilage. The 3-cm discrepancy that remained following the arthroplasty was corrected at the time of the ankle arthrodesis a year later. Following that procedure, the patient exhibited a plantigrade foot, and there was no more limb-length discrepancy.
At the last follow-up at 2.5 years after the arthroplasty, the patient had maintained good hip motion and function, walked with no limp, and was very satisfied. At that time, the Harris hip score was 90.
Proceed to Discussion >>Reference: Shahcheraghi GH, Javid M. The natural history of the development of Trevor disease of the hip and subsequent arthroplasty: a case report. JBJS Case Connect. 2017 Jul-Sep;7(3):e67.
Dysplasia epiphysealis hemimelica is a rare disease of epiphyseal cartilage that often affects the joints on 1 side of the body. The epiphyseal lesions evolve to resemble osteochondromas arising from the articular cartilage, which project into the joint cavity. They enlarge during the growth years and stop enlarging with the cessation of growth at maturity. They usually arise from 1 side of the joint and therefore produce angular and rotational deformities. The mechanical effect of an enlarging mass limits the joint motion, and the stimulating effect of the lesions often speeds up or, rarely, decreases the limb growth, producing a limb-length discrepancy.
The lower limb accounts for 73.2% of cases of dysplasia epiphysealis hemimelica, with a sizable proportion of the cases occurring in the ankle (particularly in the talus). The knee and the hip follow the ankle in terms of frequency of occurrence. Upper-extremity involvement accounts for 23.8% of cases, most often in the wrist, followed by the elbow and the shoulder. A scapular lesion was reported by Bigliani et al., and a glenohumeral lesion was treated with shoulder hemiarthroplasty by Braman and Stewart.
Hip involvement is not very common in patients with dysplasia epiphysealis hemimelica; it is seen in 10.3% of cases of the lower limb. Haddad et al. reported on a case that simultaneously involved the hip and the spine, in which the patient underwent a partial femoral head and neck resection at the age of 2.5 years; the dysplasia epiphysealis hemimelica quickly recurred. Arkader et al. described femoral and acetabular involvement in a patient with dysplasia epiphysealis hemimelica and suggested that the femoral side was involved more than the acetabulum, although there was no clear documentation of this. The 2 cases reported by Skaggs et al. were clearly acetabular lesions; another case described by Wenger and Adamczyk was also purely acetabular dysplasia epiphysealis hemimelica.
To our knowledge, all of the previously reported cases of hip dysplasia epiphysealis hemimelica had undergone early surgical excision for diagnosis and treatment. As previously mentioned, the hip joint is not a usual place for this disease; we believe that there have been no prior reports of untreated hip dysplasia epiphysealis hemimelica and specifically none that have been treated with hip arthroplasty. Six adult cases have been reported by Kettelkam et al., by Fairbank, and by Heiple; hip arthroplasty was not performed in any of these cases. Mendez et al. reported a case of hip disease that had undergone surgical excision in earlier childhood and had long-term follow-up. Our patient had no prior treatment and demonstrated the natural history of dysplasia epiphysealis hemimelica in a hip.
Arthroplasty for dysplasia epiphysealis hemimelica has been reported in 1 shoulder and in 1 knee. The challenges of hip arthroplasty in such a deformed hip include providing adequate but not excessive acetabular reaming to leave a sufficient rim and depth for the acetabular cavity as well as providing correct version of the cup. In our patient, the extra length of the limb also required more bone shortening at the neck, with maintenance of the proper tension of the hip abductors. We managed to build good soft-tissue tension, partly by not overreaming the acetabulum and partly by gradually resecting the femoral neck and testing the soft-tissue tension. We also had the advantage of correcting the limb-length discrepancy at a later stage with the extra bone resection that was performed at the time of the ankle arthrodesis.
In summary, dysplasia epiphysealis hemimelica, especially involving the hip, is rare. Patients usually undergo treatment in the earlier years of life for the deformities and limitation of joint motion that develop. This case report demonstrates the natural history of hip disease in a patient with dysplasia epiphysealis hemimelica, the surgical challenges, and the result of the total hip arthroplasty.
Reference: Shahcheraghi GH, Javid M. The natural history of the development of Trevor disease of the hip and subsequent arthroplasty: a case report. JBJS Case Connect. 2017 Jul-Sep;7(3):e67.
What is the diagnosis?
Dysplasia epiphysealis hemimelica (Trevor disease)
Giant juxta-articular osteochondroma
Paget disease
Stickler syndrome (Stickler dysplasia)
Metaphyseal chondrodysplasia (Jansen type)


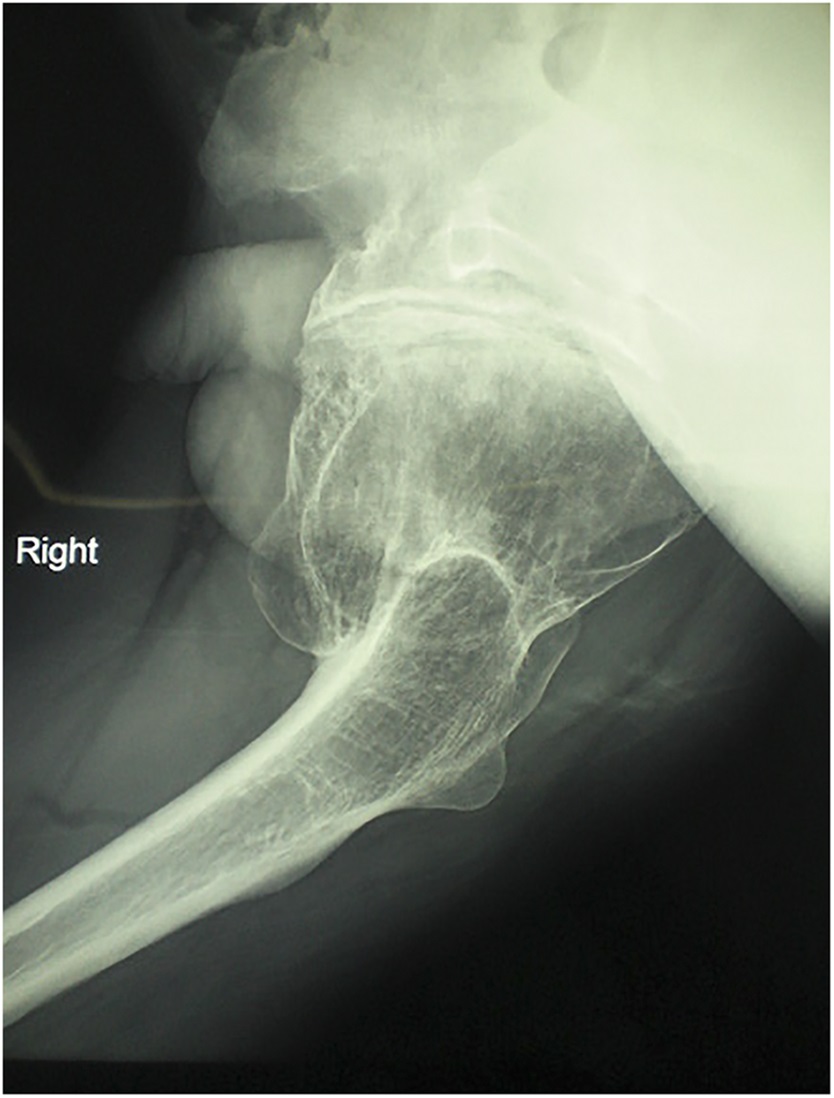


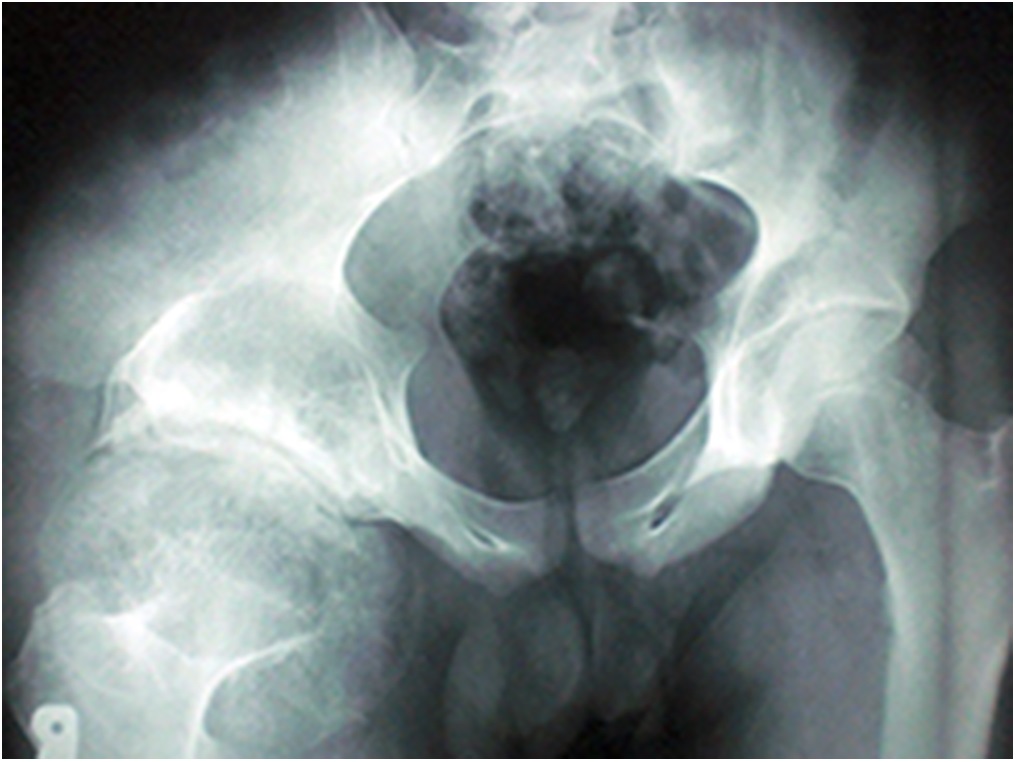
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3-A
Fig. 3-A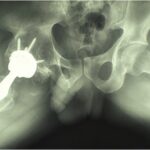 Fig. 3-B
Fig. 3-B