A 54-year-old man presented at the emergency department with low back pain and a 2-day history of a low-grade fever (maximum at-home measurement, 37.6°C). The pain had begun 1 month previously with an insidious onset. The visual analog scale for pain was 4 of 10 at rest, worsening with activity and resolving at night. His temperature on admission was 37.3°C in the emergency department. He had no alcohol abuse or smoking history, and his medications included atorvastatin and irbesartan.
An oval mass of the lumbar region was obvious during inspection. On palpation, it was rather warm, hard, immobile, and about 6 cm in size and the patient did not experience pain with this mass (Fig. 1). There were no findings from the neurological examination, and a straight leg raise test (Lasègue’s sign) was negative. Radiographs of the lumbar spine were normal. The laboratory results showed a slightly elevated white blood cell count of 11.200/μL with mild eosinophilia (7.2%). The results from a complete metabolic panel were normal, but the C-reactive protein was elevated (3.6, with normal values < 0.5), as was the erythrocyte sedimentation rate (34, with normal values <10). Magnetic resonance imaging (MRI) scans demonstrated a 4.8 × 6.8-cm, thin-walled cyst with no septation at the level of L2-L4, located inside the longissimus thoracis muscle. The lesion extended from the subcutaneous tissue of the lumbar spine to the transversospinalis muscle group, penetrating the posterior layer of the thoracolumbar fascia (Fig. 2).
Computed tomographic (CT) scans were performed on the brain, lungs, and liver. All scans were negative for cysts. Treatment with albendazole (15 mg/kg/day orally) was initiated preoperatively.
One week later, a complete surgical excision of the mass was performed with the patient under general anesthesia. During the procedure, a fully equipped anesthesiology team was on high alert in case of a rupture of the cyst. The mass was removed intact (Fig. 3), with care taken to maintain adequate margins of healthy tissue.
On histopathologic examination, the cyst wall consisted of dense, fibrous tissue with variable numbers of mononuclear cells, multinucleated giant cells, and increased eosinophils. Palisading histiocytes were present mainly on the inner surface. The foci of foreign-body giant cell reaction around eosinophilic, acellular, and refractile (Periodic acid-Schiff+) material were present (Figs. 4, 5, and 6).
The identification of hydatid membranes in the liquid from the cyst was diagnostic of echinococcosis, and the diagnosis was confirmed by histology. The patient was diagnosed with echinococcosis. Treatment with albendazole continued for 1 month postoperatively.
The patient was discharged a week after the surgical procedure. At the 6-month follow-up outpatient consultation, the patient was asymptomatic, did not experience pain, and had full, active range of motion of the spine, and no clinical or laboratory signs of infection were found. At 1 year postoperatively, a new MRI scan of the spine was performed, and the results were negative for cysts. Three years after that, the patient had pain relief with no recurrence.
Proceed to Discussion >>Reference: Raoulis V, Mitrousias V, Malahias MA, Stofas A, Fyllos A, Malizos KN. Primary paraspinal hydatid cyst in a patient presenting with low back pain: a case report. JBJS Case Connect. 2021 Feb 11;11(1):e20.00581.
Primary muscular hydatidosis is a rare manifestation of an Echinococcus granulosus infection, observed in <5% of infected patients. Although humans with this infection usually live in close contact with the 2 hosts, this patient reported that he had not been in proximity with dogs or sheep. The pathogenesis of a primary muscular hydatid cyst in muscle compartments is not clearly known. Some researchers support that that larva is transported across the muscular layer of the gastrointestinal tract into the venous system bypassing the liver, and others have proposed that direct contact of the larva with the wound can be the possible explanation. At the 6-month follow-up, our patient remembered that he had had a pimple-like wound in this area 7 months before the surgical procedure after he had lain naked on the grass, while working as a farmer in the grazing fields, suggesting a means of direct transmission.
It is also exceedingly rare for the cyst to be located paraspinally, as well as being diagnosed before any manifestation of neurological signs and symptoms, as the infection is indolent. Clinical symptoms of a hydatid cyst vary from mass detection to pressure symptoms or, rarely, anaphylactic shock and cyst infection. Inspection of the mass is not always possible and, along with palpation, depends on the depth of the lesion. Radiographs are usually normal, and diagnosis is often missed. Only advanced imaging such as MRI might provide adequate information, requiring high suspicion of the disease, especially for physicians practicing in endemic areas or dealing with immigrants from such areas. Low back pain without fever had already been presented 1 month before the final diagnosis. At that point, the patient had visited the emergency department and he was treated with a recommendation for rest and paracetamol. The red-flag sign that alarmed both the patient and the physicians was the low-grade fever that occurred later. Although very helpful for the early diagnosis of the disease, to the best of our knowledge, this is the first reported case in which fever was present in paraspinal muscular hydatidosis. This diagnosis emphasizes the need for a high suspicion for fever-like symptomatology in common clinical entities, such as low back pain.
Confirmation of the diagnosis can be difficult, as a biopsy is generally not recommended because of severe complications observed if the contents of the cyst are released, causing a possible spread of the localized disease or an anaphylactic shock. Serological tests, such as enzyme-linked immunosorbent assay, can be helpful but expensive, and their sensitivity varies between 60% and 90% in different assays. A collaboration with an infectious disease specialist might be considered mandatory to exclude other sites of infection and establish medical treatment.
Previous case series have shown that hydatid cysts within paraspinal musculature tend to invade the spinal canal through an intervertebral foramen within 12 to 36 months. The time frame is short and in sharp contrast with hydatid cysts in other locations, for example, intraosseous vertebral cysts, which invade very slowly. That is why high suspicion, early diagnosis, and direct surgical removal might be crucial.
Treatment with puncture, aspiration, injection, and reaspiration technique has been reported. Although there is evidence to support its successful use in uncomplicated hepatic cysts, this treatment still raises concerns with regard to complications, such as iatrogenic spreading of the infection. By contrast, complete surgical resection is nowadays considered as the gold-standard treatment of muscle hydatidosis. Oncologic principles with wide excision of the hydatid cyst and clear margins have been correlated with decreased rates of recurrence.
In summary, primary paraspinal hydatidosis is rare, and physicians should be aware of it when dealing with patients with low back pain and red-flag symptoms, especially in rural regions or areas where populations live in proximity to host animals. Wide excision with clear margins of an intact cyst is the definitive treatment, accompanied by anthelmintic treatment and, in this case, with albendazole both preoperatively and postoperatively.
Reference: Raoulis V, Mitrousias V, Malahias MA, Stofas A, Fyllos A, Malizos KN. Primary paraspinal hydatid cyst in a patient presenting with low back pain: a case report. JBJS Case Connect. 2021 Feb 11;11(1):e20.00581.
What is the diagnosis?
Intramuscular cysticercosis
Schistosomiasis
Echinococcosis
Coccidioidomycosis
Gossypiboma

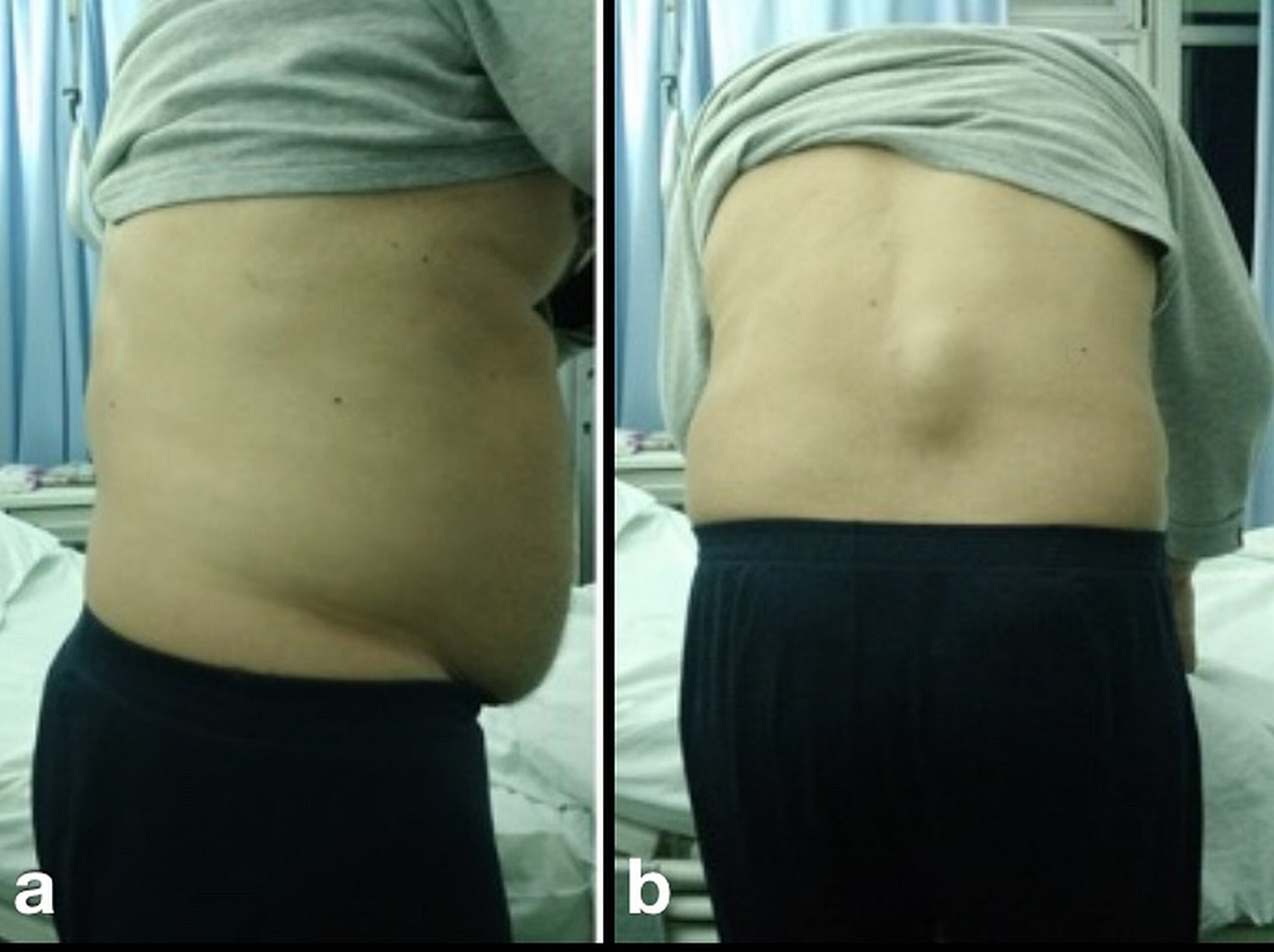
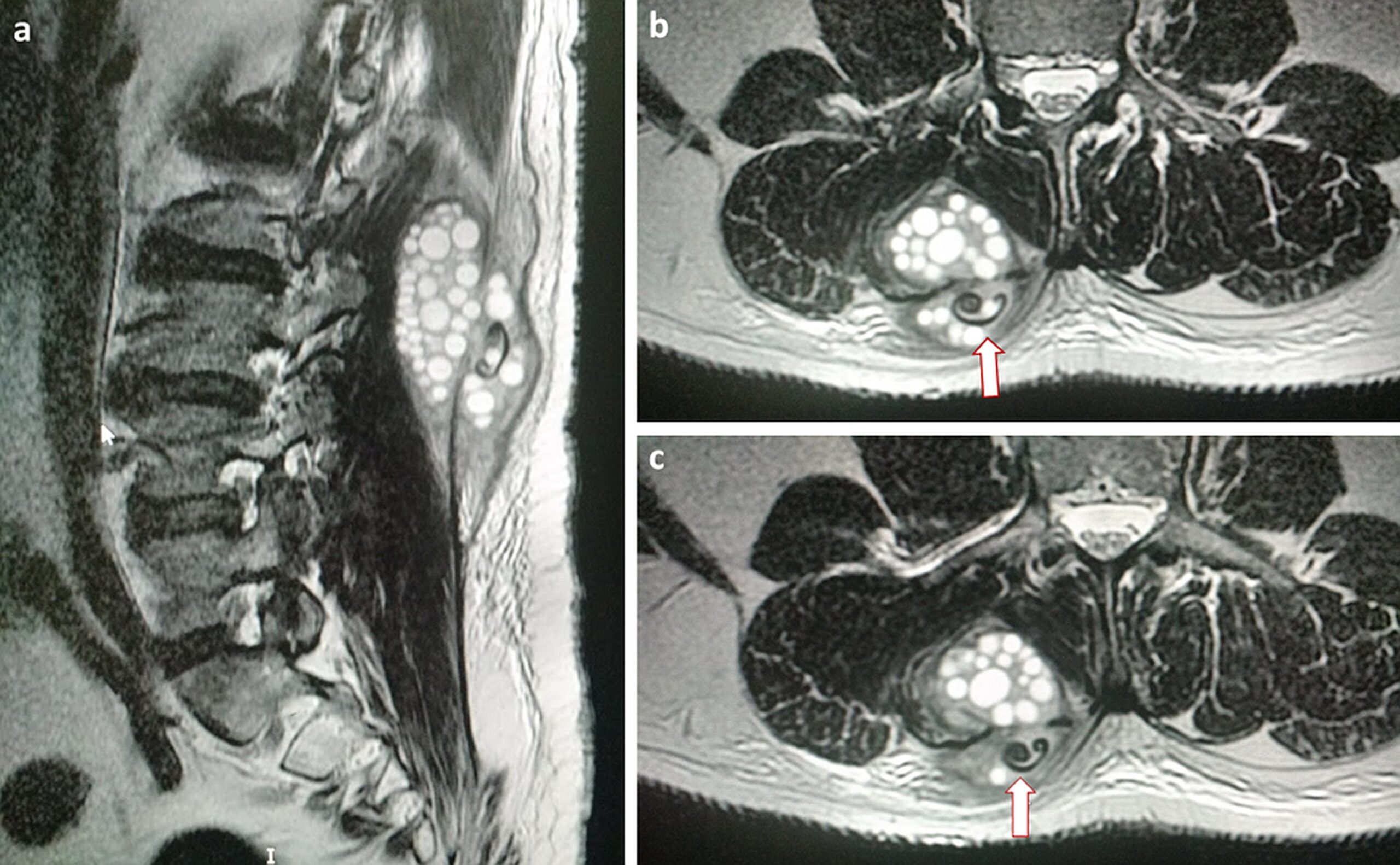
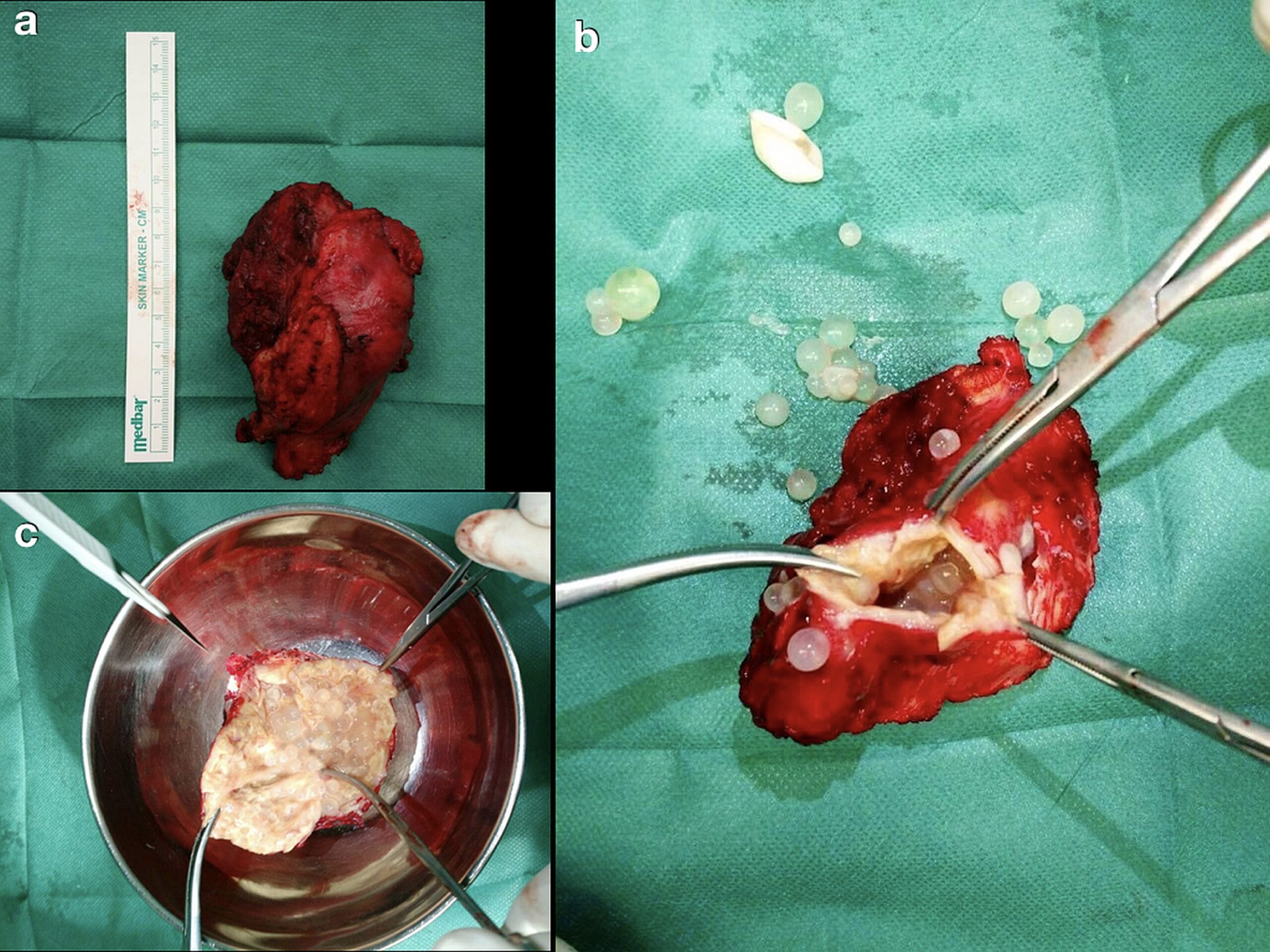
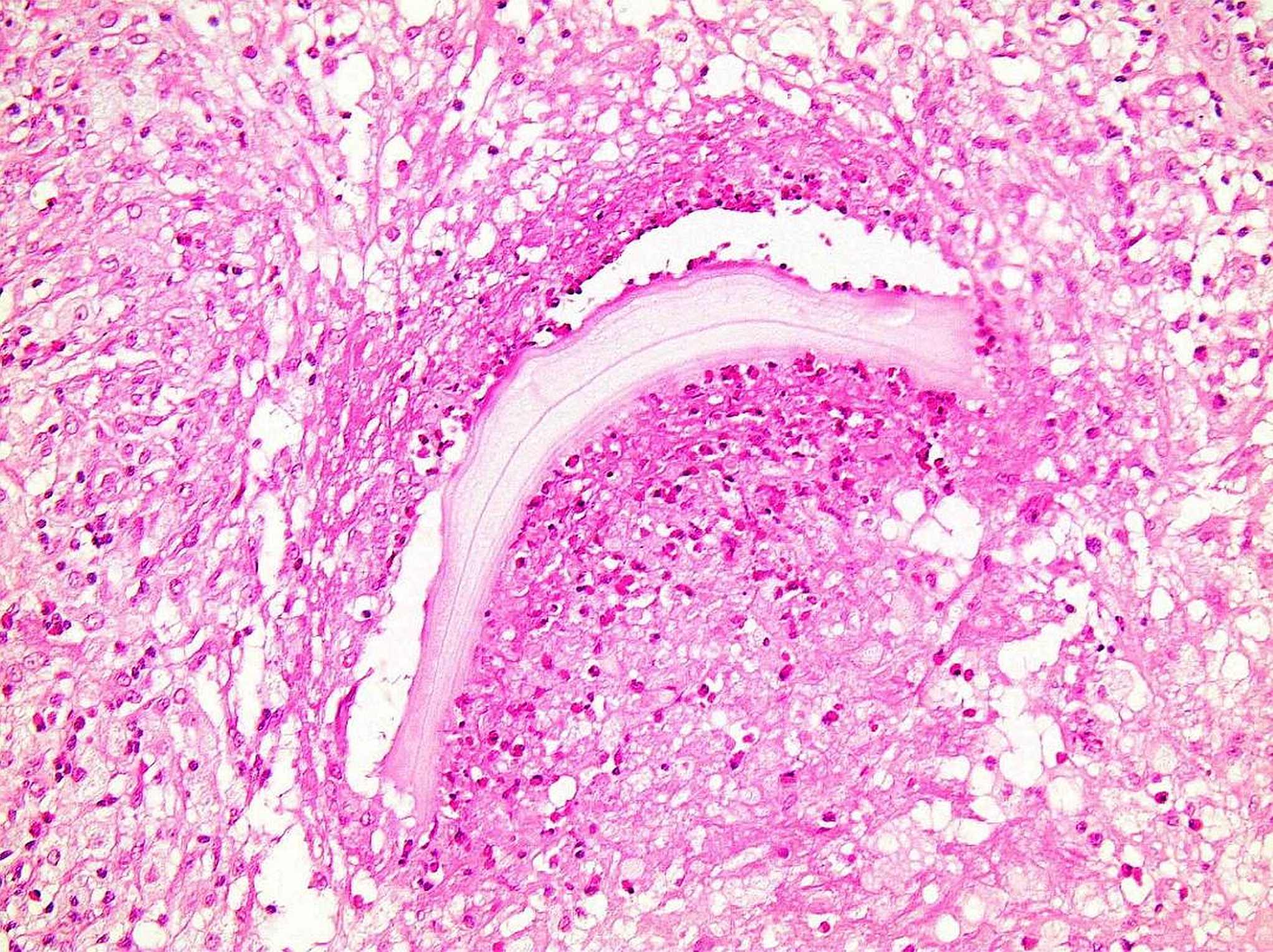
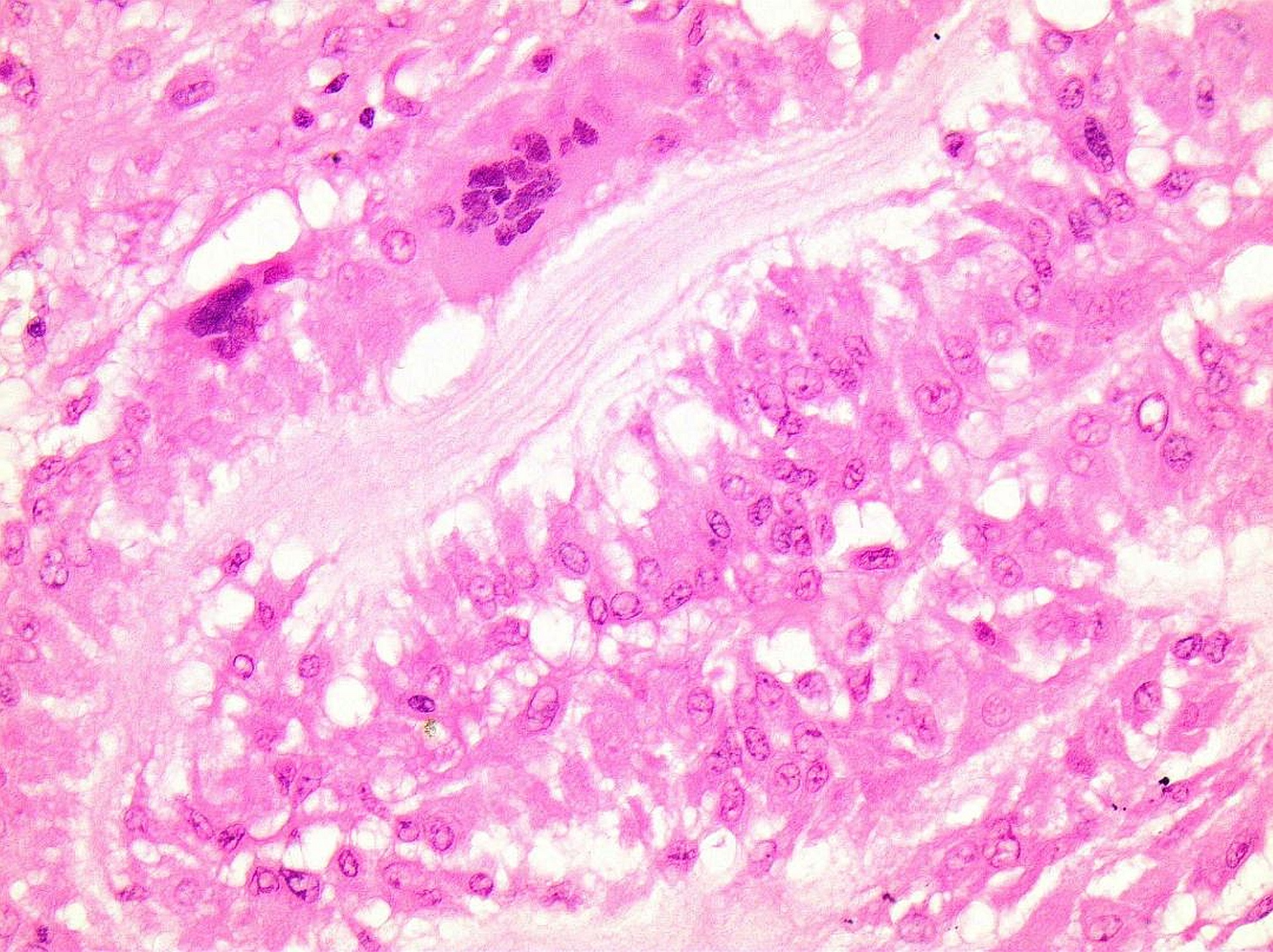
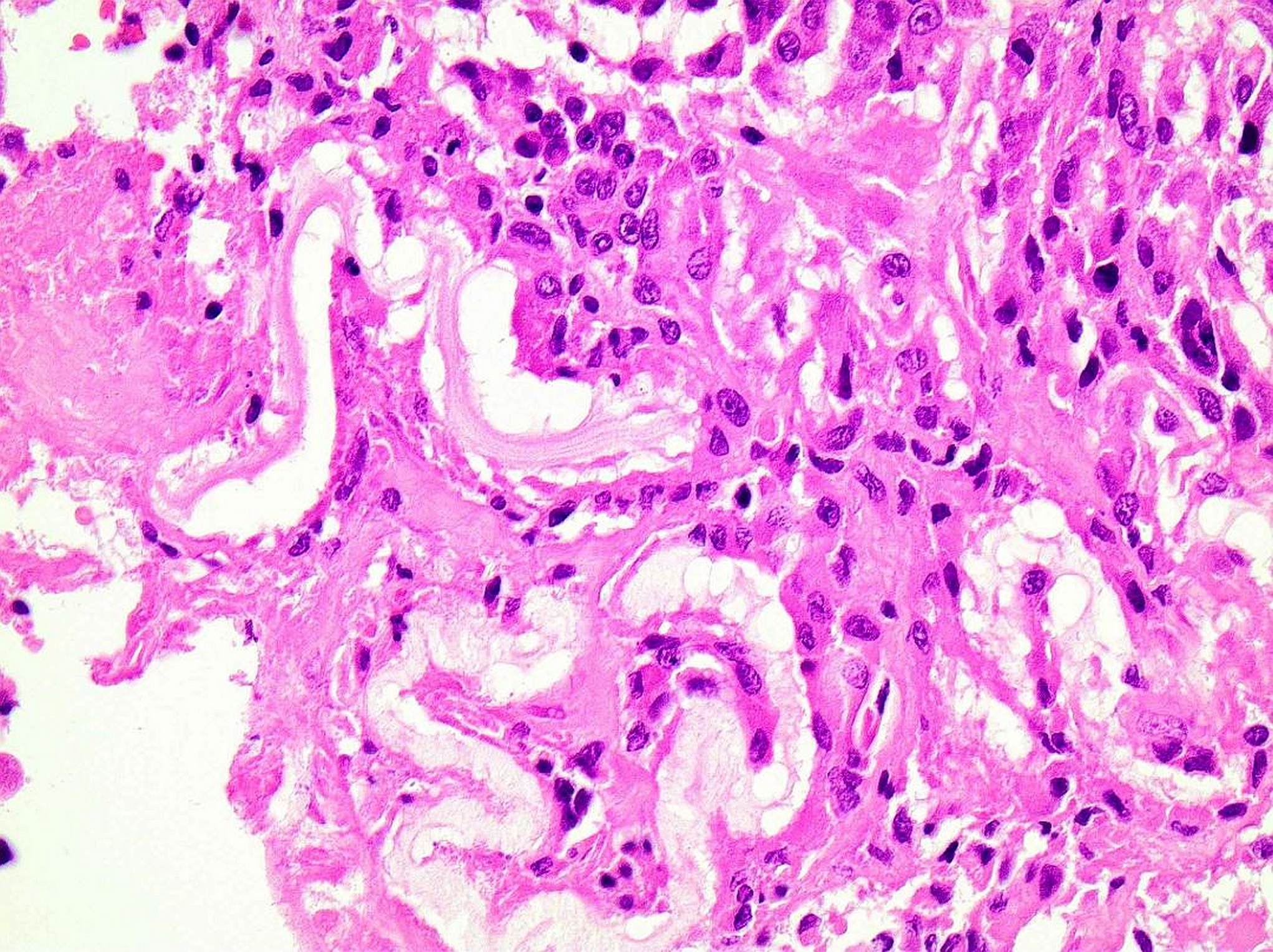
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3![Fig. 4 Fig. 4 Histological image revealing refractile material and dense inflammatory infiltrate (hematoxylin and eosin [H&E] stain; original magnification, ×100).](https://quiz.jbjs.org/wp-content/uploads/2022/05/iqjun-22-11_fig4-150x150.jpeg) Fig. 4
Fig. 4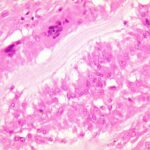 Fig. 5
Fig. 5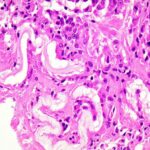 Fig. 6
Fig. 6