A 53-year-old, right-hand–dominant man presented with pain over the volar aspect of the middle phalanx of the left index finger; he had experienced this pain for the past 2 years. He also reported sensitivity to cool temperature and exquisite tenderness to pressure at the same location. His history was notable for a fishhook injury to the left index radial digital nerve at the level of the proximal interphalangeal joint at 11 years before presentation. This was followed by tenderness over the area, positive Tinel sign, and pain radiating proximally and distally. The patient underwent neurolysis and excision of a neuroma from the radial digital nerve at another institution 2 years before presentation to our clinic. Pathology confirmed the diagnosis of neuroma at that time. The patient had experienced resolution of the symptoms, but then he had gradually started to experience exquisite pain and tenderness distal to the site of the previous neuroma excision over the volar aspect of the digit.
Our physical examination revealed a normal-appearing finger with a nontender, radial midaxial scar at the level of the proximal interphalangeal joint and the middle phalanx with a negative Tinel sign. There was extreme nonradiating tenderness to palpation overlying the midline of the A4 pulley. The patient had full active range of motion with intact flexor digitorum profundus and superficialis function and no bowstringing. Sensation was intact distally with a 2-point discrimination of 4 mm. There were no signs of infection. Given the concern for a possible A4 pulley rupture or recurrent neuroma, an ultrasound was obtained. It revealed a focal, hypoechoic, hypervascular, 4 × 4 × 6 mm solid soft-tissue mass located adjacent to the radial volar aspect of the intact A4 pulley and displacing the digital nerve ulnarly (Fig. 1).
Surgical excision was performed with the use of a finger tourniquet with the patient under local anesthesia and sedation. Intraoperatively, a yellowish mass with distinctive borders was found within the radial digital nerve whose course was displaced ulnarly over the midline of the A4 pulley (Fig. 2). Intraneural microdissection was performed under loupe magnification (Fig. 3). The mass was noted to arise from one of the fascicles, which was excised en bloc with the mass (Fig. 4). The remaining fascicles were preserved. The mass was submitted to the pathology department, and its histology is shown in Figure 5.
Although an intraneural location is unusual, the histologic features were diagnostic of a benign glomus tumor.
At the 6-month follow-up, the patient had relief from preoperative pain, tenderness, and cold hypersensitivity. He had full active range of motion similar to that in the preoperative examination and remained symptom-free with intact sensation and 2-point discrimination of 4 mm comparable with other digits.
Proceed to Discussion >>Reference: Kwiecien GJ, Meaike J, Inwards CY, Rhee PC. Posttraumatic glomus tumor of the digital nerve with atypical presentation: a case report. JBJS Case Connector. 2022 Jul 8;12(3):e22.00166.
Glomus tumors account for 1% to 5% of all soft-tissue tumors developing in the hand. They typically present in the subungual area causing paroxysmal pain, tenderness, cold hypersensitivity, and sometimes nail deformities. When they occur in other locations within the hand, they may present a diagnostic challenge.
Glomus tumors originating from the digital nerves are extremely rare. Our literature review revealed only 7 case reports in addition to our patient. All of the reported cases occurred spontaneously, unlike the presented case where surgical trauma at the time of neurolysis for neuroma or the initial penetrating trauma may have triggered growth of the tumor more distally. The pathology of the original mass was not available for review, so it is possible that the mass that we identified represented a recurrence of the lesion interpreted as a neuroma, although this is less likely. Similar to our patient, most of the glomus tumors reported in the literature were diagnosed >2 years after symptom onset. The diagnosis of extraungual glomus tumors is often delayed, with 1 study showing a mean delay of 7.4 years. All the 7 patients had pain and tenderness along the mass. In our case, the digital nerve was displaced toward the volar midline. This could have been caused by a mass effect of the tumor or by the inadvertent transposition of the nerve at the time of neurolysis with scarring into this displaced position. Regardless of the etiology, our patient presented a diagnostic challenge and was initially misdiagnosed with an A4 pulley rupture.
The diagnosis of subungual glomus tumor is usually based on symptoms and physical examination. However, in cases of tumors involving digital nerves, preoperative imaging is important to determine the tumor size and the relation to the nerve and to consider other pathologies in the differential diagnosis, such as neuroma, schwannoma, or hemangioma. Magnetic resonance imaging (MRI) remains the most popular imaging modality. It can identify tumors as small as 2 mm, and most glomus tumors have a characteristic appearance with low-signal intensity on T1-weighted images, high-signal intensity on T2-weighted images, and strong enhancement after gadolinium injection. Ultrasound remains an attractive, cost-effective alternative. It can also identify tumors as small as 2 mm and allows for real-time adjustments. Glomus tumors are depicted as well-circumscribed, hypoechoic, hypervascular masses. In our patient, the use of ultrasound not only accurately diagnosed the pathology but also allowed for the simultaneous, dynamic assessment of the flexor sheath integrity, which ruled out an alternative diagnosis of an A4 pulley injury.
Complete surgical excision is the only feasible method for the treatment of glomus tumors. In 3 of the 7 previously reported cases, the tumor could be separated from the nerve entirely. In another 3 cases, 1 of the fascicles had to be excised with the tumor without reconstruction. In the remaining case, a segment of the entire digital nerve had to be excised with primary epineural repair. Transient numbness was common, but 5 of the 7 patients regained full sensation. Kline et al. reported persistent numbness after 1 of the 3 digital nerve fascicles was excised at the base of the thumb without reconstruction. Shinohara and Hirata reported mild small finger hypoesthesia after segmental excision of the digital nerve at the level of the middle phalanx after primary epineural repair. In the presented case, we discussed a possible nerve repair with the patient preoperatively. Despite the excision of one of the fascicles and no reconstruction, our patient recovered normal sensation after a brief period of transient numbness. However, it is important to counsel the patient that, in >50% of glomus tumor excisions involving the digital nerve, some portion of the nerve needs to be sacrificed, which may temporarily or permanently affect the sensation.
Finally, despite the glomus tumor being a benign lesion, it can recur if not completely excised. Among the 7 previously reported cases, there were no recurrences after the mean follow-up of 21 months (range, 10 to 36 months). Our patient had no signs of recurrence after 6 months and, at the time of this writing, was being closely followed.
Reference: Kwiecien GJ, Meaike J, Inwards CY, Rhee PC. Posttraumatic glomus tumor of the digital nerve with atypical presentation: a case report. JBJS Case Connector. 2022 Jul 8;12(3):e22.00166.
What is the diagnosis?
Glomus tumor
Lipofibromatous hamartoma of the peripheral nerve
Schwannoma (neurilemmoma)
Angiofibroma
Malignant peripheral nerve sheath tumor

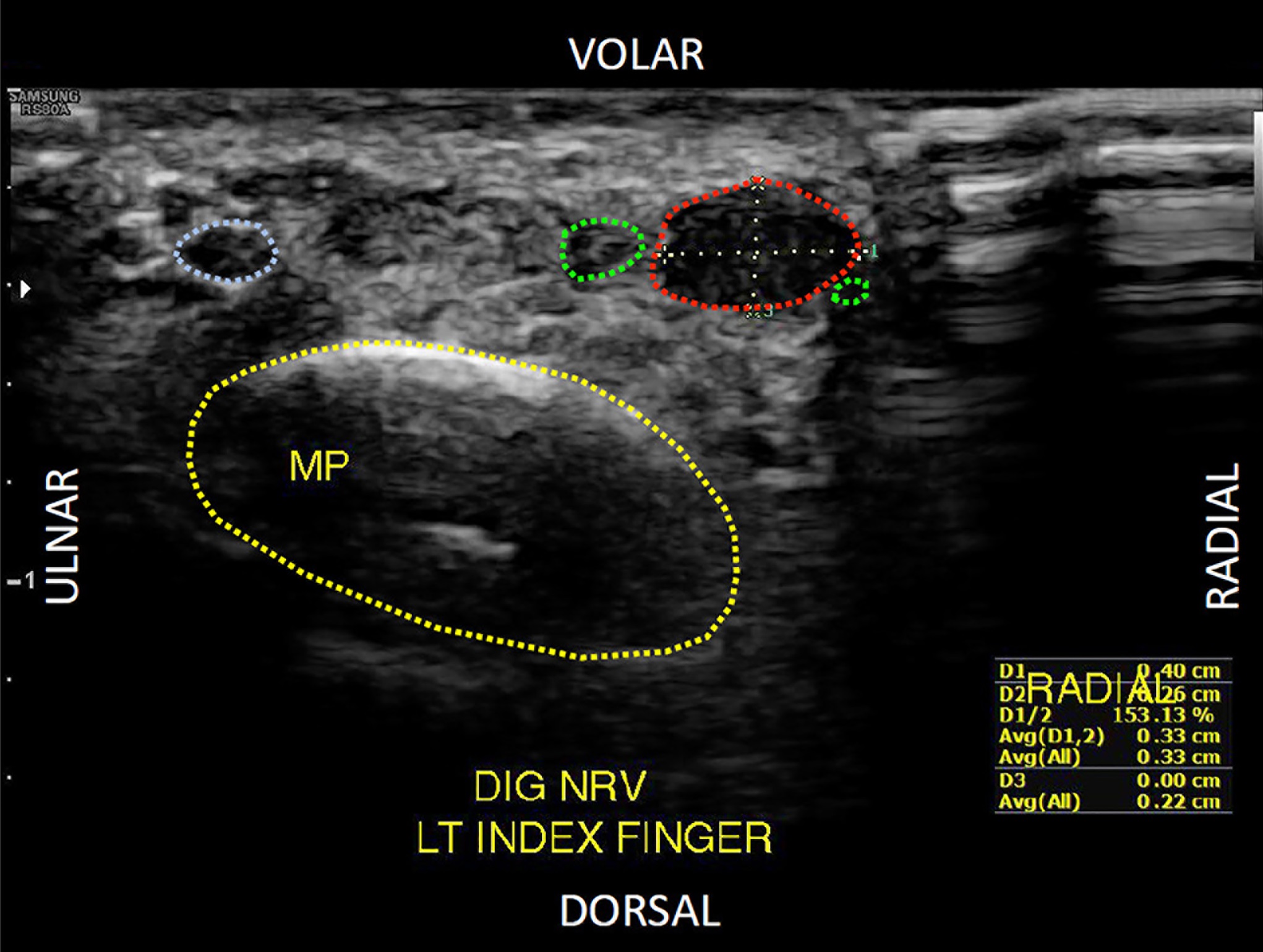
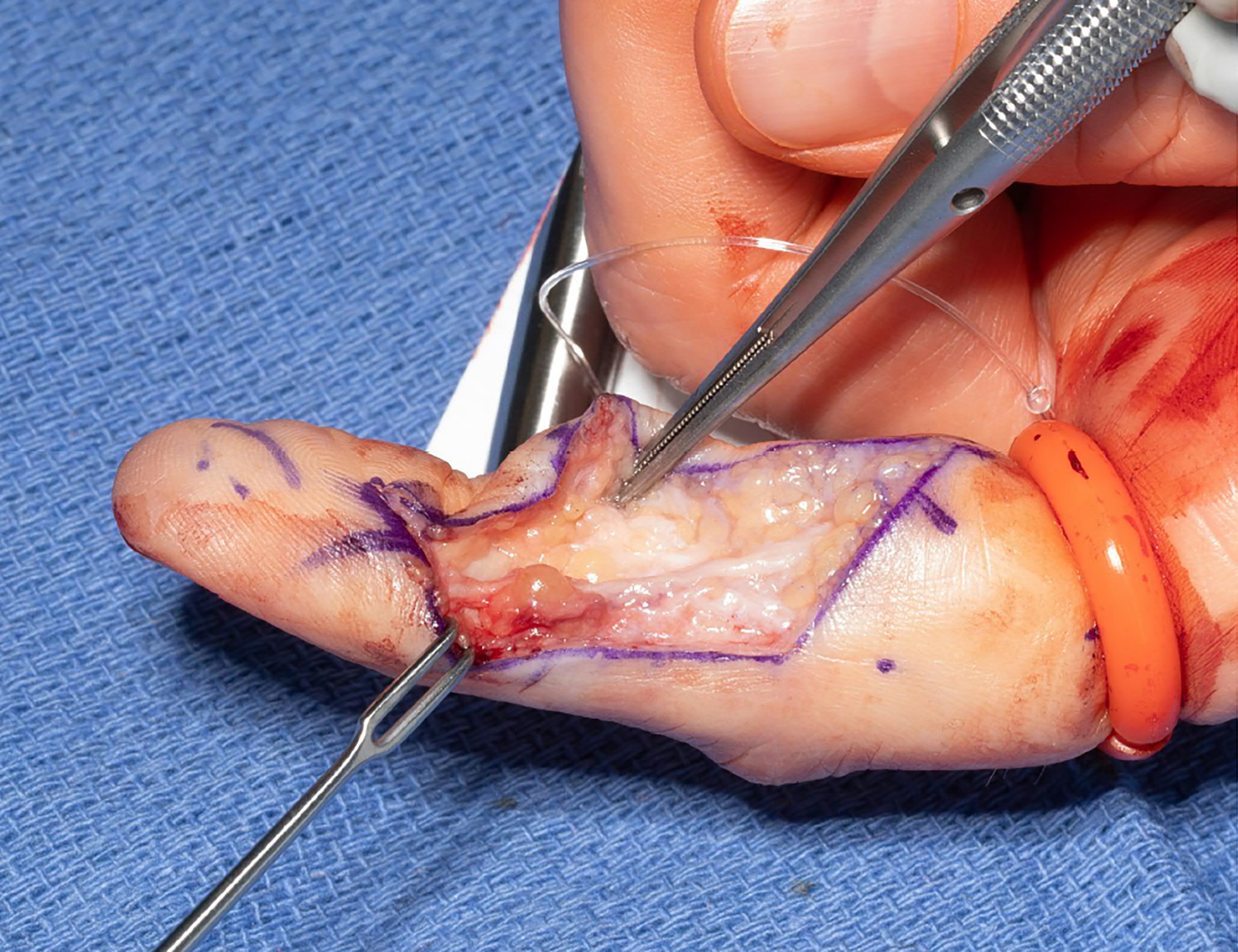
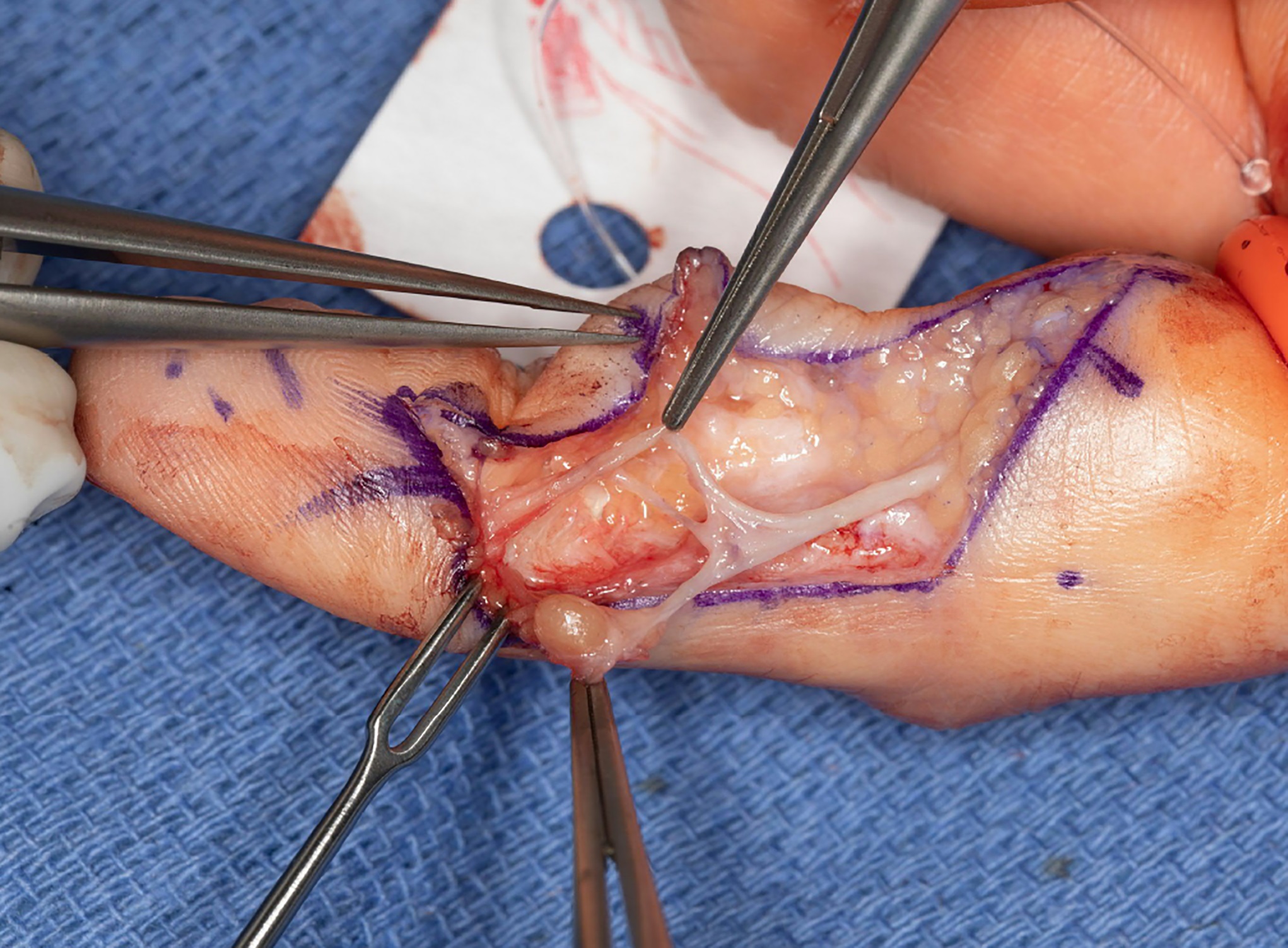

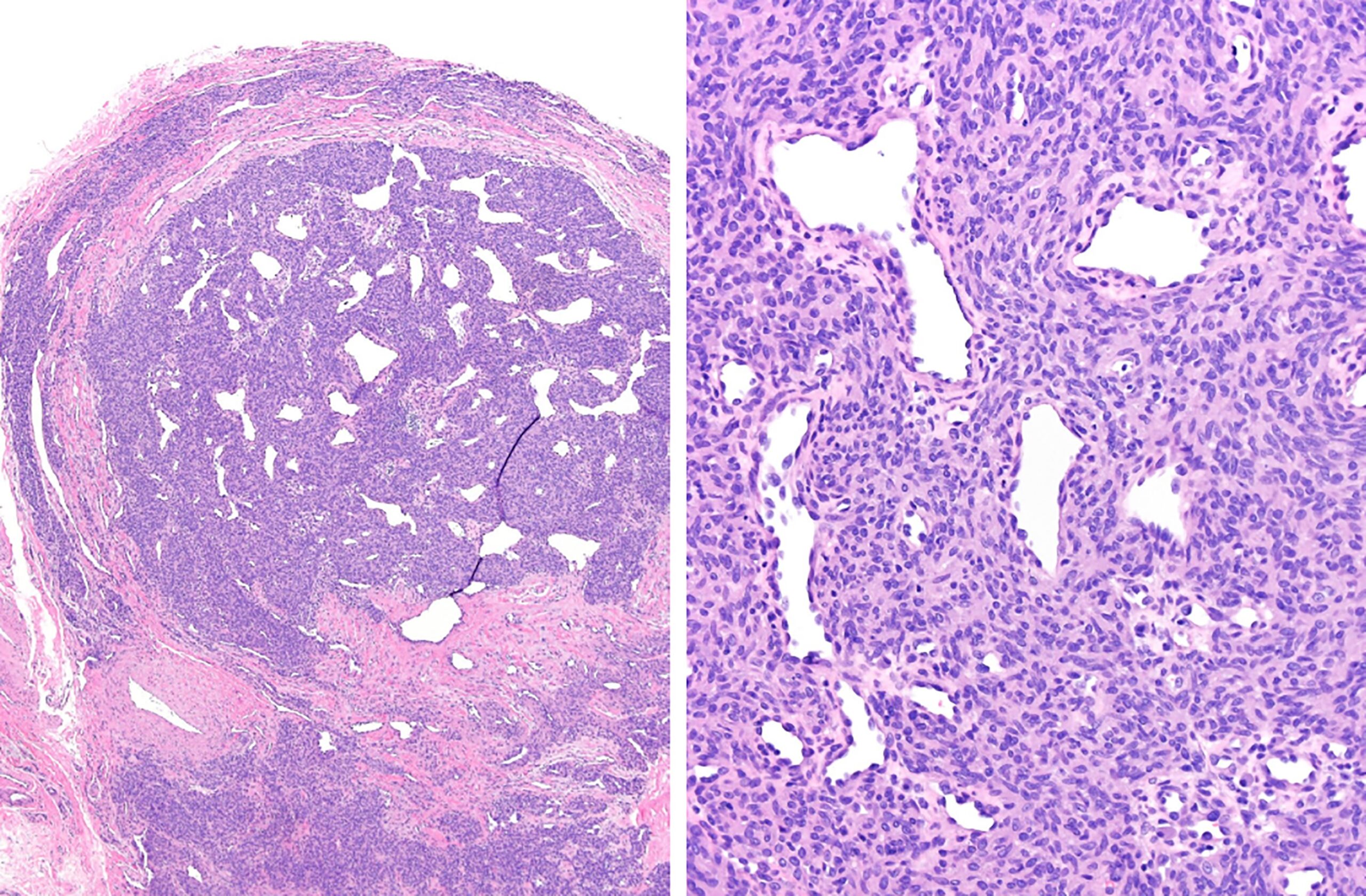
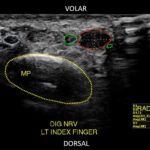 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4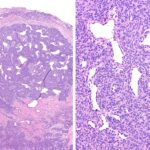 Fig. 5
Fig. 5