A 58-Year-Old Man with Foot Numbness Following a Car Accident
January 6, 2021
The patient is a 58-year-old man with a history of hypertension, diabetes mellitus complicated by neuropathy, and obesity (body mass index of 42 kg/m2) who presented for the evaluation of pain, edema, and numbness in the left hindfoot following a motor vehicle collision. Following the motor vehicle collision, the patient was referred to a podiatrist by his primary care physician for the treatment of pain. Conventional radiographic images at that time were read as negative. The patient experienced an exacerbation of pain in the same foot 8 months later when he felt a pop following a fall from standing. Following this exacerbation, the patient returned to his podiatrist and underwent 6 weeks of casting followed by a course of physical therapy. After these treatments failed to relieve the pain that the patient was experiencing, he underwent magnetic resonance imaging (MRI).
The MRI, per report, revealed diffuse bone marrow edema in the talus and navicular bones, an erosive irregularity at the talonavicular joint, and a large, multiloculated fluid collection. The radiologist included osteonecrosis, stress fractures, advanced erosive arthropathy, and infection in his differential diagnosis. The nuclear scan displayed a focal area of uptake in the anterior aspect of the talus and talar head. Moderate to severe degenerative changes were also noted in the hindfoot and midfoot joints with numerous subchondral cysts present. No fracture or midfoot collapse was noted.
After imaging, the patient was examined in an orthopaedic clinic. Here, he was diagnosed with Charcot arthropathy, and his symptoms were not relieved by a trial of ibuprofen and an air cast boot. Because of the patient’s insistence that his symptoms did not exist prior to his injury, he sought treatment with a foot and ankle specialist 19 months after the motor vehicle collision.
During his initial visit to the foot and ankle clinic, the patient reported numbness and pain over the anterior ankle and the medial and plantar surfaces of the foot. On physical examination, he was tender to palpation over the anterior ankle, lateral talonavicular joint, and sinus tarsi. He was also noted to have some mild edema of the dorsal foot. Radiographs revealed chronic-appearing deformity of the midfoot with some sclerotic changes of the osseous structures, midfoot sag, and advanced degenerative changes of the talonavicular, subtalar, and midfoot joints (Fig. 1).
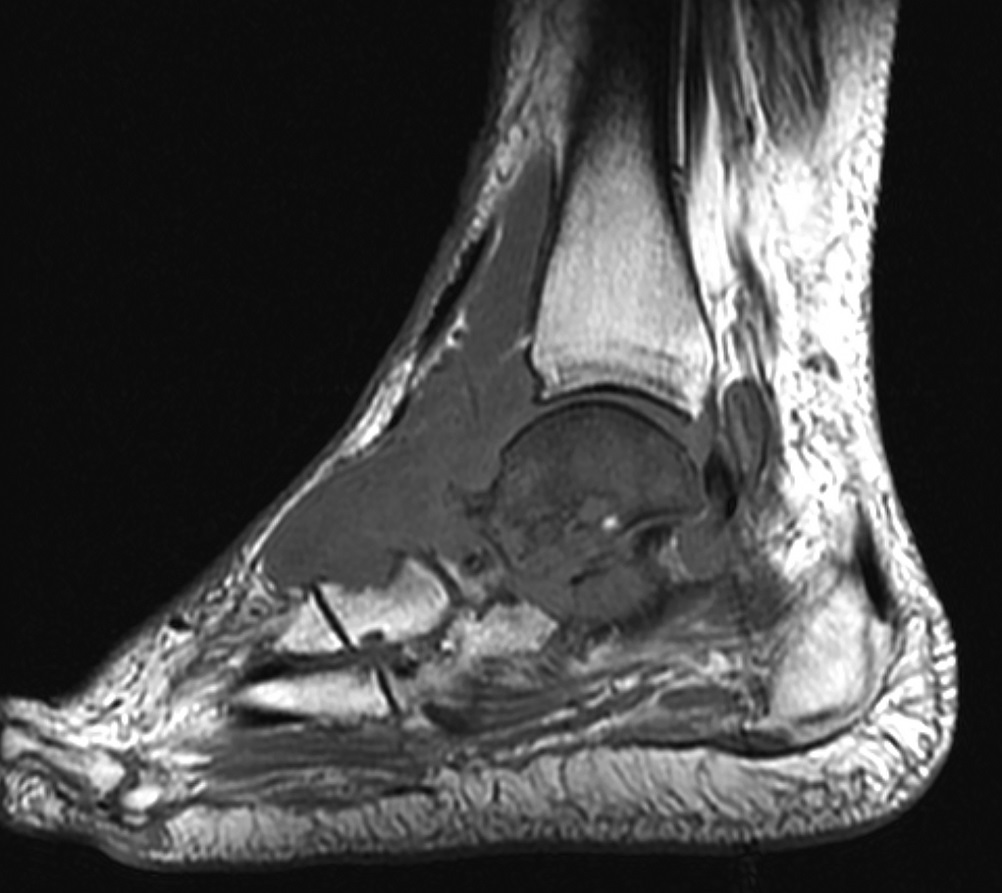
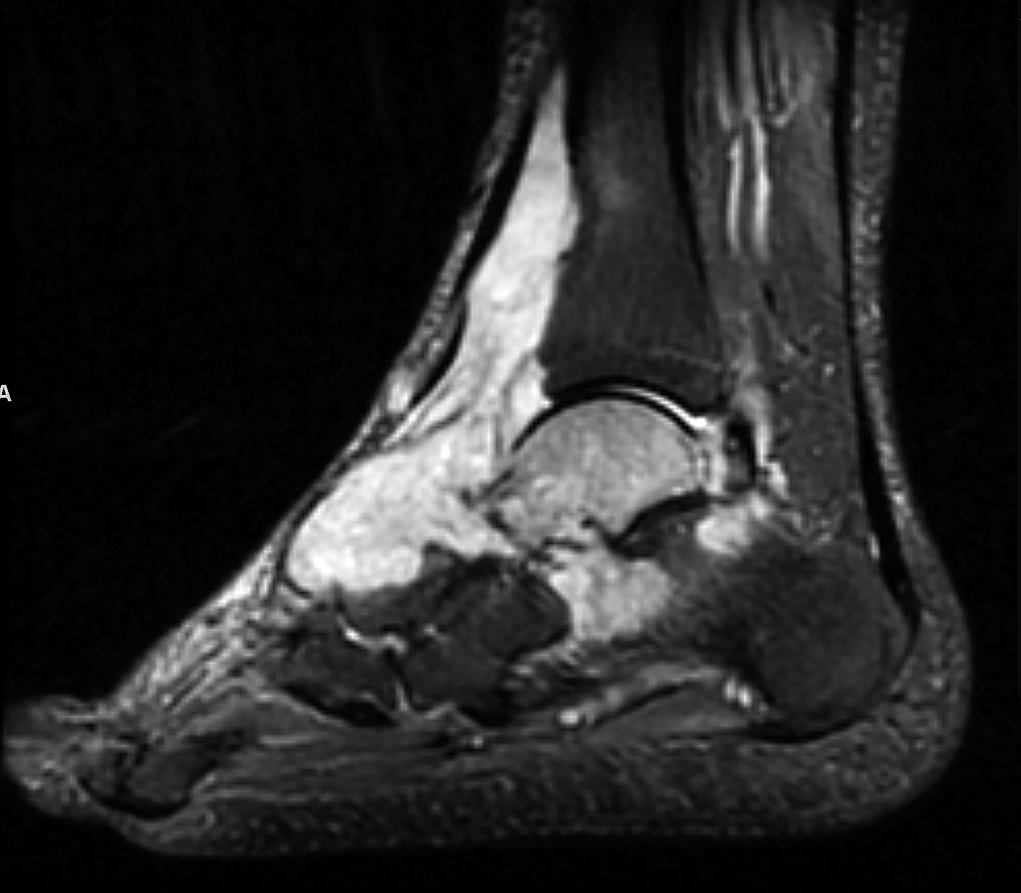
Because of the patient’s clinical picture and preexisting neuropathy, these radiographic findings were believed to be consistent with remote trauma and degenerative Charcot arthropathy. A new MRI of the foot and ankle without contrast was ordered to evaluate for osteonecrosis compared with talar edema, as osteonecrosis would prognosticate poorly for the success of future arthrodeses. Before MRI, potential surgical plans were discussed because of the midfoot degeneration including subtalar, talonavicular, naviculocuneiform, and first tarsometatarsal fusions. Additional imaging studies were obtained (Figs. 2-A and 2-B).
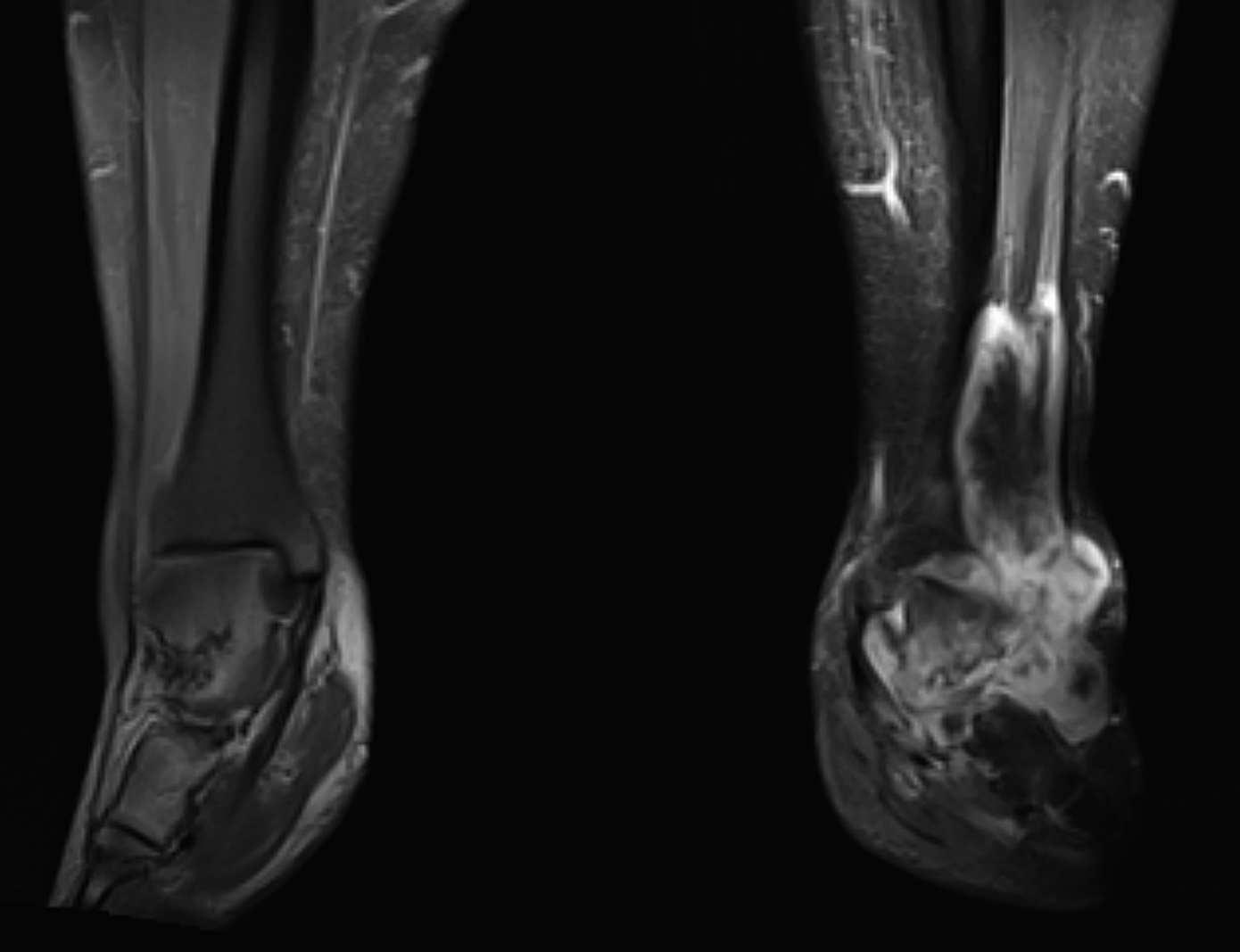
The MRI revealed a T2 hyperintense and T1 hypointense mass that appeared to have an epicenter in the soft tissue of the anterior ankle, contiguous with the talar neck and anterior talar dome. This mass extended from its origin, interdigitating in the syndesmosis, tibiotalar joint, subtalar joint, calcaneonavicular joint, and sinus tarsi. Erosive, invasive changes with associated bony edema and cortical discontinuity were noted in the talus, navicular, calcaneus, cuneiforms, and anterior distal part of the tibia. The patient was referred to an orthopaedic oncologist, who recommended ultrasound-guided core needle biopsy. Histology is shown in Figures 3-A and 3-B.
The lesion showed a neoplastic infiltrate of deeply eosinophilic cells arranged in cords and nests in a relatively hypocellular chondromyxoid ground stroma. The nuclei were round and ovoid with only thin, inconspicuous nucleoli identified. These features are diagnostic of extracellular myxoid chondrosarcoma. Some imaging examples of extracellular myxoid chondrosarcoma are shown in Figures 4 through 7. Given the limited proximal extent of the tumor, the patient underwent left below-the-knee amputation.
Staging workup included a computed tomography (CT) scan of the chest, which revealed diffuse pulmonary metastases, and an MRI of the tibia and fibula with and without contrast to evaluate the extent of the tumor. This MRI showed a 13.1 × 7.5 × 11.1-cm T2 hyperintense and T1 hypointense lobular mass with invasion of the syndesmosis (Fig. 4). However, no foreleg lesion was identified proximal to the original mass.
Six weeks postoperatively, the patient was seen by a medical oncologist and was administered the chemotherapeutic agent pazopanib 600 mg daily. The patient received a prosthesis at 10 weeks postoperatively. He reported pain as 0 of 10, and a CT scan of his chest showed stable pulmonary metastases. Seven months after initiating pazopanib chemotherapy, the patient had an unscheduled return to the oncology clinic because of masses that he had detected in his left groin. A CT scan found 2 new groin masses measuring up to 4.3 cm in diameter, the largest lung metastasis with minimal growth from 1.7 to 1.8 cm, and a new 3.5-cm right renal metastasis. His treatment regimen was switched to 37.5 mg of sunitinib taken daily. After 3 months of taking sunitinib and a total of 11 months after amputation, a repeat CT scan showed shrinking groin and renal masses and stable lung metastases. At the time of this writing, the patient was taking sunitinib and continued to undergo scheduled CT scans with medical oncology follow-up.
Proceed to Discussion >>Reference: Wilson JT, Pitts C, Hess M, Phillips SG, Siegal GP, Johnson MD. Extraskeletal myxoid chondrosarcoma of the midfoot presenting as Charcot arthropathy: a case report. JBJS Case Connect. 2019 Dec;9(4):e0458.
Extraskeletal myxoid chondrosarcoma is a rare soft-tissue malignancy that is twice as common in men than in women and typically presents in the sixth decade of life. It very rarely presents in the foot or ankle and, as a result, is not commonly in the differential of patients presenting with foot pain.
In comparison, Charcot arthropathy is a disease process characterized by fractures and dislocations resulting from decreased sensation. This lack of sensation can allow repetitive, unnoticed microtrauma to occur, predominantly in the weight-bearing portions of the joints. If these microtraumas do not heal, they can lead to degenerative joint disease, fractures, dislocations, and collapse of the arch (for example, Fig. 5). This condition is often associated with poorly controlled diabetes but can arise from other neuropathic conditions.
Extracellular myxoid chondrosarcoma is a rare neoplasm with a scarcity of information concerning its origin, epidemiology, risk factors, and treatment. The mean age of presentation is in the sixth decade of life, with a male predominance of 2:1. MRI is the preferred imaging modality and typically shows a poorly circumscribed, nodular mass ranging from 3 to 40 cm in maximal diameter. Histopathology is typically needed for diagnosis and shows characteristics of cartilage within a myxoid stroma. A t(9; 22) (q22; 12.2) genetic translocation joins the genes EWSR1 and NR4A3 and is often associated with extracellular myxoid chondrosarcoma, although other possible translocations exist. The current standard treatment is local excision. External beam radiation therapy has also proven to be effective. It is often used as an adjuvant in the postoperative period. Trials of chemotherapy have demonstrated poor results.
In our patient, Charcot arthropathy was repeatedly the working diagnosis for multiple providers given his history of morbid obesity, diabetes mellitus, neuropathy, and clinical presentation. The patient had standing foot and ankle radiographs that appeared remarkably similar to Charcot arthropathy, showing midfoot sag and arthritic changes of the subtalar, talonavicular, and naviculocuneiform joints. The distinguishing feature in our patient’s radiograph is the apparent erosion of the osseous dorsal midfoot structures (Fig. 1) rather than the heterotopic ossification and osteophytes observed in Charcot arthropathy (Fig. 5).
In this case, obtaining an MRI led to a biopsy that determined the final diagnosis. For extracellular myxoid chondrosarcoma, signal intensity on T1-weighted imaging is similar to that of muscle in a majority of cases. On T2-weighted imaging, most tumors have been shown to display intensity equal to or greater than that of fat. Our patient’s noncontrast MRI showed diffuse increased T2/short tau inversion recovery (STIR) signal and decreased T1 signal (Figs. 6-A, 6-B, 7-A, and 7-B). A contrast MRI showing heterogeneous enhancement with T2 hyperintensity helped to better characterize the mass and to define its borders before excision (Fig. 4).
Chemotherapy has provided little, if any, success in the treatment of extracellular myxoid chondrosarcoma. Previously, data were obtained from chemotherapeutic courses given to patients, and only 25% yielded stable disease for ≥6 months. The remaining courses of chemotherapy resulted in stable disease for <6 months or progressive disease; no patients demonstrated a complete response. These results were radiographically determined and obtained from a multifarious combination of chemotherapeutic agents. The disappointing tumor response to chemotherapy demonstrates the limited role that current agents play in treatment of this disease. In our patient, pazopanib, although approved by the U.S. Food and Drug Administration for the treatment of soft-tissue sarcomas, did not seem to be effective. Sunitinib, although not officially approved for use in extracellular myxoid chondrosarcoma, has shown results in small studies and appeared to show efficacy in our patient as, at the time of this writing, he had yet to show local recurrence or increased development of his metastases.
From the current literature, the only curative treatment for extracellular myxoid chondrosarcoma is wide local excision of tumor-containing tissue. External beam radiation therapy has proven to be beneficial in reducing preoperative tumor burden and as a postoperative adjuvant therapy. This patient had metastatic disease before surgery, so amputation was performed for symptomatic relief and to prevent proximal tumor spread. In patients who do not present with metastatic disease, wide local excision or amputation is potentially curative. After follow-up for the amputation and being fitted for the prosthesis, at the time of this writing, the patient no longer had any pain symptoms and had been subjectively well.
Reference: Wilson JT, Pitts C, Hess M, Phillips SG, Siegal GP, Johnson MD. Extraskeletal myxoid chondrosarcoma of the midfoot presenting as Charcot arthropathy: a case report. JBJS Case Connect. 2019 Dec;9(4):e0458.
What is the diagnosis?
Charcot arthropathy with inflammatory pseudotumor
Chondromyxoid fibroma
Langerhans cell histiocytosis
Plasma cell myeloma
Extraskeletal myxoid chondrosarcoma


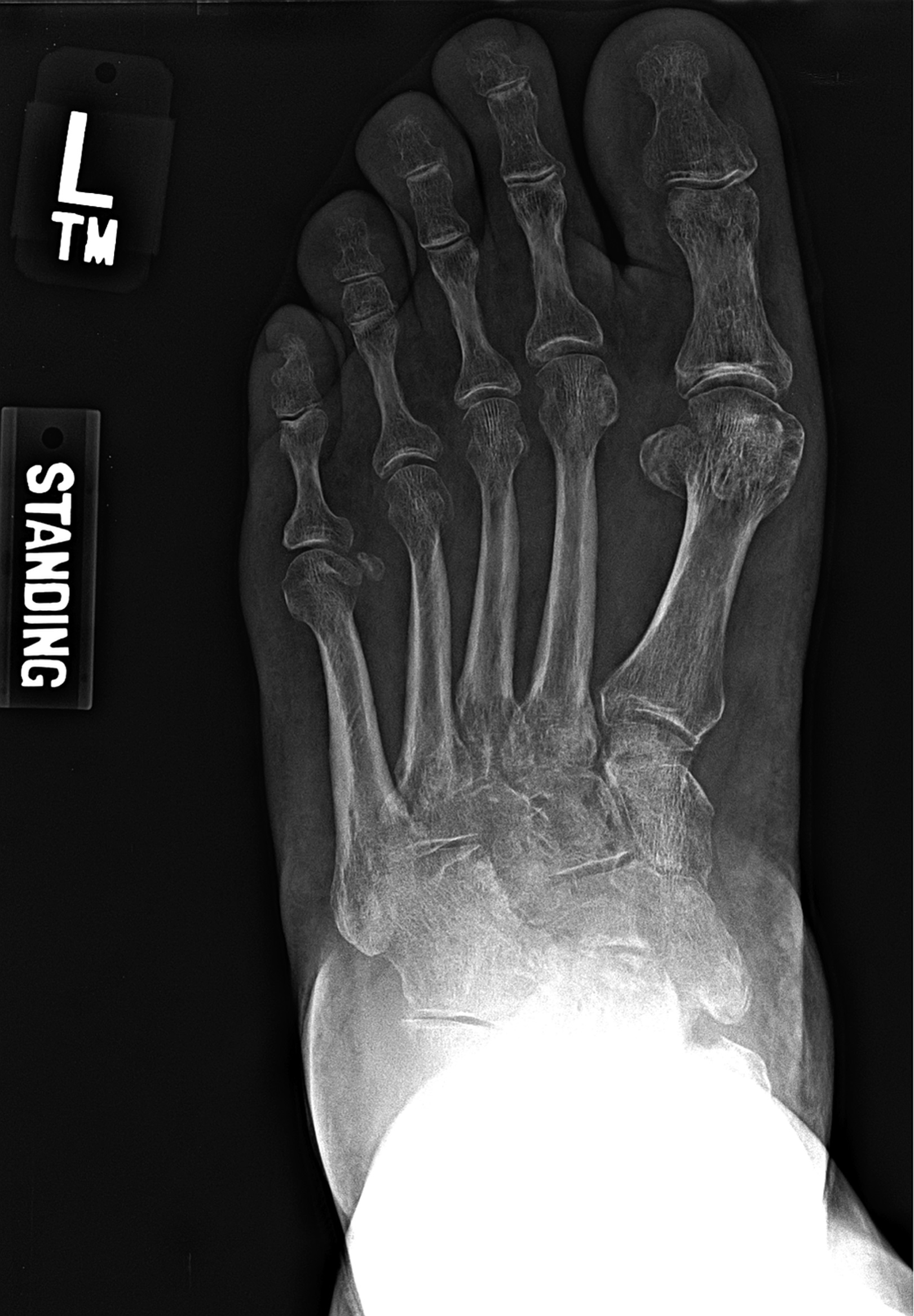

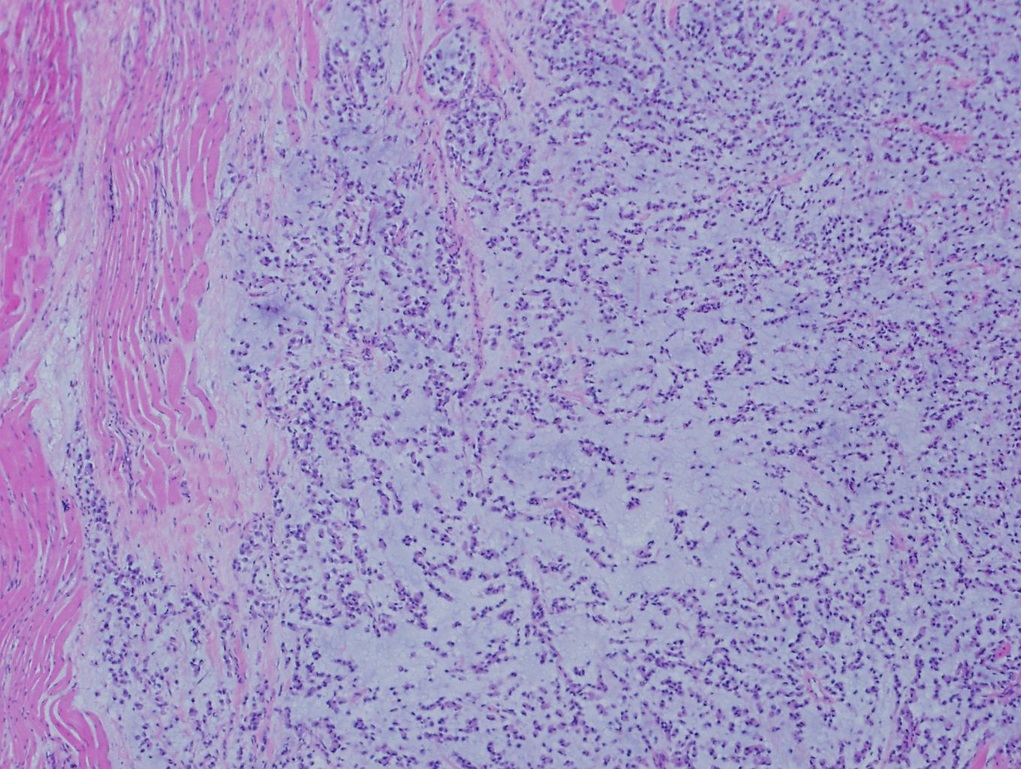
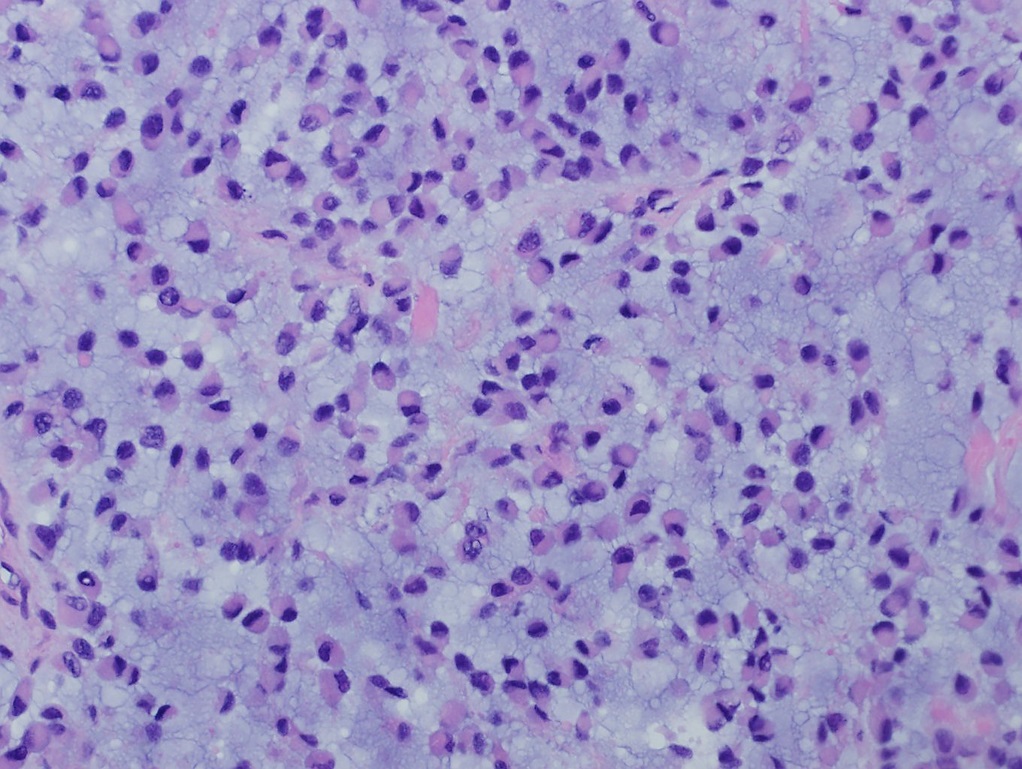
 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B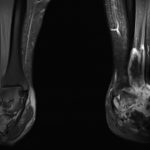 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6-A
Fig. 6-A Fig. 6-B
Fig. 6-B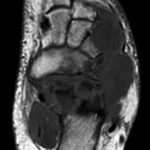 Fig. 7-A
Fig. 7-A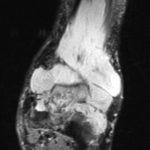 Fig. 7-B
Fig. 7-B