A 32-year-old woman presented with right thigh pain that she had experienced for 6 months. She was evaluated at a local hospital with imaging and underwent an open biopsy, after which she was referred to our institute. Her clinical examination was essentially normal except for a scar from the open biopsy. Radiographs of the femur showed an ill-defined diaphyseal lesion with a screw that had been used for the refixation of the cortical window made during the open biopsy (Fig. 1). The magnetic resonance imaging (MRI) scan showed a T1 isointense, short tau inversion recovery (STIR) hyperintense, elongated, intramedullary lesion in the diaphysis of the femur with a length of 19 cm. There were additional lesions in the neck of the femur and the distal metaphysis. Computed tomographic (CT) images revealed endosteal scalloping and intramedullary enhancing soft-tissue lesions with matrix calcification in the diaphysis of the femur (Fig. 2). A bone scan revealed an uptake in the diaphysis of the right tibia and a minimal uptake in the proximal right part of the tibia in addition to the lesion in the femur (Fig. 3). A radiograph of the right tibia showed an ill-defined lesion in the distal diaphysis (Fig. 4). The proximal part of the tibia was normal in the radiograph and the MRI scan, and the minimal uptake in the bone scan was believed to be due to the physiological causes, such as alteration in gait. The MRI scan of the tibia revealed a diaphyseal intramedullary lesion that was hypointense on a T1-weighted sequence and hyperintense on STIR images. A positron emission tomography (PET) CT scan did not reveal any systemic metastasis (Fig. 5). An image-guided biopsy was performed on the tibial diaphyseal lesion (Fig. 6).
The biopsy was interpreted as grade-2 chondrosarcoma, so, in the context of radiographic findings, the patient was diagnosed with synchronous multifocal chondrosarcoma.
This case was discussed by a multidisciplinary tumor board, and it was decided to perform the surgical procedure in a staged manner. The patient underwent intercalary resection of the tibial diaphyseal lesion first. We preferred biological methods of reconstruction for the defects after intercalary resection because it has the advantage that, once it is incorporated with the host bone, it is a lifelong solution and is not associated with the complications of using an intercalary prosthesis. The methods of biological reconstruction available were the reimplantation of sterilized tumor bone, allograft reconstruction (not feasible in our setting because of the nonavailability of allograft), and vascularized fibula grafting. The latter has the advantage of osteogenic potential; early osseous union; predictable vascular pedicle; ability to harvest as a composite flap along with skin, fascia, and muscle; and potential for hypertrophy. However, it has many disadvantages, including donor site morbidity, prolonged operating time, requirement of microvascular surgeon, and poor strength of the graft. In this patient, reconstruction of the defect was performed by reimplanting the irradiated tumor bone. After wide excision, all the gross tumor tissues were removed from the tumor bone and were then sent for irradiation with 50 Gy in a single fraction. The medullary cavity of the irradiated bone was filled with bone cement, and it was reimplanted with plates and screws. This biological method was preferred because it provides an exact match to the resected bone. One month later, the patient underwent total femoral excision with adequate margin and total femoral replacement.
The patient’s postoperative period was uneventful. Non-weight-bearing mobilization was started in the immediate postoperative period, and protected weight-bearing mobilization with the patellar tendon-bearing brace was started at 6 weeks after total femoral replacement. At the 38-month follow-up, the patient was free of disease (Fig. 7). She is ambulant with a Musculoskeletal Tumor Society (MSTS) score of 26.
Proceed to Discussion >>Reference: Paul M, Sugath BS, P S, Np P, Nair SG, Rajasekharan R. Synchronous primary multifocal skeletal chondrosarcoma of extremity: a report of 2 cases. JBJS Case Connect. 2022 Feb 16;12(1).e21.00176.
Multiple chondrosarcoma is commonly described in the setting of multiple enchondromatoses. Secondary multiple chondrosarcoma (synchronous or metachronous) can develop in the setting of Ollier disease (multiple enchondromatoses). We considered Ollier disease as a differential diagnosis of our patient, but in Ollier disease, a skeletal survey will usually reveal multiple enchondromas and deformities. In our case, no such lesions were identified elsewhere in the skeletal system, and, hence, the diagnosis of Ollier disease was ruled out. Synchronous bone involvement can also occur in cases with skeletal metastasis at presentation, but this situation is almost always associated with lung metastasis. It cannot be said with certainty that the secondary lesions in our patient were not metastasis from the larger primary lesion, but all lesions were seen in the same or adjacent sclerotome. This may point toward congenital errors in the development of an embryo as an etiology for the development of multiple primary lesions and favors the diagnosis of a synchronous primary tumor rather than metastatic disease, especially as no pulmonary metastases were identified. Another point is that our patient remained free of disease at the 38-month follow-up, which would be unlikely in the case of metastasis.
We are aware of only 3 previous case reports of multifocal synchronous skeletal chondrosarcoma. In 1996, Damron et al. described 8 patients with multifocal chondrosarcoma; of these patients, 3 had synchronous multifocal chondrosarcoma. Each of the patients with synchronous chondrosarcomas had single bone involvement (2 cases with femoral involvement and 1 case with tibial involvement). The authors observed that patients with synchronous monomelic chondrosarcoma had better prognosis than metachronous nonmonomelic involvement. Prasad et al. reported another case of multifocal grade-1 chondrosarcoma involving the body and symphysis of the mandible, which was treated with segmental mandibulectomy and curettage of smaller lesions. All 4 patients had lesions in a single bone, and these may be skip lesions rather than a true synchronous malignancy. Manfrini et al. reported a case of a 43-year-old man with clear cell chondrosarcoma of the proximal part of the humerus with a synchronous lesion in the contralateral distal femoral condyle. The patient was treated with wide local excision of the proximal part of the humerus with allograft bone reconstruction and extended curettage of femoral condylar lesion at the same appointment. He was free of disease at the reported 10-year follow-up, which shows that the smaller lesion was not a metastatic lesion.
An interesting learning point in this case report is the role of PET-CT in the evaluation of chondrosarcoma. In our patient, a head-to-knee PET imaging missed the tibial lesion, although, fortunately, we could detect it in the bone scan (Fig. 3). This supports the need for adequate head-to-toe imaging in musculoskeletal oncology whenever indicated.
Although rare, the possibility of multifocal primary skeletal chondrosarcoma should be kept in mind during the workup of a patient with chondrosarcoma, and, if present, each lesion should be approached individually.
Reference: Paul M, Sugath BS, P S, Np P, Nair SG, Rajasekharan R. Synchronous primary multifocal skeletal chondrosarcoma of extremity: a report of 2 cases. JBJS Case Connect. 2022 Feb 16;12(1).e21.00176.
What is the diagnosis?
Ollier disease
Dedifferentiated chondrosarcoma
Polyostotic fibrous dysplasia with chondroid metaplasia
Synchronous multifocal chondrosarcoma
Maffucci syndrome

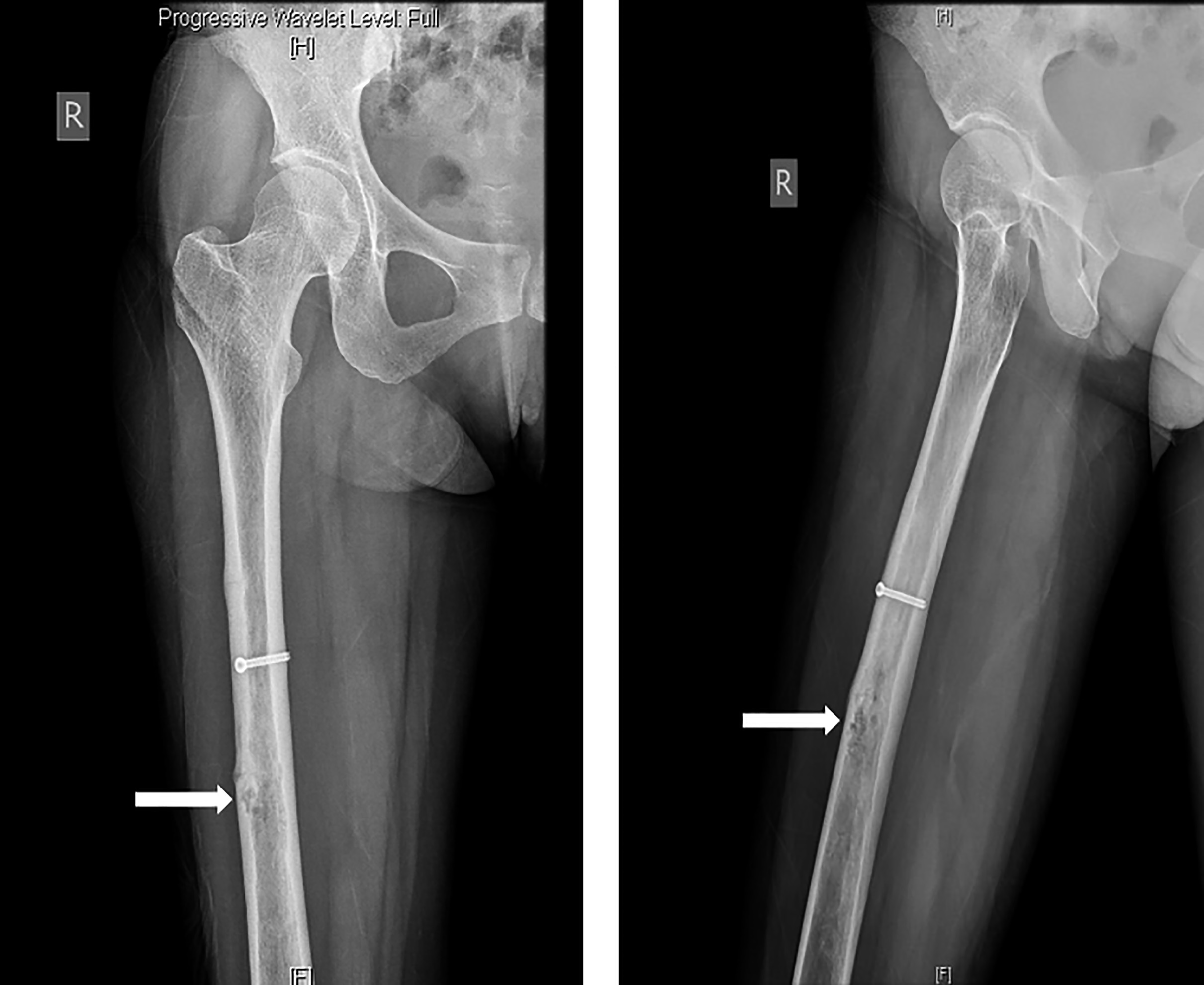
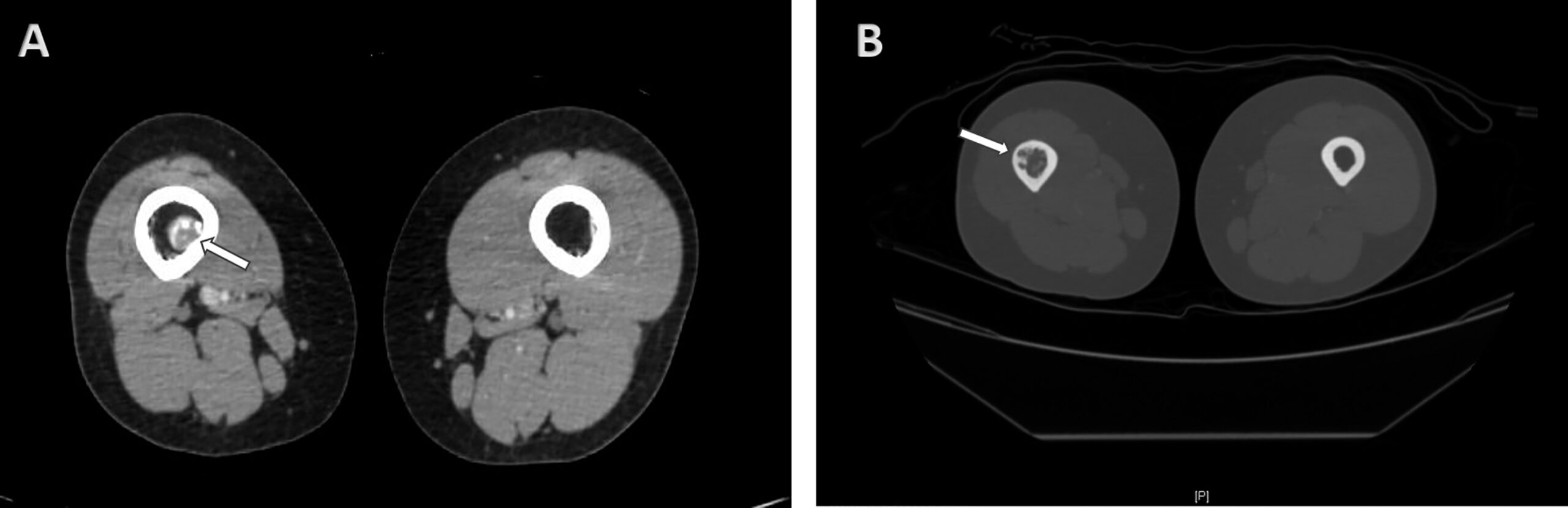
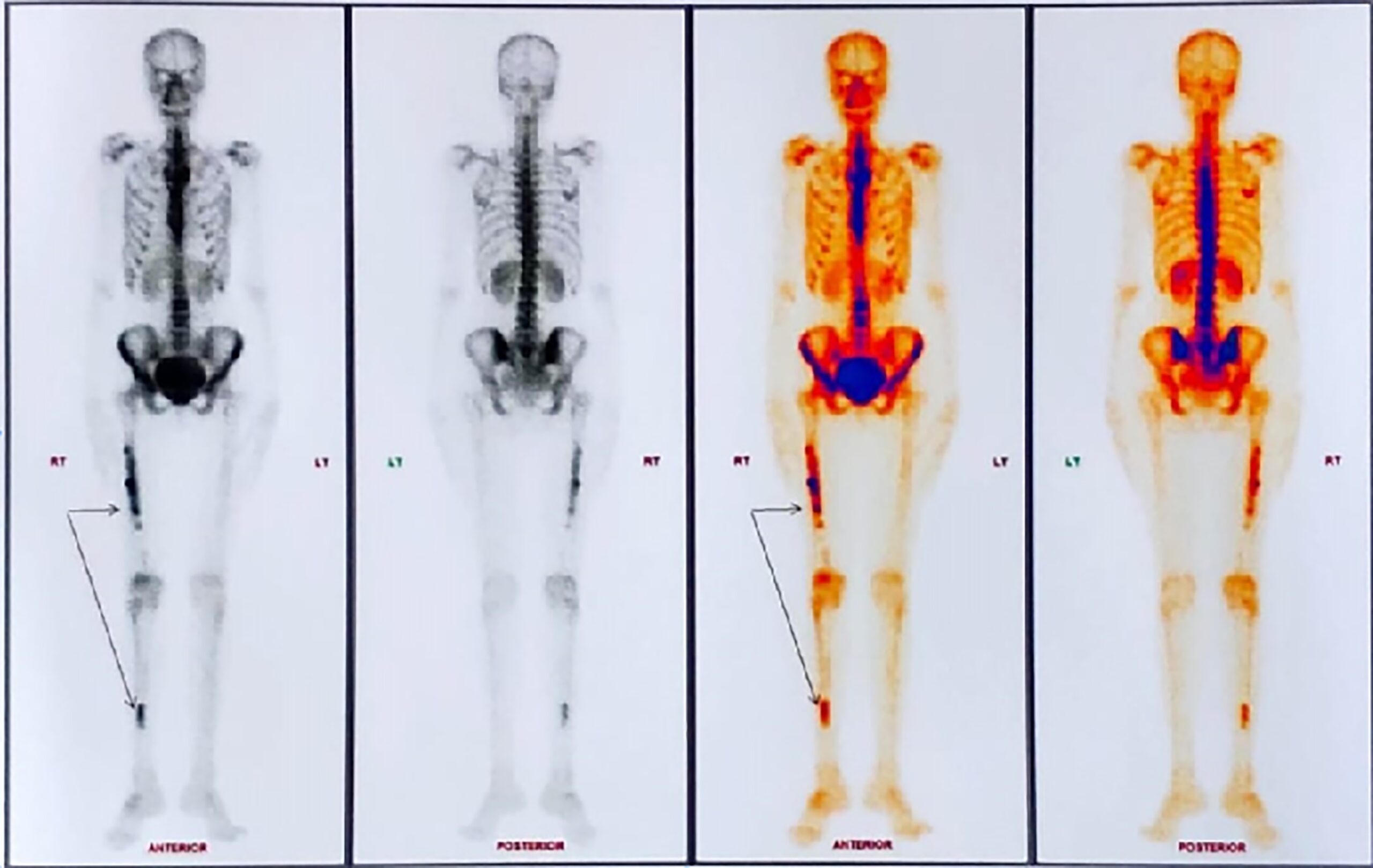

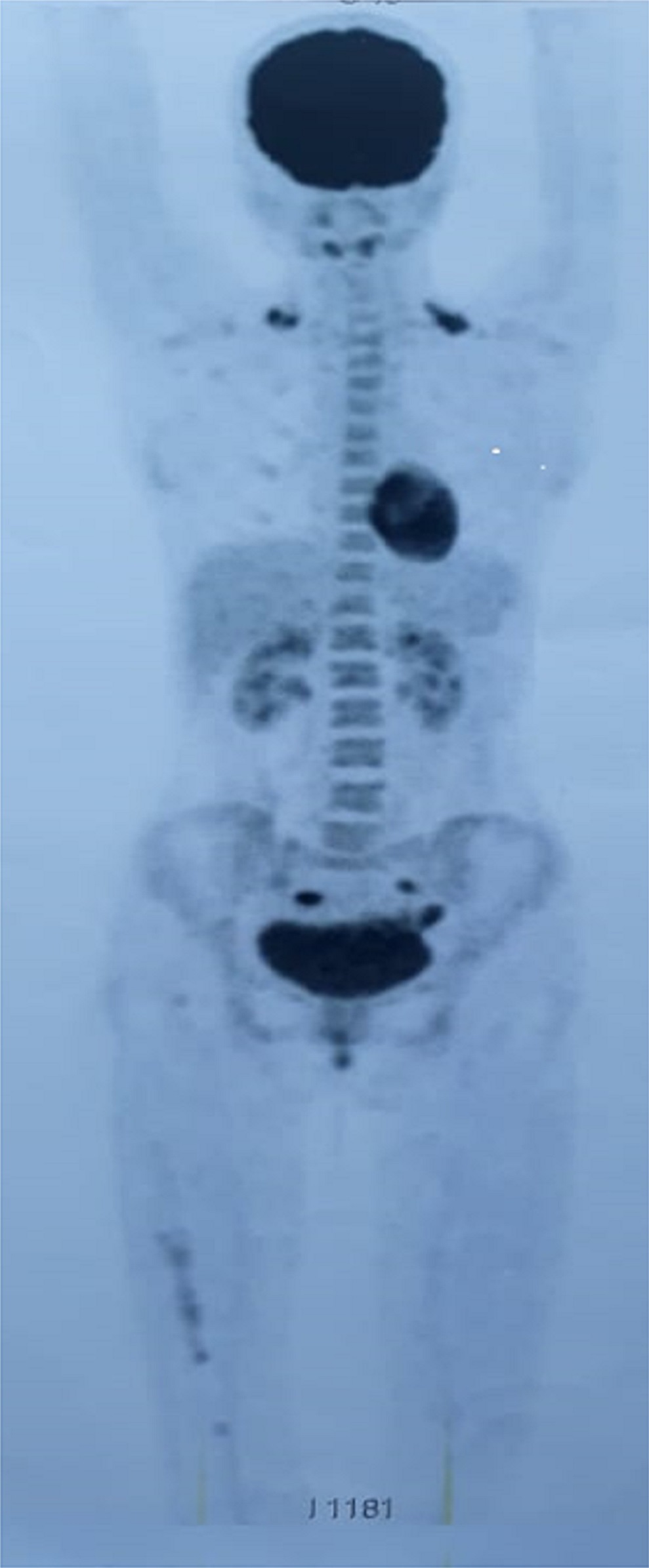
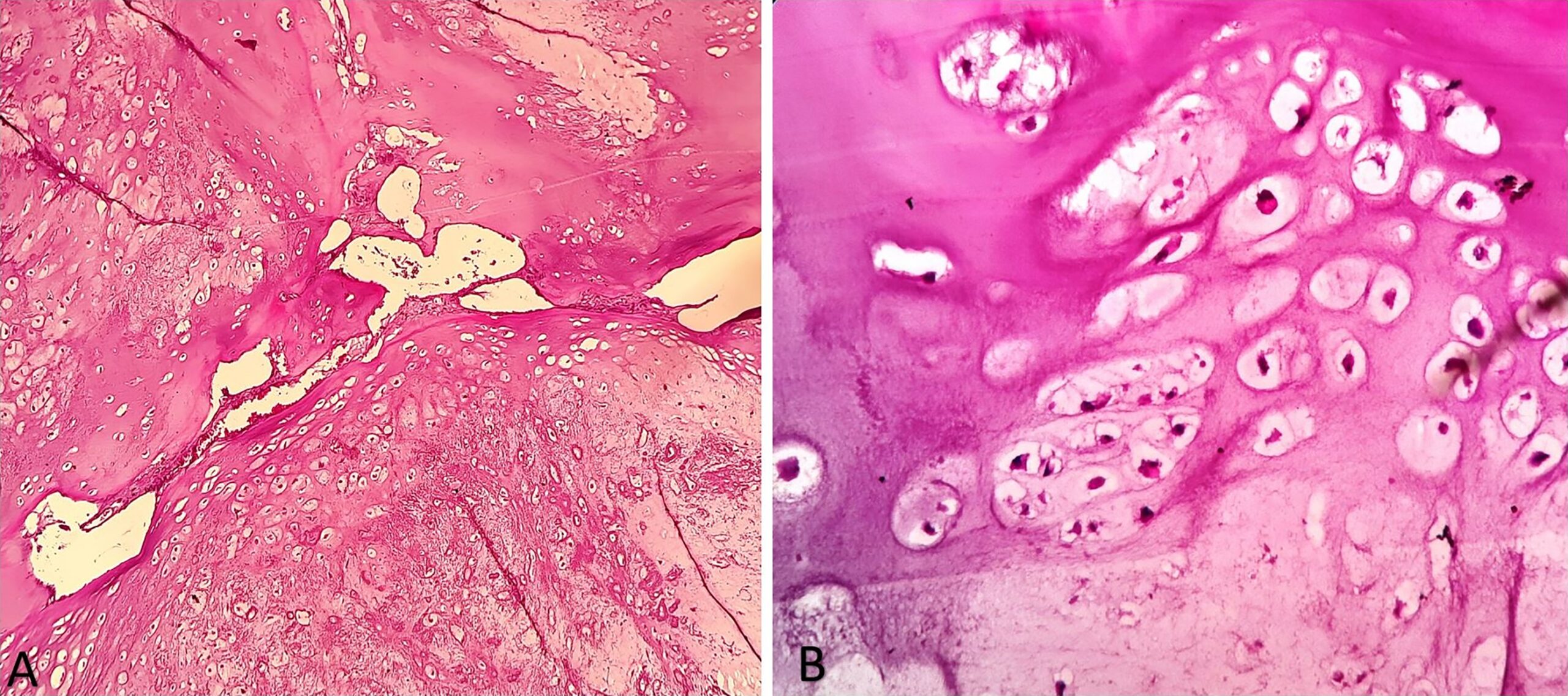
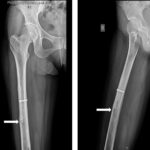 Fig. 1
Fig. 1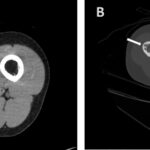 Fig. 2
Fig. 2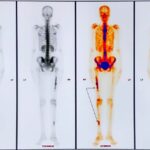 Fig. 3
Fig. 3 Fig. 4
Fig. 4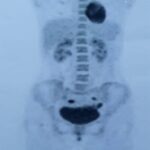 Fig. 5
Fig. 5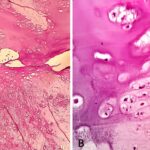 Fig. 6
Fig. 6 Fig. 7
Fig. 7