A 4-year-old boy presented with right ankle pain, erythema, edema, and limping, which started 1 month previously. These symptoms started after he sprained his ankle and injured it against a wood splinter. After treatment with casting for 1 week, symptoms did not decrease and blood tests showed a white blood cell (WBC) count of 18,910 cells/μL, a C-reactive protein (CRP) of 20.2 mg/L, and an erythrocyte sedimentation rate (ESR) of 30 mm/h. Empiric antibiotics were started and were given for 15 days. The patient was directed to our clinic at this point. He was limping and had right ankle pain and localized swelling and rubor. Blood tests showed a WBC count of 15,620 cells/μL, CRP of 61.18 mg/L, and ESR of 40 mm/h, and radiographic imaging demonstrated distal metadiaphyseal erosion (Fig. 1). Previously performed magnetic resonance imaging (MRI) with intravenous contrast agents presented heterogeneous contrast in the distal metadiaphyseal region of the fibula (Fig. 2).
Under general anesthesia, the distal metadiaphyseal region of the fibula was reached using a 4-cm anterior incision. The bone was drilled and emptied using a curette. Bacteria that grew on culture are shown in Figure 3, and biopsy findings are shown in Figures 4-A and 4-B.
Small colonies of gram-positive, blunt, or club-shaped bacilli grew on culture (Fig. 3), and the tissue showed acute and chronic inflammation without granulomas (Figs. 4-A and 4-B). Therefore, the diagnosis was osteomyelitis caused by gram-positive bacteria. The bacteria were subsequently characterized by fermentation and other tests as Corynebacterium. The patient was then referred to pediatric infectious diseases and vancomycin with cefazolin was given intravenously. An analytical profile index (API) test was performed and the Corynebacterium was subtyped as C. striatum.
The patient was followed for 6 weeks at the hospital because he was given intravenous antibiotics. All clinical symptoms faded, and blood tests showed CRP of 0.5 mg/L, ESR of 11 mm/h, and WBC count of 12,200 cell/μL at his 6-month clinic visit. Radiographs (Fig. 5) and MRI (Fig. 6) revealed recession in pathologic signs.
There were no complications, wound infections, or joint limitations at the follow-up visits. At the last follow-up, at 2 years postoperatively, radiographs were normal (Fig. 7).
Proceed to Discussion >>Reference: Bayram S, Bilgili F, Anarat FB, Saka E. Subacute osteomyelitis of the fibula due to Corynebacterium striatum in an immunocompetent child. A case report. JBJS Case Connect. 2019 May;9(2):e0220.
Osteomyelitis in children is primarily in the acute form and hematogenous in origin, although cases secondary to penetrating trauma, surgery, or infection in a contiguous site have also been reported. Because the signs are weak, clinical suspicion and radiologic imaging are needed, which takes approximately 63 days to make a proper diagnosis. In our case, diagnoses were made around 58 days after the symptoms began.
Staphylococcus aureus is the most common agent responsible for subacute osteomyelitis. Other organisms such as Staphylococcus epidermidis, Streptococcus species, Pseudomonas, Haemophilus influenzae, and coagulase-negative Staphylococcus have also been reported. Corynebacterium species has also been reported, albeit infrequently. C. striatum is a gram-positive bacillus microorganism isolated from mucus membranes and skin. The literature has reported C. striatum as being related mostly to opportunistic infections, especially as the cause of nosocomial infections such as respiratory tract infections, ulcer, keratitis, meningitides, endocarditis, peritonitis, osteomyelitis, urinary tract infections, and catheter infections, as well as through breaks in the skin.
Under light microscopy, gram-positive bacilli Corynebacterium species may be seen arranged in palisades. To distinguish species, metabolic profiling is the most common method. Metabolic profiling such as glucose, sucrose, catalase activity, and fatty acid analysis shows similarity between C. striatum, Corynebacterium minutissimum, and Corynebacterium macginleyi species. These tests include N-acetylglucosamine assimilation, phenyl acetate assimilation, and lipophilia. When using metabolic profiling, phenotypic overlap limits analysis of fatty acids to discriminate C. striatum from other species. The API Coryne test is more reliable especially differentiating C. striatum and Corynebacterium amycolatum. Corynebacterium is best identified with phenotypic methods and complete 16S Ribosomal ribonucleic acid (rRNA) gene sequencing. C. striatum has been reported to develop resistance against levofloxacin, erythromycin, imipenem, penicillin, cephalosporin, clindamycin, and linezolid. No resistance is reported for vancomycin and it must be included in treatment.
Another concern for this disease is that the radiologic signs can easily be confused with bone tumors. MRI has 88% to 100% sensitivity and 75% to 100% specificity. However, Riise et al. found that only 69% of patients with subacute osteomyelitis had positive magnetic resonance signs. For this reason, biopsy and culture are needed. The differential diagnosis includes tuberculosis, osteoid osteoma, osteosarcoma, chondroblastoma, osteogenic sarcoma, Ewing sarcoma, fibrosarcoma, and eosinophilic granuloma.
The recommended treatment of subacute osteomyelitis is curettage and lesion excision and 6 weeks of antibiotic therapy. Surgical treatment is controversial but may be needed for diagnosis and proper treatment. In pediatric patients, when the disease is at epiphyseal or metaphyseal sites, antibiotic treatment should be the first choice.
To our knowledge, this is the first case report of subacute osteomyelitis in a child caused by C. striatum in an immunocompetent patient without risk factors, probably secondary to a wood splinter injury without any visible skin wounds.
Clinical signs, laboratory results, and imaging studies in themselves may not distinguish subacute osteomyelitis from benign or malignant bone tumors. Tissue culture specimens should routinely be taken and tissue should be examined in pathology. Carefully chosen antibiotics are usually needed for recovery.
Reference: Bayram S, Bilgili F, Anarat FB, Saka E. Subacute osteomyelitis of the fibula due to Corynebacterium striatum in an immunocompetent child. A case report. JBJS Case Connect. 2019 May;9(2):e0220.
What is the diagnosis?
Bacteria and granulomatous inflammation consistent with mycobacterial infection
Filamentous bacteria and acute inflammation consistent with Actinomyces infection
Gram-negative rods and inflammation consistent with Salmonella osteomyelitis
Osteomyelitis caused by gram-positive bacteria
Gram-negative bacilli and acute inflammation consistent with Pseudomonas osteomyelitis

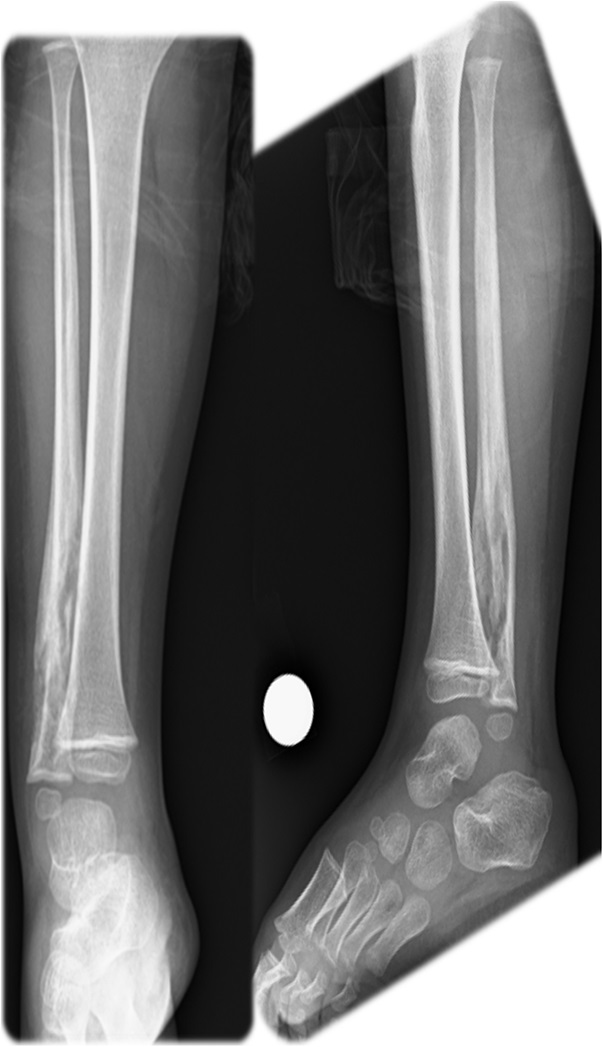
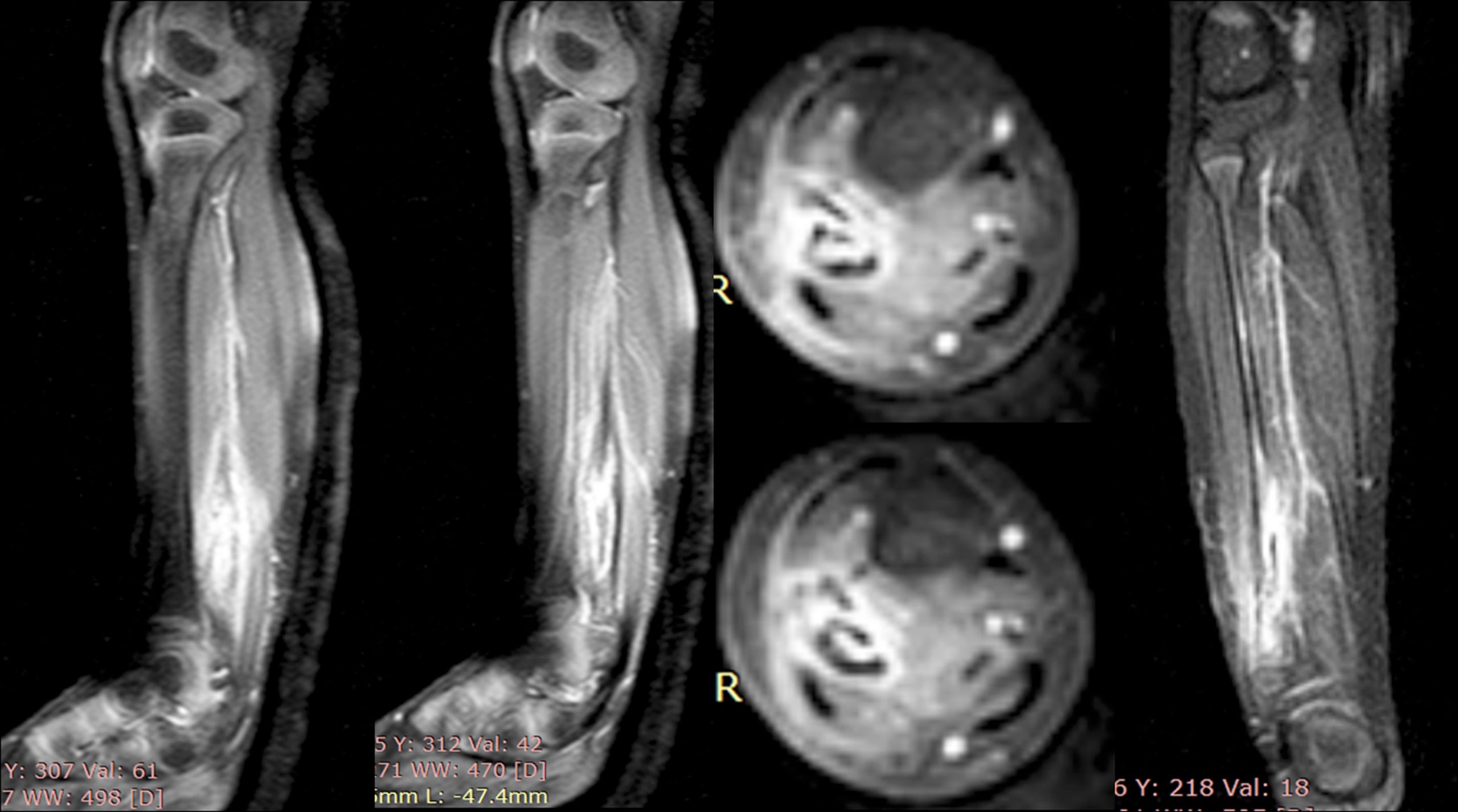

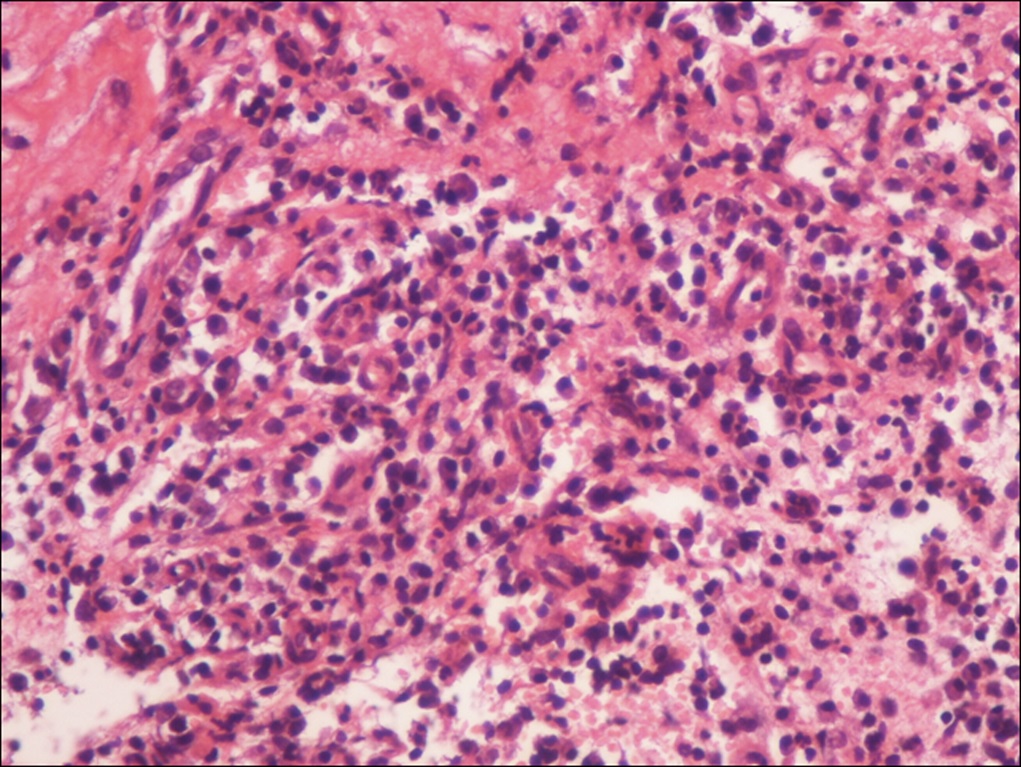
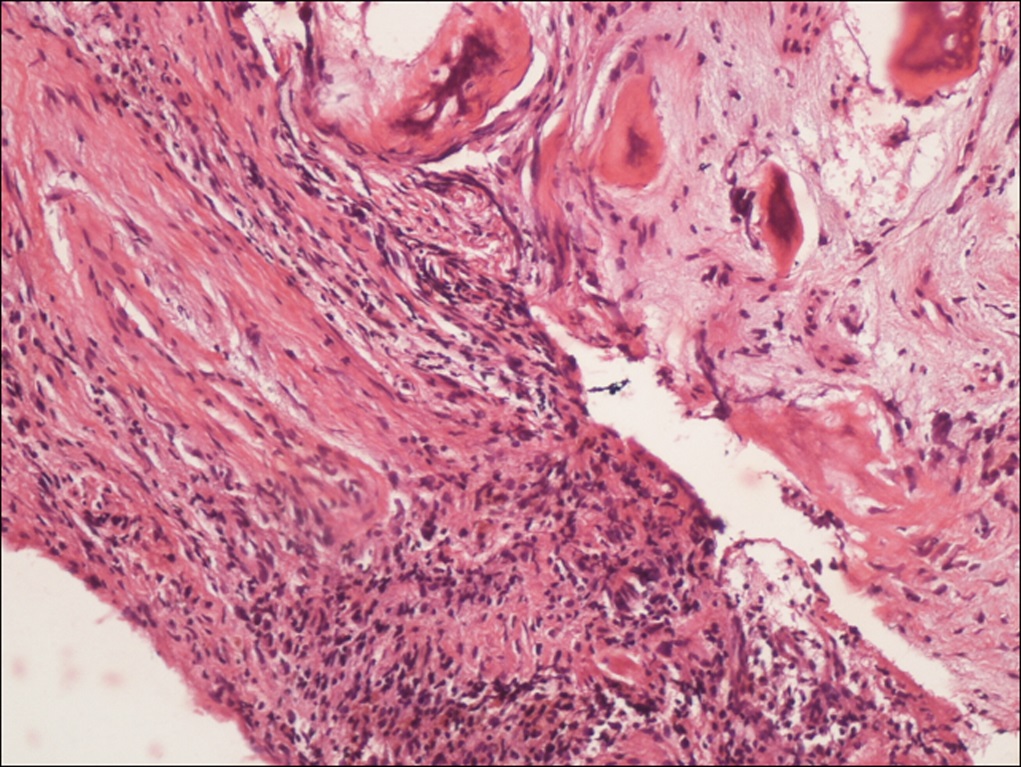
 Fig. 1
Fig. 1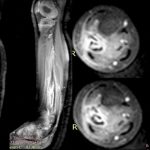 Fig. 2
Fig. 2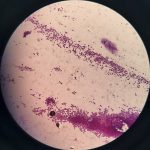 Fig. 3
Fig. 3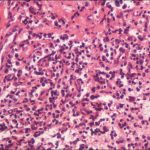 Fig. 4-A
Fig. 4-A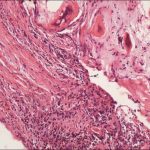 Fig. 4-B
Fig. 4-B Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7

