A 57-Year-Old Woman with Increasing Wrist Pain
January 3, 2024
A 57-year-old woman presented 6 years after bilateral carpal tunnel release with a 3-month history of nodularity, erythema, and tenderness to the bilateral scars. Increasing discomfort limiting daily hand function prompted an evaluation by her hand surgeon. Her medical history was notable for melanoma of the chest status after wide local excision, type II diabetes mellitus, hypertension, and hyperlipidemia. She was also diagnosed with systemic sarcoidosis in the interval since the carpal tunnel release, which had spontaneously resolved after treatment with continued asymptomatic remission for 3 years at the time of presentation. Physical examination displayed firm, tender subcutaneous nodules underlying 3-cm linear scars of the palmar wrists bilaterally (Figs. 1 and 2). The bilateral involvement in previously well-healed incisions many years postoperatively prompted further evaluation by biopsy. While awaiting pathology results, symptomatic management was attempted with silicone pad dressings and daily application of triamcinolone 0.1% topical cream, but neither provided substantial improvement with 1 month of use.
Bilateral punch biopsies were obtained (Figs. 3 and 4).
The pathology in the setting of the patient’s history and clinical presentation indicated a diagnosis of scar sarcoidosis.
Initiating treatment and monitoring response was pursued over further diagnostic testing for microbial causes of granulomatous disease because the patient had no systemic symptoms to indicate infection or a history of recent immunosuppression. Previous hilar mediastinal lymph node biopsies with acid-fast bacteria and Grocott’s methenamine silver stains at the time of primary sarcoidosis diagnosis were negative for microorganisms. Treatment with intralesional corticosteroid injections was undertaken. Using a 25-gauge needle, 1 mL of dexamethasone and 1 mL of lidocaine 1% without epinephrine were injected along the entire length of the hypertrophic scars. Over 5 months, the patient received 4 corticosteroid injections with progressive improvement in the presenting symptoms. At the 1-year follow-up, the patient experienced a complete resolution of the symptoms with no recurrence of carpal tunnel symptoms, and she continued remission for 2 years after the initial appearance of the lesion. She did not sustain a recurrence of systemic sarcoidosis and remained asymptomatic at the last follow-up.
Proceed to Discussion >>Reference: Meyer AM, Macdonald C, Fornadley JM, Taylor KF. Cutaneous sarcoidosis in bilateral carpal tunnel release scars: a case report. JBJS Case Connect. 2023 Oct 5;13(4):e23.00143.
Scar sarcoidosis describes the formation of noncaseating granulomas in preexisting scars and is associated with surgical procedures, trauma, tattooing, and herpes zoster infection. This is the first case, to our knowledge, of scar sarcoidosis developing after carpal tunnel release and a rare instance of bilateral disease. Cutaneous inflammatory granuloma formation in sarcoidosis is theorized to involve a complex interplay between host immune response, infectious process, environmental exposure, and underlying genetic predisposition. Cutaneous areas associated with damage to the underlying neuroimmune network are more likely to develop secondary skin diseases, termed immunocompromised districts. Factors known to disrupt cutaneous immune function include a surgical procedure, trauma, tattooing, herpetic infection, chronic lymph stasis, ultraviolet and ionizing radiation, and intradermal vaccines. For instance, in areas of prior trauma, a surgical procedure, or herpetic infection, damage to sensory nerve fibers can impair the release of immunity-related peptides, whereas disruption of lymphatic drainage can impair the normal movement of immunocompetent cells. The mechanism of immune destabilization is multifaceted and is likely the result of amalgamation of damage and disruption over time. Several studies demonstrated that the association between foreign material and sarcoid granuloma formation is not mutually exclusive, further suggesting that foreign material may act as a nidus for granulomatous inflammation. In a histological review of 32 cases of cutaneous sarcoidosis, 26% of biopsies contained concurrent birefringent foreign material. Regardless of the insult, the combination of varying clinical factors associated with immunocompromised districts potentiates a shared pathogenesis of local neuroimmune network disruption, resulting in an increased susceptibility to granulomatous dysimmune reactions in affected skin areas.
This case illustrates a unique presentation of scar sarcoidosis, a disease that is often overlooked and is commonly mistaken as a foreign-body reaction and is misdiagnosed as a hypertrophic scar or keloid, especially with asymptomatic lesions. From a surgical perspective, it is important to consider the diagnosis of cutaneous sarcoidosis in patients who present with nodularity, discoloration, and tenderness in previously benign well-healed incisions. As demonstrated in this case, cutaneous manifestations occur at variable latency periods to systemic disease, with intervals from 6 months to 59 years reported in the literature. Suh and Ahn discussed 2 cases of scar sarcoidosis after blepharoplasty, 15 and 30 years after the procedure, with one of the subjects developing bilateral disease. Demirkök et al. described scar sarcoidosis of a thyroidectomy scar at 17 years after the procedure. Scar sarcoidosis was also reported within the site of a previous melanoma scar at 4 years after the procedure, as described by Fournier et al. Our patient developed cutaneous manifestations at 5 years after the initial diagnosis without recurrence of systemic involvement at the last follow-up. Cutaneous sarcoidosis may also precede systemic involvement and, in rare instances, occur in isolation. Routine monitoring after cutaneous sarcoidosis presentation is imperative because cutaneous lesions may signal exacerbation or relapse of systemic sarcoid disease. A thorough workup and care coordination with a pulmonologist are recommended, especially in the presence of systemic symptoms to exclude additional causes of granulomatous disease.
Treatment and management of scar sarcoidosis should consider the involvement of systemic disease, the severity of symptoms, and the impact on the patient’s quality of life. Intralesional glucocorticoid injections are considered a first-line treatment for cutaneous sarcoidosis. The number of injections and the treatment interval are largely based on the response to treatment because current guidelines lack consensus on the dose, frequency, and duration of treatment. The prognosis is favorable for cutaneous lesions, with slow, spontaneous resolution in most cases. Systemic corticosteroids are reserved for multiorgan involvement or disseminated cutaneous lesions refractory to therapy. Although cutaneous sarcoidosis is not life-threatening, prolonged inflammation can cause disfigurement that impairs quality of life. In this case, the patient’s ability to engage in activities of daily living had been substantially hindered by pain and wrist sensitivity, and treatment initiation was prioritized.
Topical corticosteroids were trialed initially to avoid the effects of systemic corticosteroid therapy in the setting of the diabetes that the patient had. However, the severity of symptoms impairing the patient’s daily function prompted the initiation of intralesional corticosteroid injections. High-potency topical corticosteroids have not demonstrated similar efficacy. Excision has been reported to be successful with small lesions, although it is not recommended because it may further induce sarcoid infiltrates or cause scar sarcoidosis. The prognosis of cutaneous disease is favorable, and prevention can be prioritized through early recognition and initiation of treatment.
In conclusion, scar sarcoidosis should be considered when presented with a cutaneous lesion in association with a cutaneous scar, either as primary presentation or as a disease recurrence.
Reference: Meyer AM, Macdonald C, Fornadley JM, Taylor KF. Cutaneous sarcoidosis in bilateral carpal tunnel release scars: a case report. JBJS Case Connect. 2023 Oct 5;13(4):e23.00143.
What is the diagnosis?
Metastatic malignant melanoma
Amyloidosis associated with carpal tunnel syndrome
Granulomatous reaction to yeast (fungal infection)
Scar sarcoidosis
Foreign-body (suture) granulomas



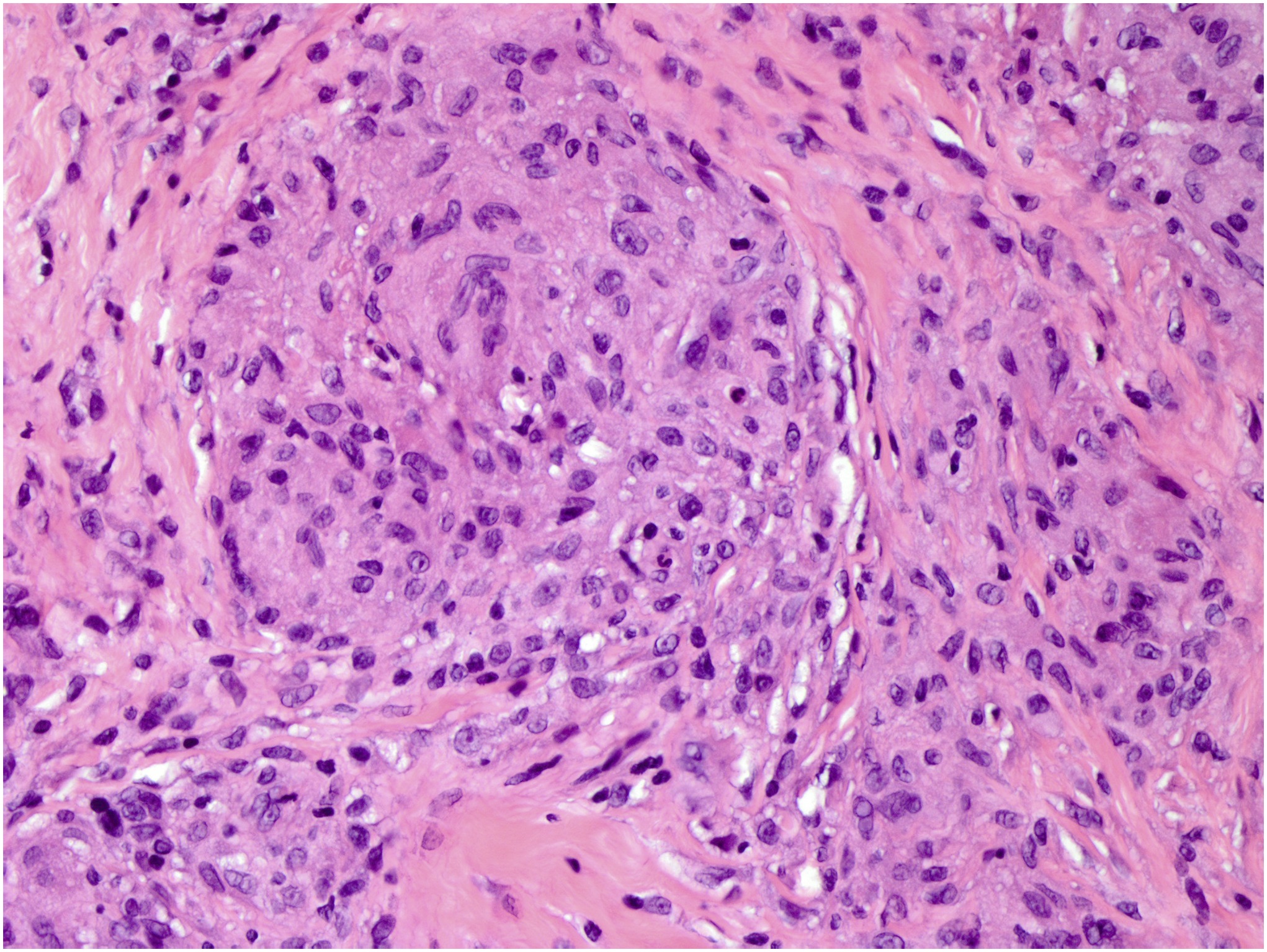
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4