A 4-Month-Old Boy with Gradual Swelling of the Arm
November 2, 2022
A 4-month-old boy presented with swelling of the right forearm that he had experienced for 2 months. His parents had previously consulted another hospital 1 month prior where fine-needle aspiration cytology showed only inflammatory cells. The child was brought to our hospital as the swelling continued to progress in size. The child was afebrile, and there were no other swellings.
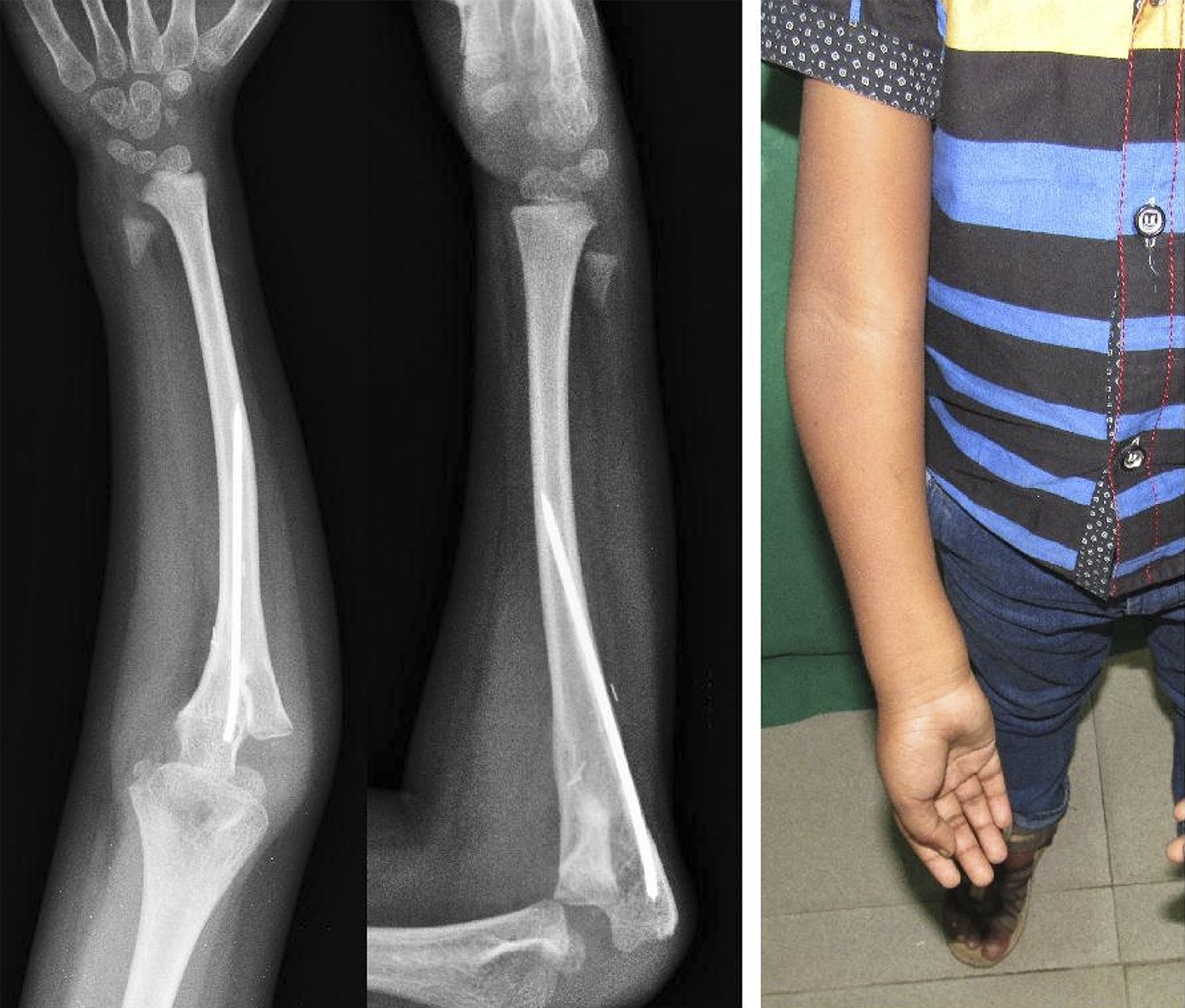
Clinical examination showed diffuse, hard, immobile, and nontender swelling over the proximal aspect of the dorsal surface of the forearm. The swelling was 6 cm by 3 cm in size over the ulna (Fig. 1). Movements of the elbow and wrist and pronation and supination were normal. Radiographs of the forearm showed the lytic area in the ulna surrounded by sclerotic bone (Fig. 2). Blood examination showed normal white blood cell counts, erythrocyte sedimentation rate, C-reactive protein, and alkaline phosphatase.
Magnetic resonance imaging (MRI) of the forearm showed altered marrow signal noted in the middle third to the proximal third diaphysis of the ulna with an adjacent, fairly defined, soft-tissue mass at the medial aspect. The medial cortex of the ulna was eroded with areas of periosteal new bone formation.
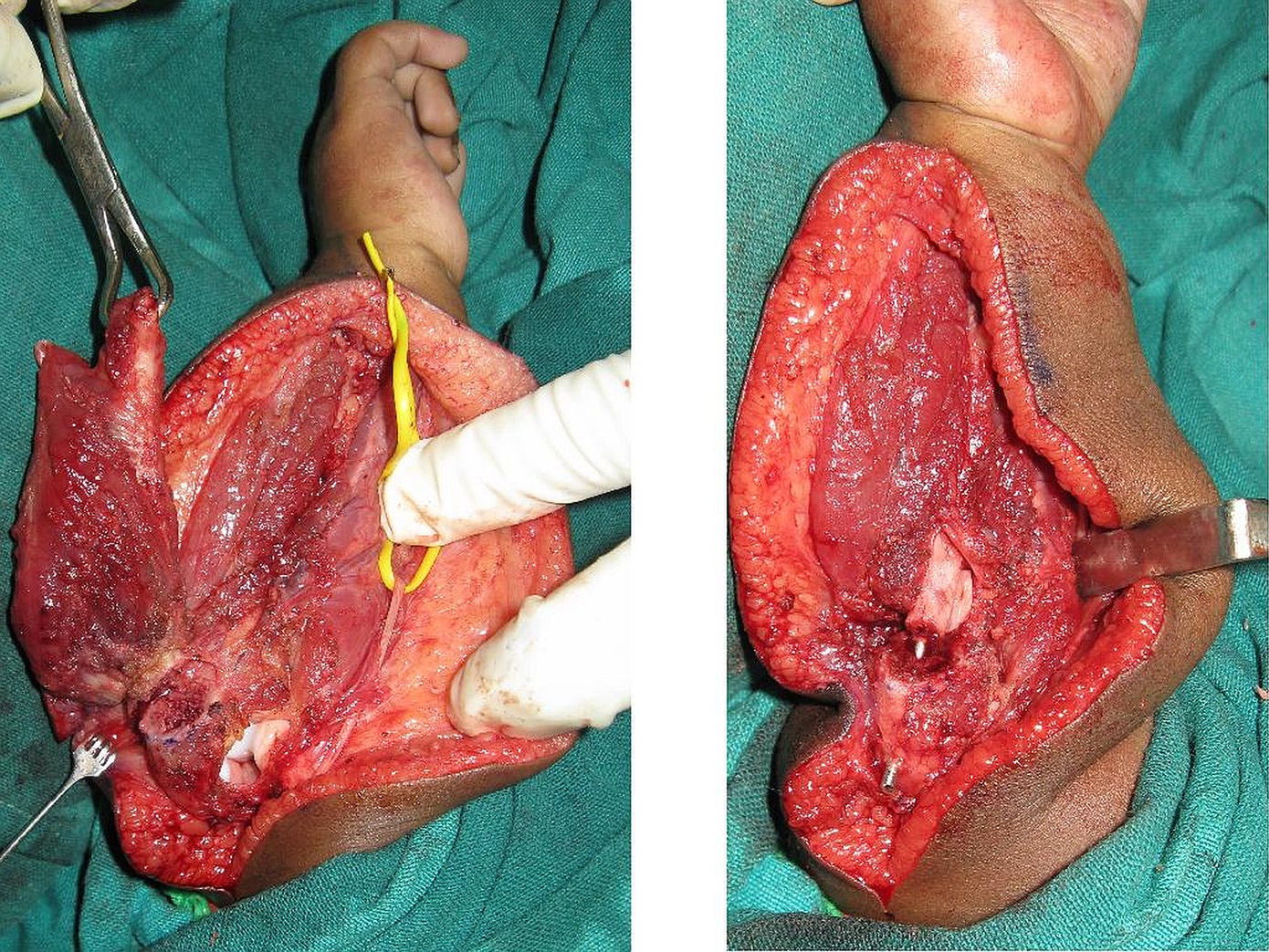
An open biopsy was performed, and, on exposure, the ulnar black tissue was seen under the periosteum and was eroding the ulna (Fig. 3). The tissue was removed, and histopathology showed fibrous tissue containing irregular clusters of cells in a fibrillary matrix and clusters of cells containing pigment granules (Figs. 4, 5, and 6).
The patient was diagnosed as having a melanotic neuroectodermal tumor of infancy.
Upon knowing the diagnosis, the 24-hour urinary vanillylmandelic acid was checked, and it was within normal limits. A wide excision of the tumor was undertaken; this excision included a resection of most of the ulna, leaving only 1.5 cm of the proximal part of the ulna and the distal 2-cm part of the ulna. The radius was osteotomized at the proximal third after isolation of the posterior interosseous nerve, and the distal segment of the radius was joined to the olecranon to create a one-bone forearm (radioulnar synostosis) and was stabilized with an intramedullary nail of the appropriate diameter introduced from the olecranon (Fig. 7). A Plaster of Paris posterior above-the-elbow slab was given for a period of 2 weeks followed by an above-the-elbow cast for 6 weeks. The postresection specimen was 3.5 cm long, 1 cm at its broad end, and 0.4 cm at its narrow end. Microscopic examination showed infiltration of the tumor into the medullary cavity and skeletal muscle with clear margins.
After 8 weeks, the osteotomy and union of the radius with the ulna were seen to be progressing. The patient was under regular follow-up with radiographs until he was 6 years of age. There was no tumor recurrence clinically or radiologically (Fig. 8), and the child had a functional upper limb with a full range of wrist and elbow movements, full supination, and pronation until he was midprone.
Proceed to Discussion >>Reference: Kovoor CC, Jayakumar R, Manjunath S. Melanotic neuroectodermal tumor of infancy in the ulna of an infant: a very rare tumor: a case report. JBJS Case Connect. 2021 Mar 8;11(1):e20.00239.
The melanotic neuroectodermal tumor is a rare tumor with a predisposition for the head and neck region, especially in the maxilla. Most of the literature comprises case reports with occasionally larger series. The tumor is known to be still rarer in the extremities.
To the best of our knowledge, this is the first report of a melanotic neuroectodermal tumor of infancy that developed in the ulna. It is important to identify this tumor because the treatment and clinical outcome are different from those for other tumors in the extremities at this age, mainly metastatic neuroblastoma, rhabdomyosarcoma, Ewing sarcoma, peripheral primitive neuroectodermal tumor, desmoplastic round cell tumor, malignant melanoma, and lymphoma. The age of presentation, characteristic histopathological appearance, and immune histochemical studies distinguish the melanotic neuroectodermal tumor of infancy from others.
In one of the first cases in the extremities, the tumor was removed from the subcutaneous tissue of the deltoid; in addition to excision, a course of radiotherapy was given for 10 days. Ma et al. described another case in the soft tissue of the forearm, which was treated by excision alone with no other adjuvant treatment but with a short period of follow-up.
Based on the existing case reports, the recommended treatment of a melanotic neuroectodermal tumor of infancy in the appendicular skeleton is wide excision. All patients reported so far had no complications. The evidence for use of radiotherapy in this condition has been limited. Similarly, there has been a lack of evidence for chemotherapy either preoperatively or postoperatively, and fatal cardiac side effects to chemotherapy have been reported.
The presence of elevated urinary vanillylmandelic acid suggested that the tumor had a neural crest origin and was not diagnostic. Elevated and normal values have been reported in cases of melanotic neuroectodermal tumors of infancy both in the craniofacial region and in other regions.
The gross appearance of a melanotic neuroectodermal tumor of infancy typically has a grayish cut surface with areas of black indicating melanin content. Occasionally, the black areas may not be seen, and melanin may be seen only on microscopy with appropriate staining. The microscopic appearance reveals round to polygonal cells in clusters, indistinguishable from other round cell tumors of infancy. The diagnostic feature is of another cell population of epithelioid cells with melanin pigment. Immunohistochemical studies have shown strong positivity for cytokeratin CK17 and CK19 and MIC2/CD99 and a focal positivity for synaptophysin and HMB-45 within the tumor cells. After exhaustive genomic, transcriptomic, epigenetic, and pathological characterization studies of a primary fibular tumor in a 2-month-old female infant and a derived cell line, Barnes et al. identified germline mutation of CDKN2A and novel RPLP1-C19MC fusion. In their series, Gomes et al. found that some melanotic neuroectodermal tumors of infancy may harbor the BRAFV600E mutation, thereby making them amenable to treatment with small molecule drugs targeting BRAF or MEK kinases, providing the first insights to their personalized treatment. It may be of notable importance in recurrent cases and in cases not amenable to wide resection. Neven et al. proposed a treatment protocol for recurrent melanotic neuroectodermal tumors of infancy with surgery and adjuvant chemotherapy as the tumor showed a loss of heterozygosity of chromosome 1p and a gain of chromosome 7q analog to neuroblastomas. We did not perform immunohistochemical studies or next-generation sequencing panel in our case, and we did not have a recurrence in the 6-year follow-up.
The melanotic neuroectodermal tumor of infancy is an unusual tumor of neural crest origin occurring mostly in the craniofacial region. Very rarely, it can occur in the bone and soft tissues of the extremities, and this is the first case reported to occur in the ulna. Radiologically, round cell tumors and osteomyelitis were possible differential diagnoses. Microscopic characteristics are the key to diagnosis.
Awareness about the condition is important for the diagnosis and treatment, particularly considering the differential diagnoses, which are more aggressive and have a poorer prognosis.
Reference: Kovoor CC, Jayakumar R, Manjunath S. Melanotic neuroectodermal tumor of infancy in the ulna of an infant: a very rare tumor: a case report. JBJS Case Connect. 2021 Mar 8;11(1):e20.00239.
What is the diagnosis?
Tenosynovial giant cell tumor, diffuse type (pigmented villonodular synovitis)
Ochronosis
Malignant peripheral nerve sheath tumor with heterologous elements (triton tumor)
Melanotic neuroectodermal tumor of infancy
Melanotic schwannoma



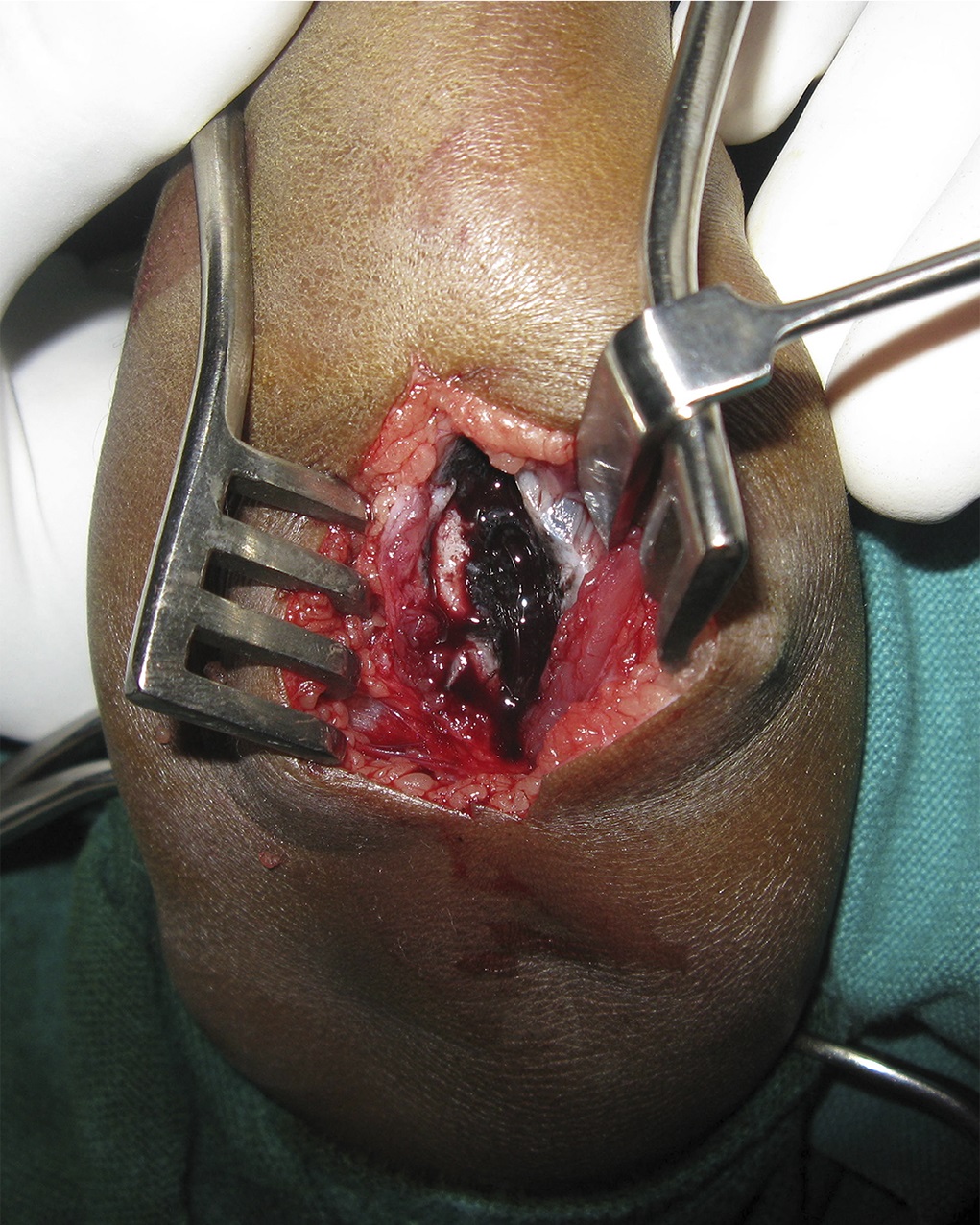
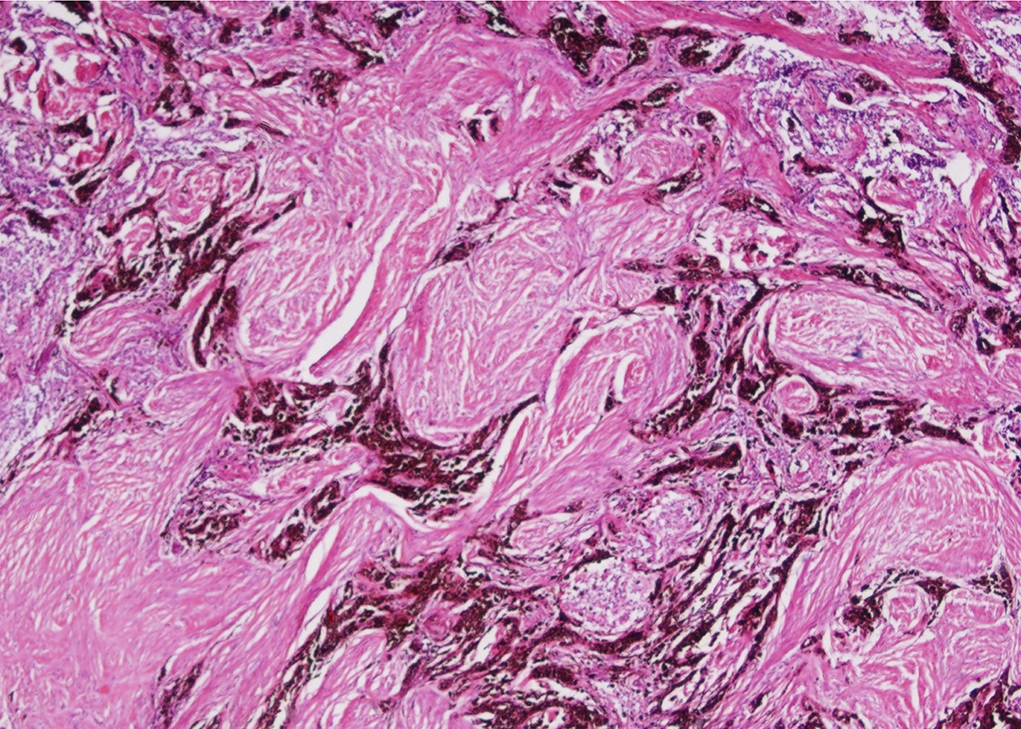
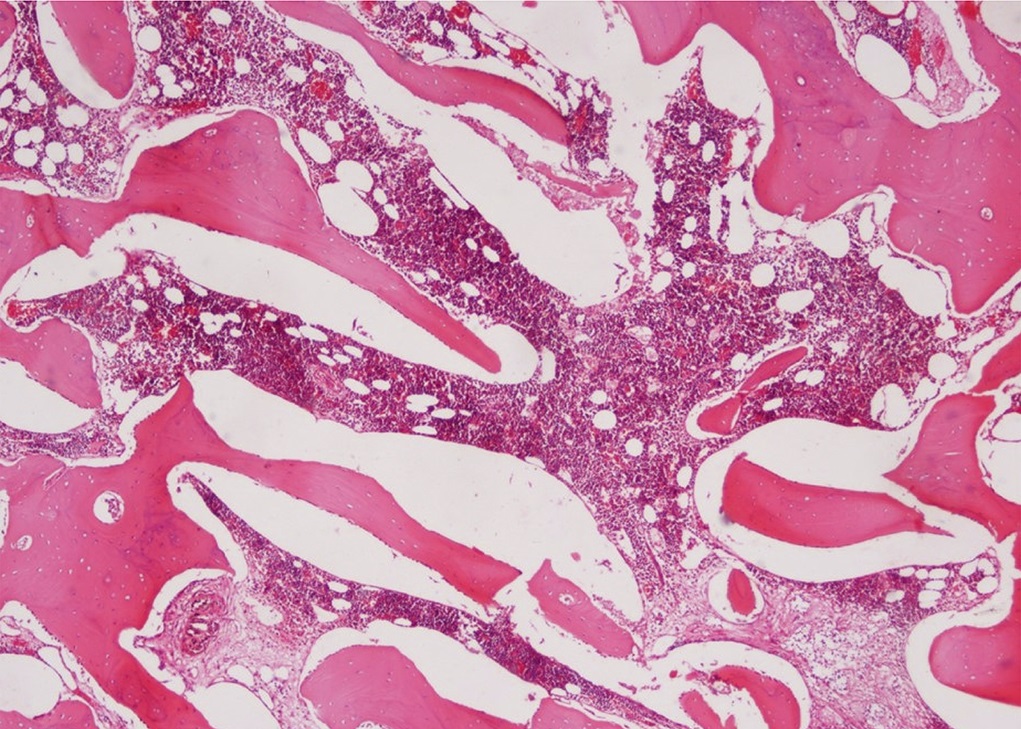
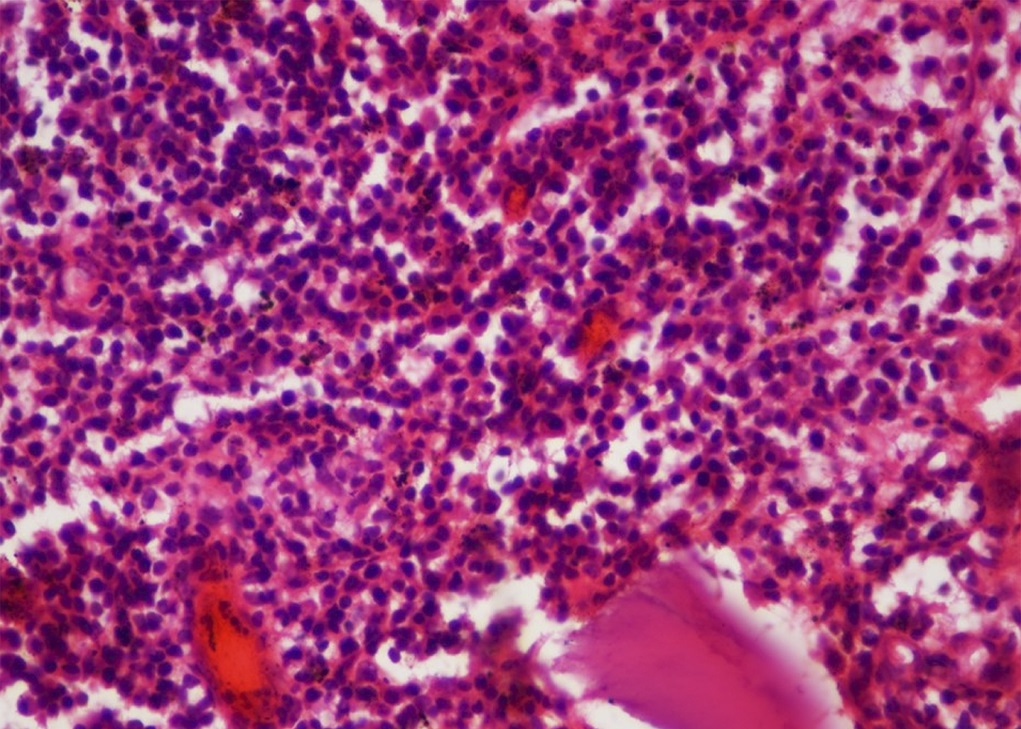
 Fig. 1
Fig. 1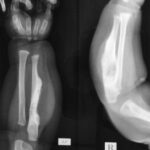 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4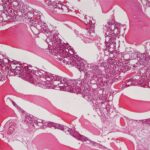 Fig. 5
Fig. 5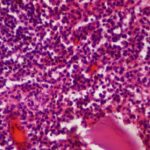 Fig. 6
Fig. 6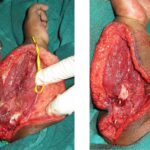 Fig. 7
Fig. 7 Fig. 8
Fig. 8