A 29-Year-Old Man with Nonspecific Chest Pain
September 6, 2023
A 29-year-old Hispanic man without prior medical conditions or a history of trauma presented with nonspecific thoracic pain, local tightness without radiculopathy, and neurological deficits that had lasted for a few weeks. The patient said that he did not have any constitutional symptoms such as fatigue, weight loss, or febrile episodes.
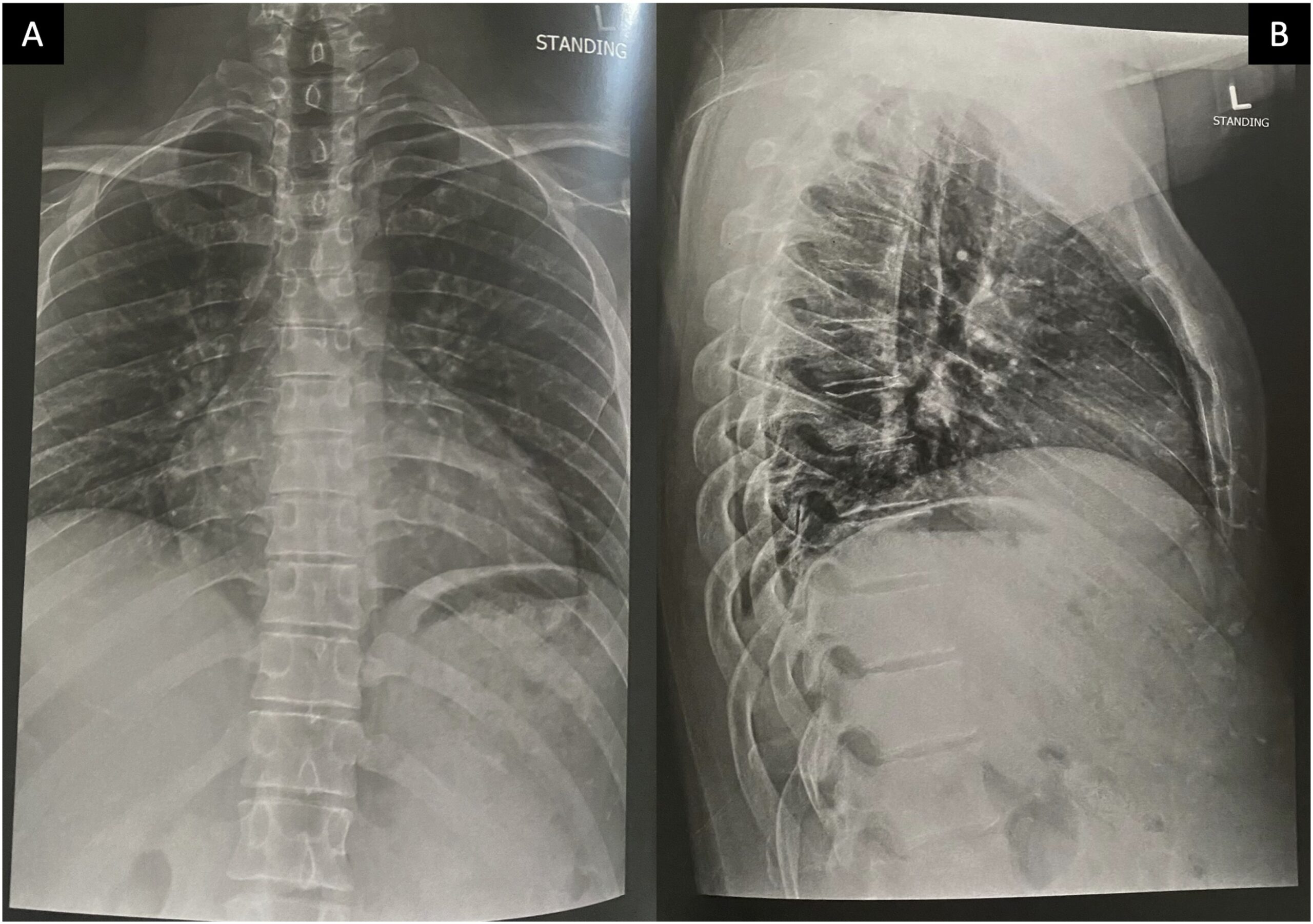
Magnetic resonance imaging (MRI) scans (Fig. 1) and computed tomographic (CT) scans (Fig. 2) without contrast of the thoracic spine showed diffuse abnormal bone marrow edema with superimposed sclerotic changes occupying the T3 vertebral body and extending into the right-sided pedicle and posterior elements. The right inferolateral cortex of the vertebral body demonstrates a cortically based lesion with peripheral hyperintensity on T2-weighted MRI scans with central sclerosis and surrounding paraspinal inflammatory changes measuring 9 × 9 mm. No associated compression fractures were noted. We explained the clinical scenario and management alternatives to the patient. He opted for surgical treatment considering that the frequent pain and constant nonsteroidal anti-inflammatory drugs (NSAIDs) were affecting his quality of life, and he wanted a permanent solution. We proceeded with an endoscopic partial corpectomy and mass resection.
Under general anesthesia, the patient was placed in a prone position, followed by the thoracic spine area cleansing and draping. A midline incision was performed over T6. The spinous process was dissected, and a clamp reference was placed. A 3-dimensional O-arm scan was performed for navigation (Fig. 3). A navigated Jamshidi needle was placed on the right T3 vertebral body, followed by a guidewire and tube dilation. A single working cannula was established to set the Joimax endoscope, and correct placement was verified with navigation and fluoroscopy. Fluid management was performed with water tower pressure at 70 mm. A partial corpectomy was performed with a high-speed diamond burr followed by curettage under direct visualization. Then the lesion site was reamed and coagulated with a radiofrequency probe (Fig. 4). The postoperative evaluation using an O-arm showed a complete resection of the lesion (Fig. 5). The wound was closed with 2-0 Vicryl and Dermabond. The patient tolerated the procedure well without complications. The pathologic assessment of the lesion is shown in Figure 6.
The imaging studies and the histology were diagnostic of an osteoid osteoma.
At the first postoperative follow-up, the patient had substantial pain improvement and no longer needed to take NSAIDs. At 1 year after the procedure, the patient was satisfied with the results, including complete pain resolution and no signs of the lesion on radiographs made at that time (Fig. 7).
Proceed to Discussion >>Reference: Mangual-Peréz D, Martínez-Rivera A, Torres-Lugo NJ, Deliz-Jimenez D, Rivera-Rodriguez G, Claudio-Marcano A, Montañez-Huertas JM, Rivera-Colón Y. Complete endoscopic resection of an osteoid osteoma in the body of a thoracic vertebra: a case report. JBJS Case Connect. 2023 Jan 12;13(1):e22.00253.
Osteoid osteomas are benign primary lesions characterized by the proliferation of bone cells, frequently affecting long bones, yet 20% of them occur in the spine. Structurally, they contain osteoblasts that produce immature bone tissue and secrete prostaglandin E2 within the lesion nidus (producing local pain, one of the main symptoms). In the spine, the posterior elements of the thoracolumbar section are the most commonly involved. The incidence is higher in male patients compared with female patients (about 3:1). The most common ages at presentation are from 10 years to early adulthood. The mean duration of symptoms before the final diagnosis is approximately 20 months because of its nonspecific nature. Most patients (80% to 100%) present with neck or back pain, mainly localized but occasionally radicular and sometimes associated with physical activity. It usually appears or worsens at night and usually responds very well to treatment with acid acetylsalicylic (AAS) or NSAIDs.
On radiographs, osteoid osteomas present as solitary lesions that are primarily osteosclerotic with or without visible nidus. Calcification of the nidus and surrounding sclerosis with low signal intensity are common on T1 and T2-weighted images. Using gadolinium during MRI, the vascular nidus can be enhanced. Spinal angiography usually reveals a nonspecific pattern of hypervascularity.
Differential diagnoses for osteoid osteoma include osteoblastoma, aneurysmal bone cyst, giant cell tumor, osteosarcoma, Ewing’s sarcoma, cartilaginous tumors (i.e., enchondroma, osteochondroma, and chondrosarcoma), and osteomyelitis. Although rare, metastases should be included in the differential diagnosis in elderly patients. A definitive diagnosis can be made with a histopathological examination consisting of a reddish-yellow nodule with osteoblasts, producing osteoid bone and tissue trabeculae interconnected with a highly vascularized fibrous connective tissue ring with various degrees of sclerosis around the lesion. Still, the location of the lesion within the spine and its imaging characteristics can differentiate it from most lesions.
Benign tumors of the spine often do not require surgical treatment unless they show aggressive behavior. A treatment algorithm begins with a thorough history and physical examination to evaluate for genetic inheritance of similar lesions and to rule out a neurovascular compromise. In some cases, observation with radiographic surveillance imaging may be used as indicated to characterize the lesion and its local effects.
The initial treatment of osteoid osteomas consists of NSAIDs or AAS. A surgical procedure becomes the treatment of choice when the patient is unresponsive to medication options. Thus, surgical indications are like those of other primary spinal tumors and include pain, deformity, tumor growth, diagnostic doubt, and complete oncologic treatment. Resection is the basis for the surgical treatment of benign tumors. Surgical resection and approaches are more technically challenging than tumors on the appendicular skeleton. Spinous processes, laminae, pedicles, and facets can be addressed through standard posterior approaches. When instability is present after resection, posterior instrumentation should be performed.
Percutaneous procedures guided by imaging have been developed and successfully implemented for the treatment of benign spinal tumors such as cryoablation, laser ablation, radiofrequency ablation, and alcohol ablation. These percutaneous techniques may have complications, including spinal instability with or without concomitant pathological fracture, focal neurological deficit, advanced coagulopathy, and systemic infection. Previous reports on minimally invasive treatments have focused on image-guided percutaneous radiofrequency ablation. This technique is currently the treatment of choice for most osteoid osteomas because of high success rates, yet there are limitations, such as the lack of direct visualization of the operative field, incorrect displacement of the radiofrequency electrode, and thermal injury.
Endoscopic surgery of the spine represents a relatively new approach for mass resection. The percutaneous endoscopic technique is widely used for degenerative spinal diseases such as disc herniation, stenosis, and facet cysts. This approach has many advantages such as minor skin incision, reduced hospital length of stay, shorter rehabilitation periods, preserved facets and pedicles, no need for fusion, macroscopic visualization of small tumors, less soft-tissue damage, and direct visualization of nervous structures. In contrast, conventional surgical approaches have accessibility limitations for more central or anterior lesions in the vertebral body, but techniques such as thoracoscopy can be considered.
Full-endoscopic techniques have been reported since 2012. Their use was aimed at treating neuropathic pain by decompression of nervous structures compressed by an expansive metastatic lesion. Biopsy and decompression of metastatic lesions of the spine were performed by transforaminal endoscopic access. In 2015, a study demonstrated the possibility of complete resection of a lesion in the lumbar spine for the first time. In the same year, the first case of resection of an epidural tumor was published.
Endoscopy has shown promising results, including the total resection of benign spinal lesions, allowing good control of symptoms, shorter hospital stays, faster recovery, and satisfactory periods in patients without disease. Previous studies have shown excellent immediate and 3-year follow-up results in 11 patients with benign lesions of the lumbar and sacral spine resected endoscopically, and another study showed that 81.3% of patients needed internal fixation after conventional open surgical resection of an osteoid osteoma. A specific study treated this type of lesion with photocoagulation and percutaneous laser ablation and found that 29.8% of patients underwent bone biopsy after ablation, with 29.4% of patients without a definitive diagnosis due to insufficient samples.
Full-endoscopic techniques protect and preserve adjacent structures, do not compromise spinal stability, allow good resection, facilitate hemostasis, and prevent recurrences. In our case, the endoscopic approach for mass resection also allows radiofrequency ablation as the Joimax endoscopic spine system usually includes this technology as a bipolar sealer for hemostasis. The application of this technique has major considerations over percutaneous radiofrequency ablation, especially the direct visualization of the lesion. This benefit is crucial to ensure complete mass resection through direct visualization without the invasiveness of an open approach but minimizing the risk of injuries to the vascular or neurologic structures of the percutaneous approach. A previous series evaluating osteoid osteoma resection had achieved complete pain relief in more than 90% of patients, hence, the benefits of mass resection as a definitive treatment for our patient. However, orthopaedic surgeons should be aware that good results with endoscopic techniques are achieved only with a considerable learning curve.
We report the successful resection of an osteoid osteoma in the body of a thoracic vertebra through a complete endoscopic approach. This minimally invasive technique represents an adequate and cost-effective approach for the complete resection of these benign lesions. Further studies with larger samples and longer postoperative follow-ups are needed to compare this endoscopic technique with other therapeutic options.
Reference: Mangual-Peréz D, Martínez-Rivera A, Torres-Lugo NJ, Deliz-Jimenez D, Rivera-Rodriguez G, Claudio-Marcano A, Montañez-Huertas JM, Rivera-Colón Y. Complete endoscopic resection of an osteoid osteoma in the body of a thoracic vertebra: a case report. JBJS Case Connect. 2023 Jan 12;13(1):e22.00253.
What is the diagnosis?
Osteoid osteoma
Giant cell tumor
Chondroblastoma
Osteofibrous dysplasia
Brodie abscess

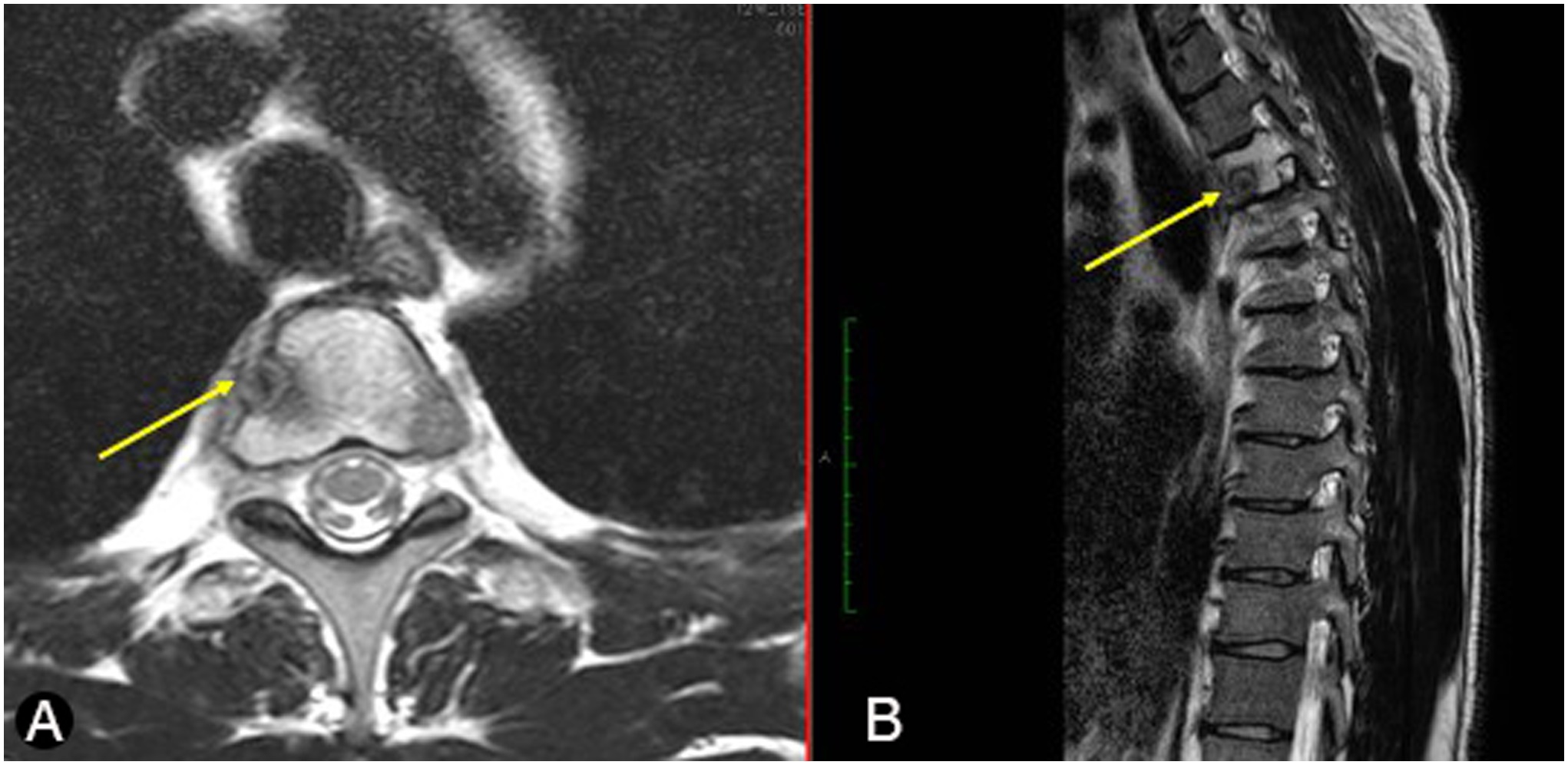
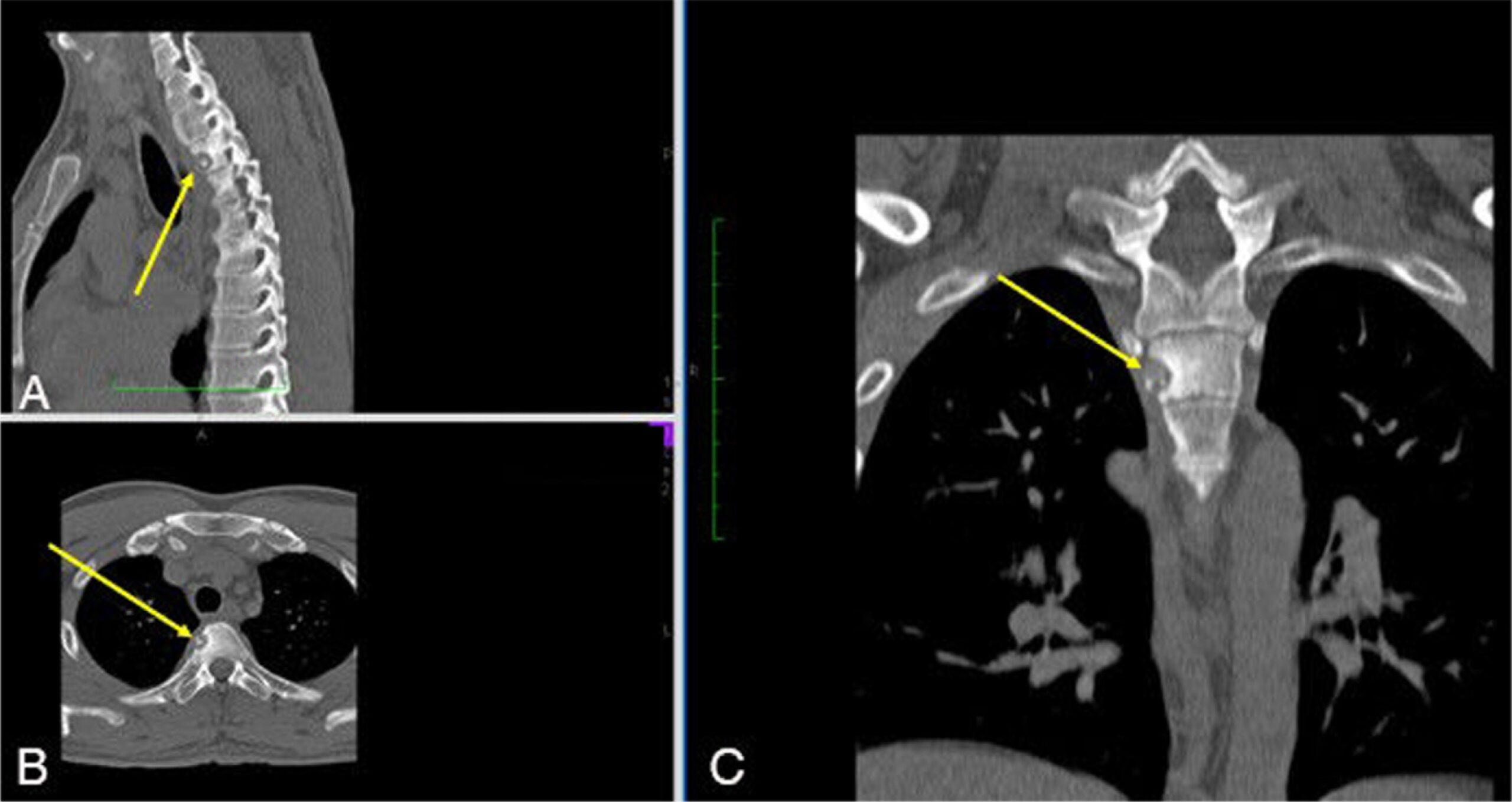
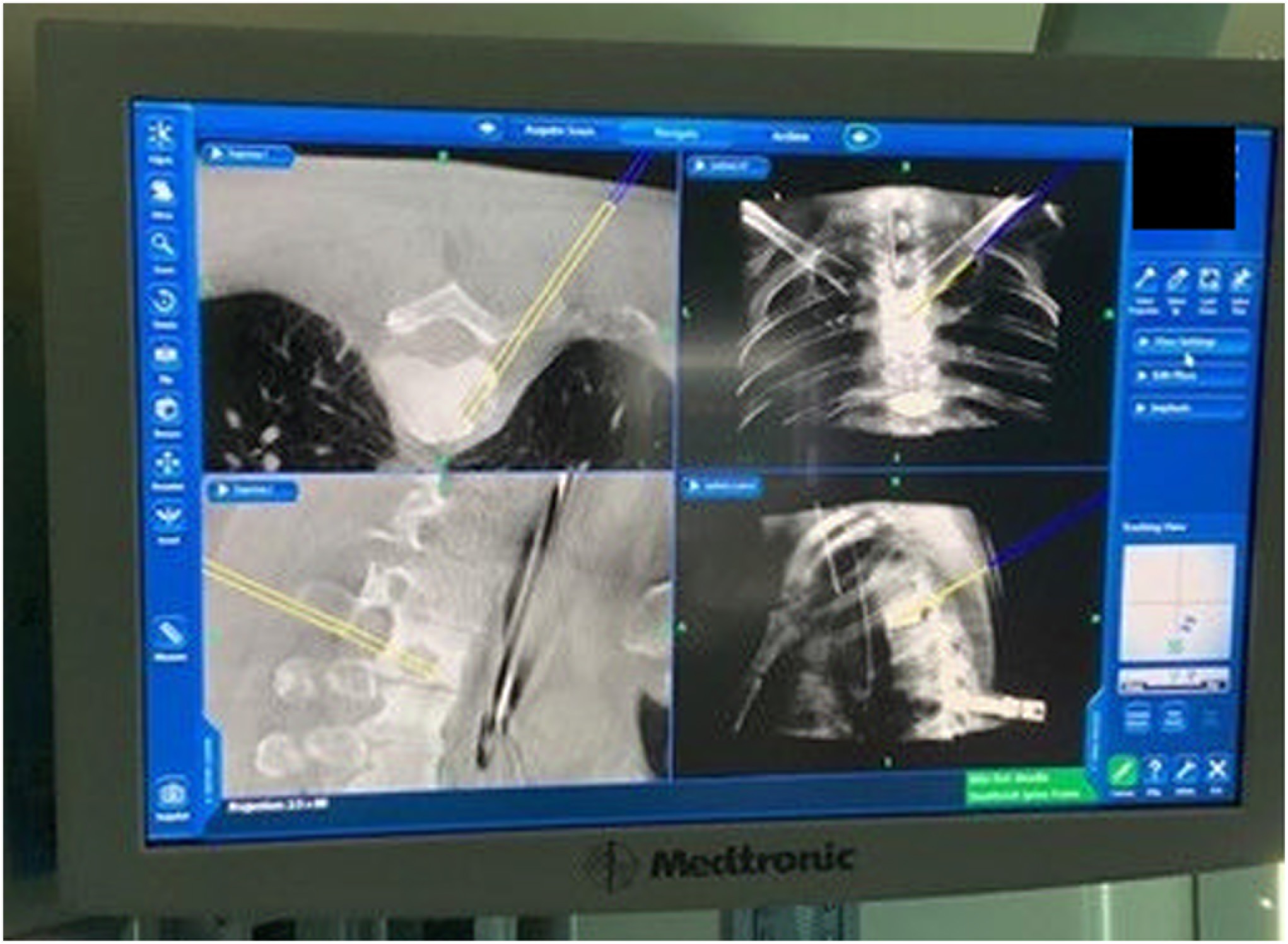
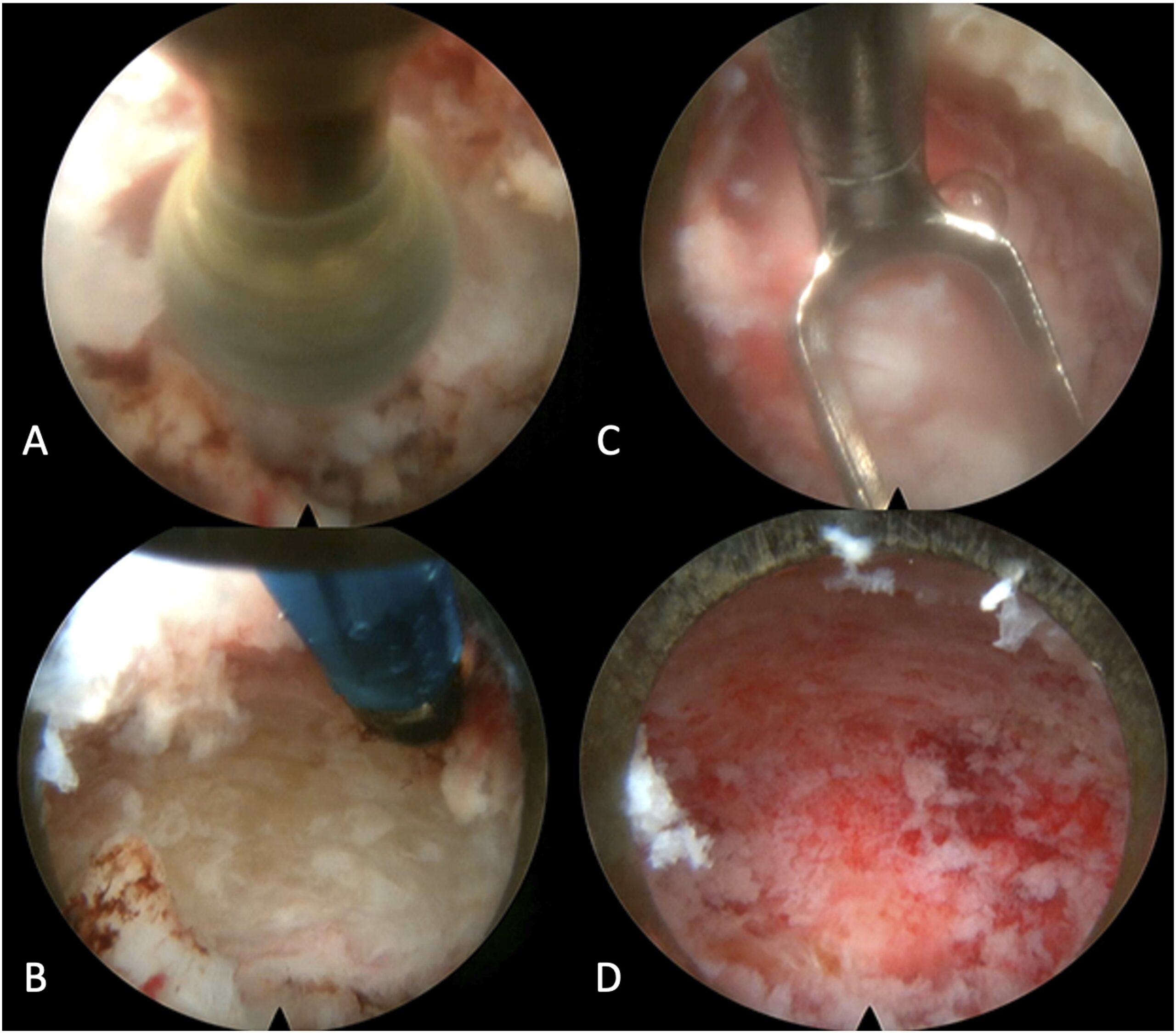
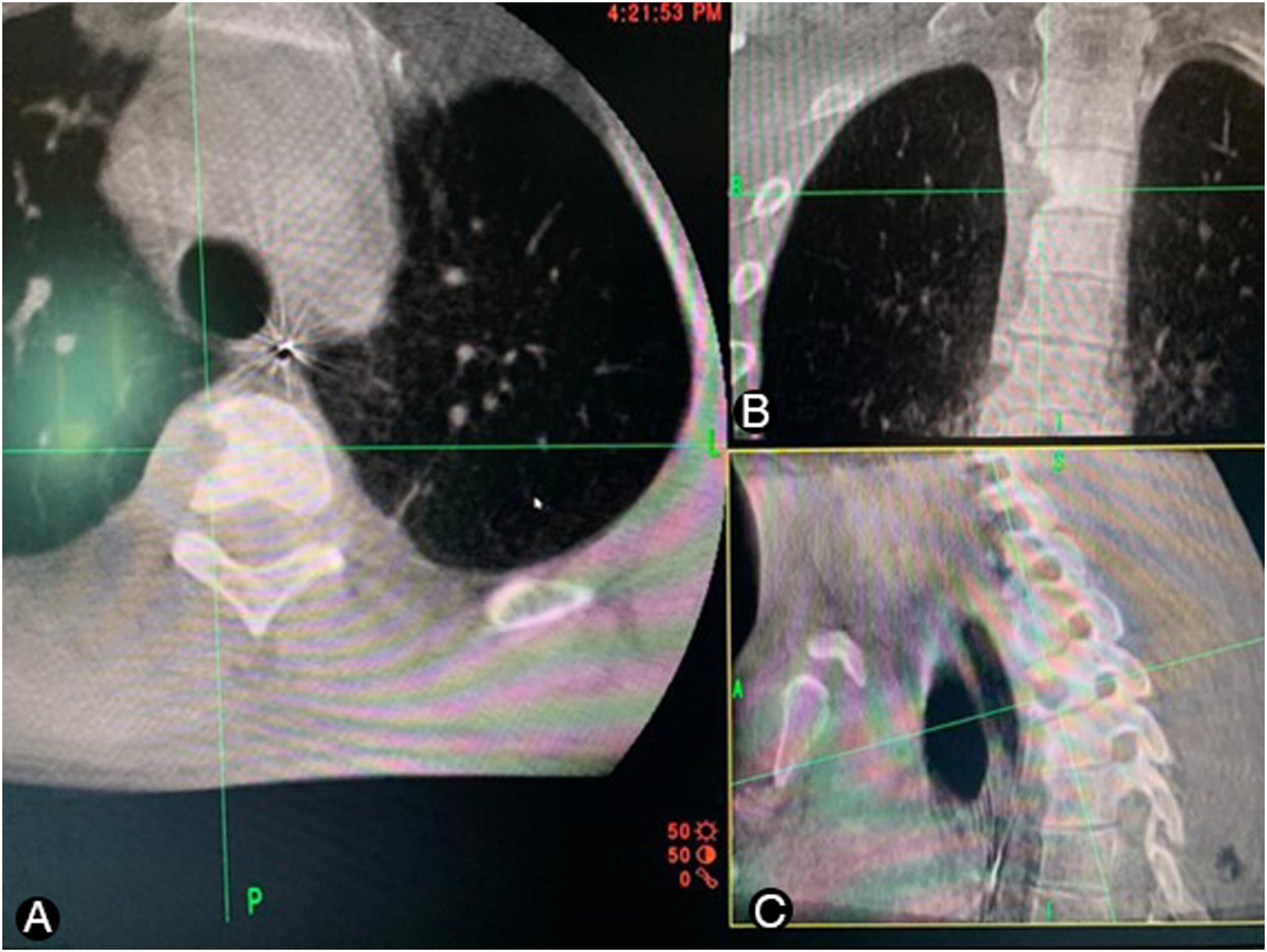
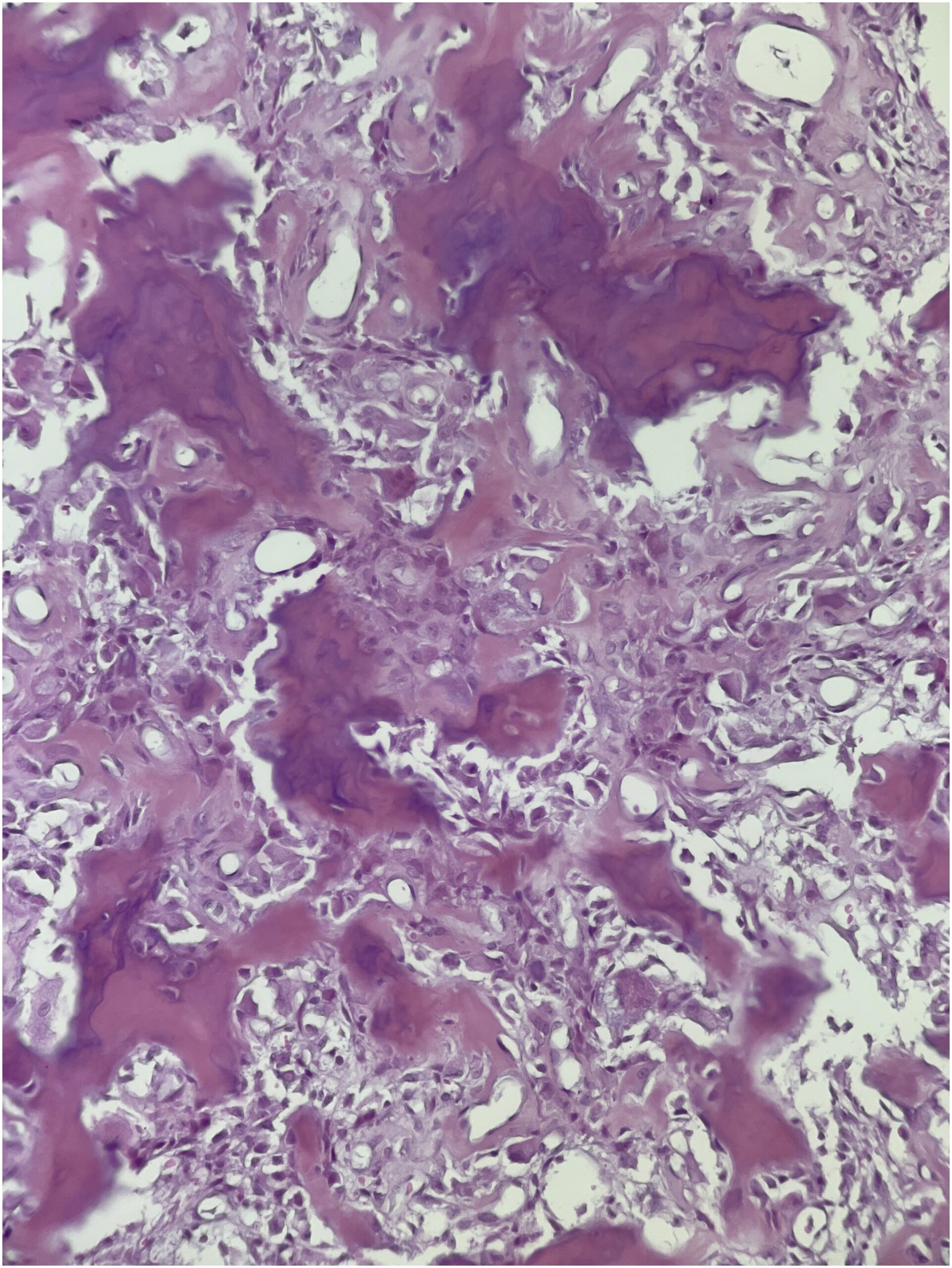
 Fig. 1
Fig. 1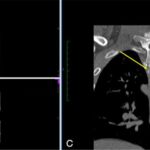 Fig. 2
Fig. 2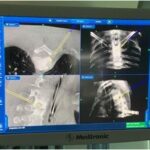 Fig. 3
Fig. 3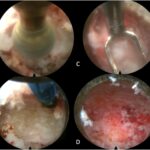 Fig. 4
Fig. 4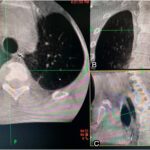 Fig. 5
Fig. 5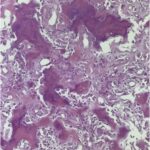 Fig. 6
Fig. 6 Fig. 7
Fig. 7