A Fifteen-Year-Old Boy with Recurrent Back Pain
December 7, 2011
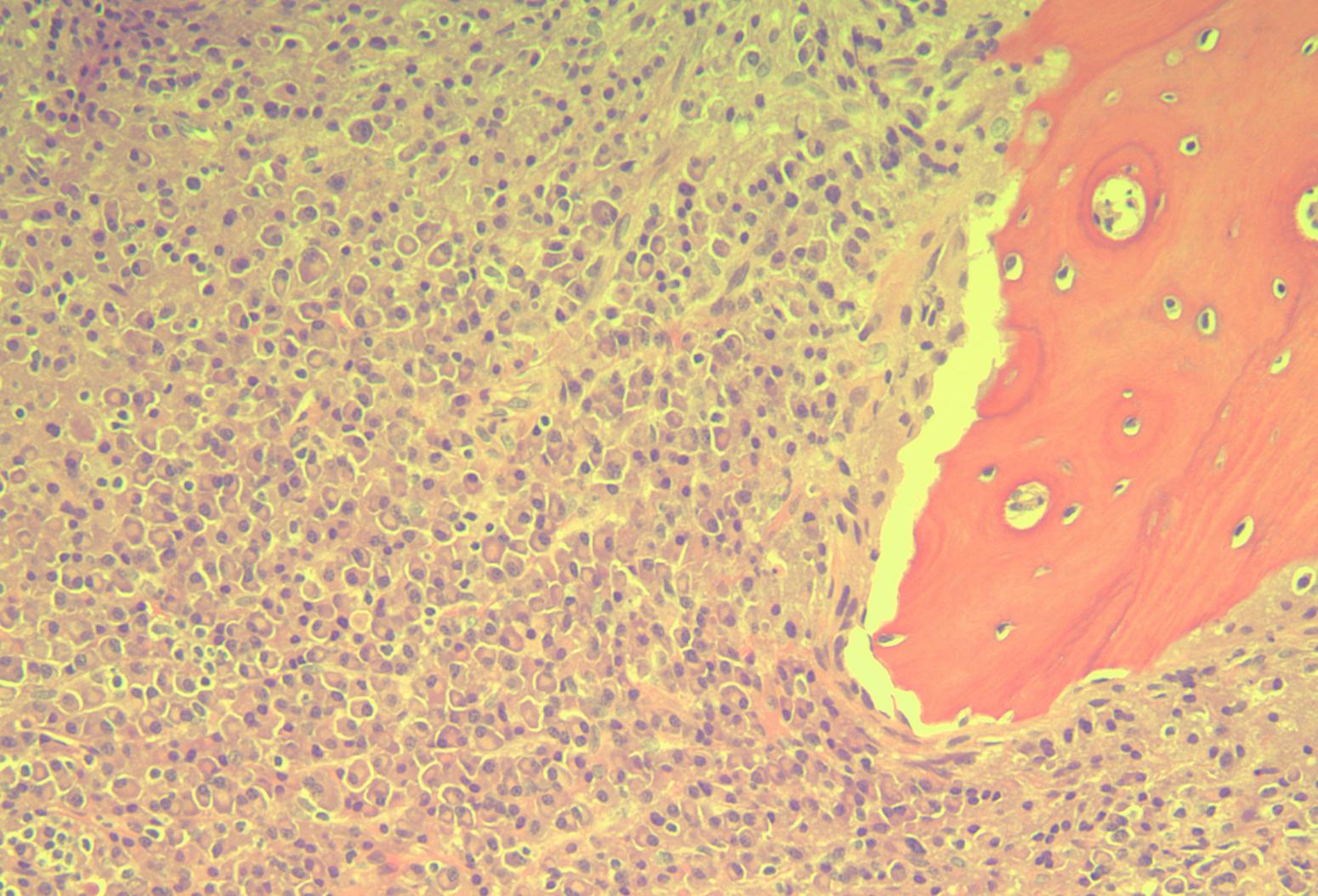
An otherwise healthy fifteen-year-old boy was referred in October of 2008 after several months of lower thoracic back pain and a progressive gait abnormality. He had been seen at another institution sixteen months earlier because of mild back pain. A radiograph at that time was negative, but a subsequent bone scan showed increased uptake in the T10 vertebral body (Fig. 1). The patient was managed with a Jewett-type back brace and oral nonsteroidal anti-inflammatory drugs, with some pain relief. Six months later, radiographs showed an isolated T10 vertebra plana (Fig. 2). Physical examination revealed only mild tenderness over the T10 area and pain with extremes of back motion but no neurologic deficits. A complete blood count with differential and the C-reactive protein level were within normal limits. Magnetic resonance imaging (MRI) of the thoracolumbar spine showed an isolated T10 vertebra plana with 80% loss of vertebral height, maintenance of the adjacent disc spaces, minimal vertebral retropulsion without cord compression, minimal edema within the vertebral body, and no soft-tissue component or posterior element involvement (Figs. 3-A and 3-B). A working diagnosis of vertebra plana secondary to Langerhans cell histiocytosis was made, and the patient was managed nonoperatively and was encouraged to slowly return to activities when asymptomatic. At the time of the six-month follow-up, the patient had no changes on examination or on radiographs. More than a year after the initial presentation, the patient returned to our clinic after three weeks of slowly worsening lower extremity paresthesias, intermittent subjective coolness in the foot and ankle bilaterally, an unsteady gait, and worsening middle and lower back pain. The patient walked with a mild slapping gait and had difficulty walking in a straight line without external aids. Physical examination showed grade-5 (of 5) motor strength in all extremities but decreased sensation to light touch and pinprick in the foot and ankle bilaterally. In each lower extremity, he had 4+ ankle reflexes, a positive Babinski sign, and decreased great toe proprioception. Radiographs showed continued T10 flattening with a new 50% loss of height of the L5 vertebral body (Fig. 4). A skeletal survey showed vertebra plana of T10 and L5 with radiolucencies in the left second and right tenth ribs and in the right parietal skull region (Fig. 5). A repeat MRI showed increased vertebral retropulsion with cord compression, posterior element involvement at T10, and a large soft-tissue component at T10 causing circumferential encasement of the thecal sac. There were interval T2 signal changes within the vertebral bodies of T3, L1, L4, and L5, with mild retropulsion and an associated soft-tissue mass (Fig. 6-A). Additional findings on computerized tomography (CT) with contrast included a soft-tissue component on the left second rib lesion and expansile radiolucencies in the left ninth rib, left glenoid, bilateral iliac wings, and right posterior acetabulum (Fig. 6-B). Computerized tomography with contrast of the chest, abdomen, and pelvis demonstrated negative findings, with no organomegaly or lymphadenopathy. Given the multiple lesions and clinical findings, the patient was referred to a pediatric oncologist and was admitted to the hospital. Serum studies included a complete blood count, including a white blood-cell count (5.2 × 109/L), hemoglobin (14.5 mmol/L), hematocrit (44.9%), platelets (323 × 109/L), and absolute neutrophil count (3000 cells/µL; normal, 1500 to 8000 cells/µL). Electrolytes, renal function, liver function, albumin, prealbumin, and serum uric acid were all within normal limits. The sedimentation rate and the lactate dehydrogenase were mildly elevated at 43 mm/hr and 280 IU/L, respectively. Computerized tomography-guided biopsy was performed at L5 (Fig. 7).
The diagnosis of multiple myeloma was made. Langerin, CD1, and S100 were negative. CD79a and CD138 showed variable positive staining. There was no staining for kappa and diffuse staining for lambda. Heavy chain stains showed IgA restriction in the plasma cells, with no staining for IgG, IgM, or IgD. Subsequent blood work showed elevated serum IgA (1440 mg/dL; normal, <435 mg/dL). Serum and urine immunoelectrophoresis identified a monoclonal IgA protein. Serum protein electrophoresis (SPEP) showed an increase in alpha-II globulin as well as gamma globulin and a monoclonal protein detected at a concentration 1.33 g/dL. The biopsy was negative for the 13q14.2 deletion, for loss of the ATM tumor suppressor gene, and for the CCND1 and IgH rearrangements. Radiation therapy to the T10 and L5 vertebrae and intravenous dexamethasone were started during the initial admission, with substantial neurologic improvement by two days. A combination of Revlimid (lenalidomide) and steroids was initiated, with enoxaparin followed by aspirin for prophylaxis against deep-vein thrombosis. The patient continued to receive zoledronic acid every month along with calcium and vitamin-D supplementation. In April 2010, the patient underwent an uneventful stem cell transplantation. The back pain had remained minimal, and the neurologic symptoms had not recurred since the initiation of treatment. At the time of the latest follow-up, the patient had not had any major illnesses or adverse reactions to treatment but did complain of fatigue.
Proceed to Discussion >>Reference: Greenleaf RM, Ricciardella LF, Latona CR, Sangimino MJ. Vertebra plana in an adolescent caused by multiple myeloma. A case report and review of the literature. J Bone Joint Surg Am. 2011;93:e37(1-7).
Vertebra plana was first described by Jacques Calvé in 1925 in a report on two pediatric patients with a single compressed vertebral body. Calvé believed that the radiographic finding represented vertebral body osteochondritis, which he described as “what Keohler’s disease is to the foot.” The work by Calvé and Buchman defined the classic radiographic findings as (1) involvement of only one vertebra, (2) lack of adjacent intervertebral disc involvement, (3) widened intervertebral disc space, and (4) greater opacity of the involved, collapsed vertebral body. Compere et al. and Lichtenstein reviewed multiple case reports and proposed that the cause of vertebra plana was eosinophilic granuloma. Eosinophilic granuloma along with Hand-Schüller-Christian disease and Letterer-Siwe disease are three variations of Langerhans cell histiocytosis (LCH), which is the term that is most commonly used today. There is an annual incidence of 5.4 cases per million children per year. Eosinophilic granuloma is the most common and benign form, is isolated to bone, and is typically monostotic but may occur in multiple locations, including the spine, skull, and ilium. The peak incidence occurs between five and ten years of age. Radiographic findings include lytic vertebral lesions with poorly defined margins, sparing of posterior elements, preservation of the adjacent disc space, and a predilection for the thoracic spine. Surgical interventions, including curettage, grafting, decompression, and stabilization, have been advocated in the past. Recent long-term follow-up studies have shown good results following nonoperative treatment in children, so surgery should be reserved for adults with neural compromise or substantial deformity or instability. The classic radiographic findings of vertebra plana are strongly suggestive of eosinophilic granuloma. Other, less common causes include trauma, Gaucher disease, osteomyelitis, coccidiodomycosis, tuberculosis, myofibromatosis, aneurysmal bone cyst, osteosarcoma, leukemia, lymphoma, Ewing sarcoma, and giant-cell tumor. To our knowledge, there have been no reported cases of multiple myeloma presenting as isolated vertebra plana. Multiple myeloma is the most common primary bone malignancy and is the second most common blood cancer after non-Hodgkin lymphoma. It is an adult disease, with a median age of seventy years at the time of diagnosis, and rarely presents before the age of forty years. Plasma cells are a type of B cell that normally produces immunoglobulins in the bone marrow. In multiple myeloma, myeloma plasma cells proliferate uncontrollably and overproduce the cell’s respective immunoglobulin; these serum monoclonal immunoglobulins are known as the M protein. The presenting symptoms of multiple myeloma, in order of prevalence, are bone pain (especially back pain), fatigue, pathologic fractures, weight loss, and paresthesias. One-third of patients are asymptomatic when diagnosed, and osseous lesions often show decreased uptake on nuclear bone scans. The definitive diagnosis of multiple myeloma requires advanced testing. Electrophoresis identifies excess protein from monoclonal antibodies (the M protein) in the blood and detects the light-chain component of these antibodies in urine (Bence-Jones proteinuria). Biopsy of bone marrow aspirate allows histological confirmation, with characteristic sheets of plasma cells with eccentric nuclei and perinuclear clear zones (Fig. 7). The specific monoclonal immunoglobulin may be characterized, and several additional biochemical and genetic markers are being used or investigated to offer prognosis and predictions regarding response to therapy. Treatment strategies should be individualized; some milder variations of the disease require no treatment, whereas older or sicker patients may not be able to tolerate aggressive chemotherapy regimens. Multiple myeloma is very sensitive to radiation therapy, and, in patients with spinal cord compression, radiation can rapidly reduce both pain and neurologic symptoms. Autologous stem cell transplantation is the gold standard for patients who can tolerate the associated chemotherapy. There is controversy about whether biopsy is necessary to determine the exact cause of the vertebra plana. Biopsy of the vertebral body is an invasive procedure that risks damage to the vertebral growth plates, which are typically spared by eosinophilic granuloma. Growth plate injury, at least in theory, may hinder reexpansion of the vertebral body in these young patients. However, we found no reported cases of iatrogenic growth plate injury during biopsy. O’Donnell et al. suggested performing open biopsy in suspected cases of eosinophilic granuloma vertebra plana except when a strict set of criteria for observation was met: an age of less than twenty years; no radiating pain or neural compression; no constitutional symptoms or abnormal laboratory findings; and monostotic, symmetric vertebral body collapse with sparing of the posterior elements. However, their review and recommendations predated the widespread use of MRI, which would likely play a role now in the selection of biopsy candidates. More recently, some authors have suggested reserving biopsy for atypical cases in patients with either an associated soft-tissue mass on MRI, involvement of the disc space, or the presence of neurologic symptoms. When biopsy is warranted, there is still no consensus regarding the use of an open or percutaneous technique. Older reports in the literature cited a low diagnostic yield with percutaneous needle biopsy. However, CT-guided needle biopsy is being increasingly advocated in light of more recent reports showing lower morbidity and higher yields than previously reported. Yasko et al. reported 90% accuracy in a cohort of thirty-nine patients, whereas Elsheikh et al. found 100% accuracy in three cases. In conclusion, our adolescent patient with vertebra plana and back pain did not have any atypical clinical or radiographic findings for nearly two years after the onset of symptoms. Our strategy of frequent follow-up with serial imaging is consistent with most contemporary treatment algorithms. Multiple myeloma is exceedingly rare in patients this young, and little is known about its natural history, prognosis, and optimal treatment. The initial workup for vertebra plana should include MRI and a skeletal survey to evaluate for systemic disease or atypical findings as described above. We recommend a strong consideration of CT-guided needle biopsy if there is any suggestion of malignant disease or if the diagnosis is doubtful. If the results of the needle biopsy are inconclusive, open biopsy may be done.
Reference: Greenleaf RM, Ricciardella LF, Latona CR, Sangimino MJ. Vertebra plana in an adolescent caused by multiple myeloma. A case report and review of the literature. J Bone Joint Surg Am. 2011;93:e37(1-7).
Langerhans cell histiocytosis
Multiple myeloma
Leukemia
Amyloidosis



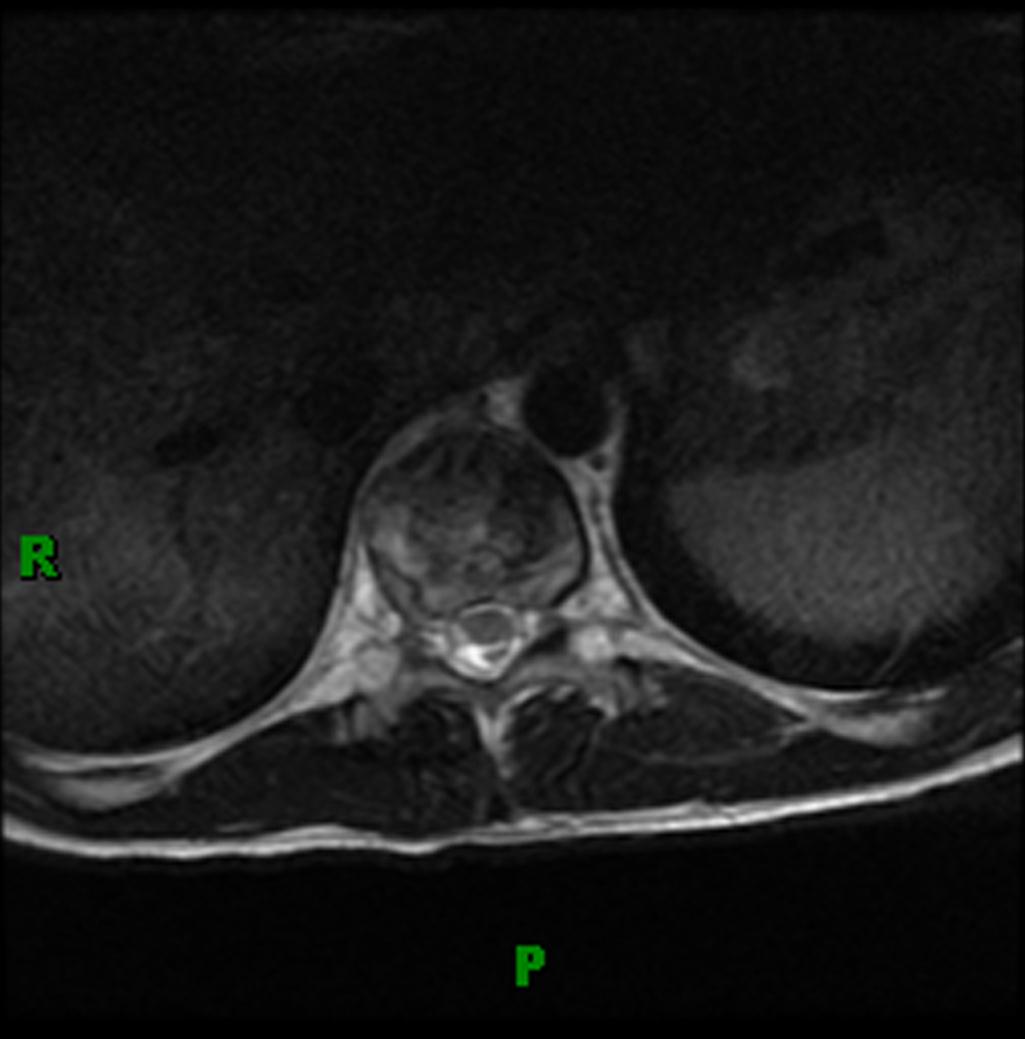

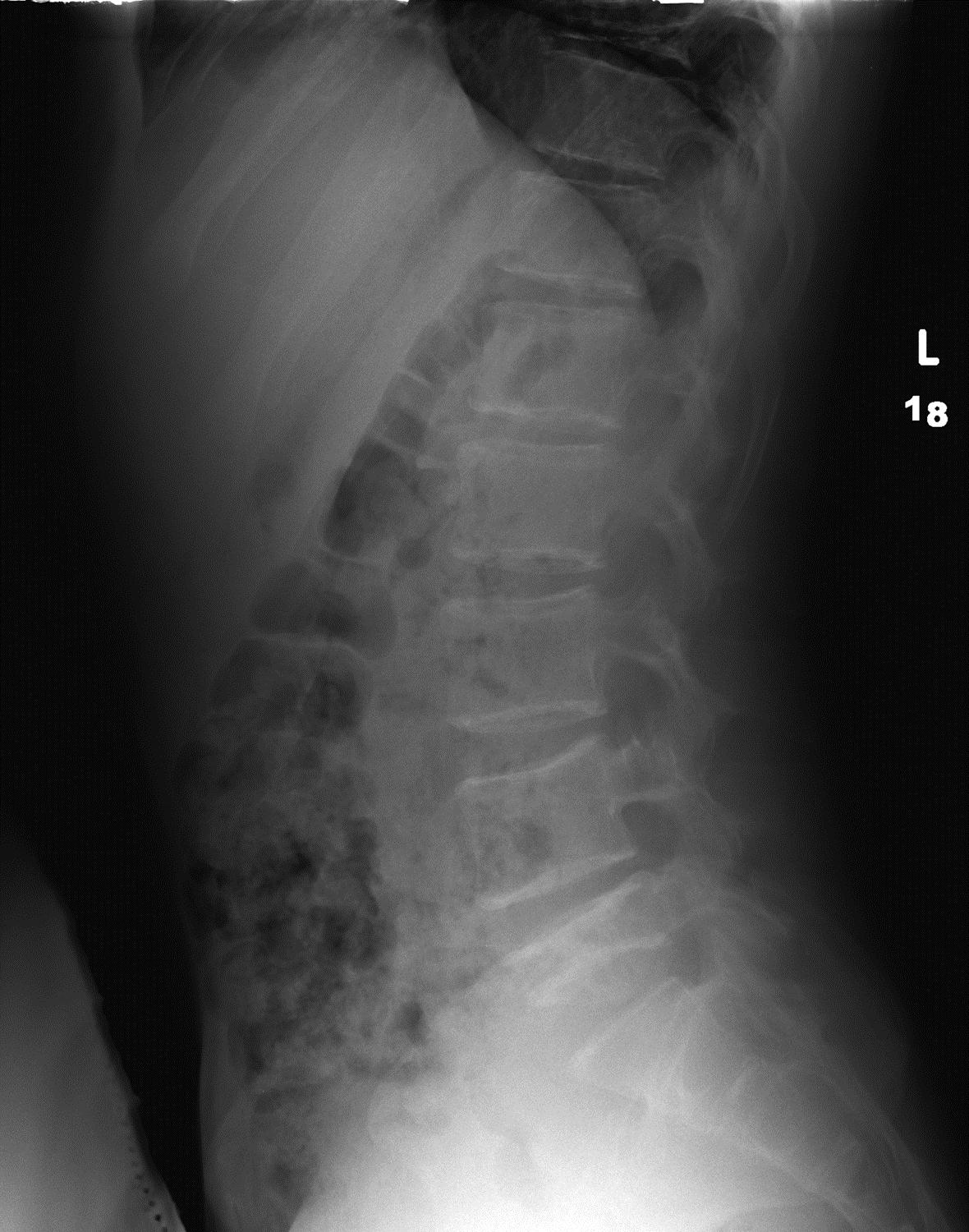

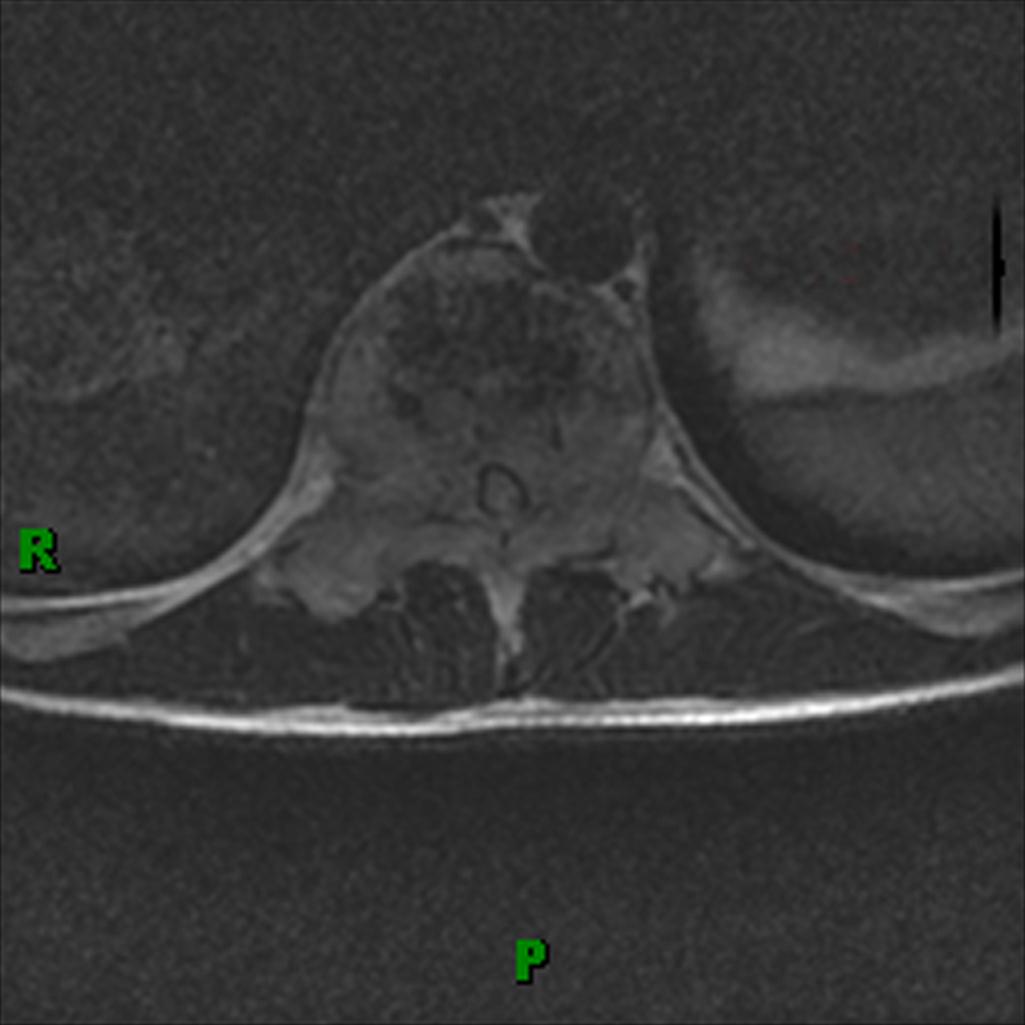
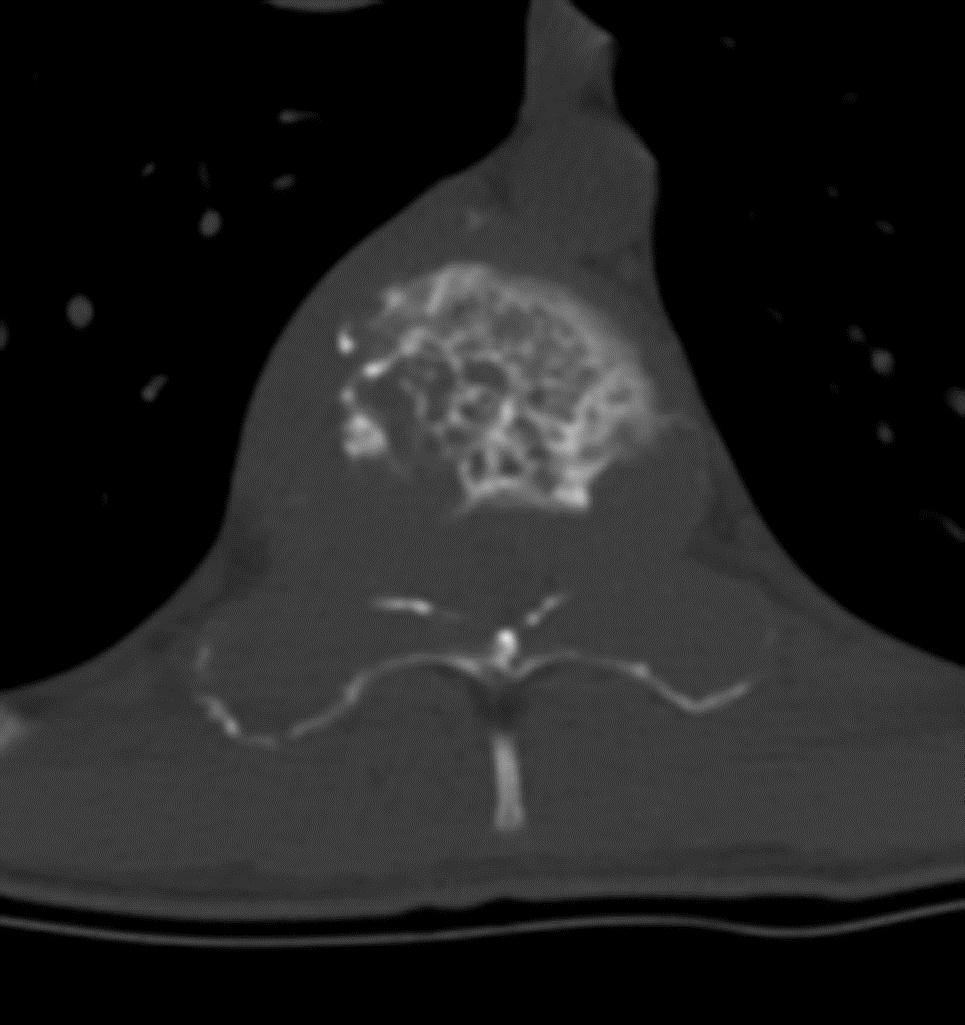
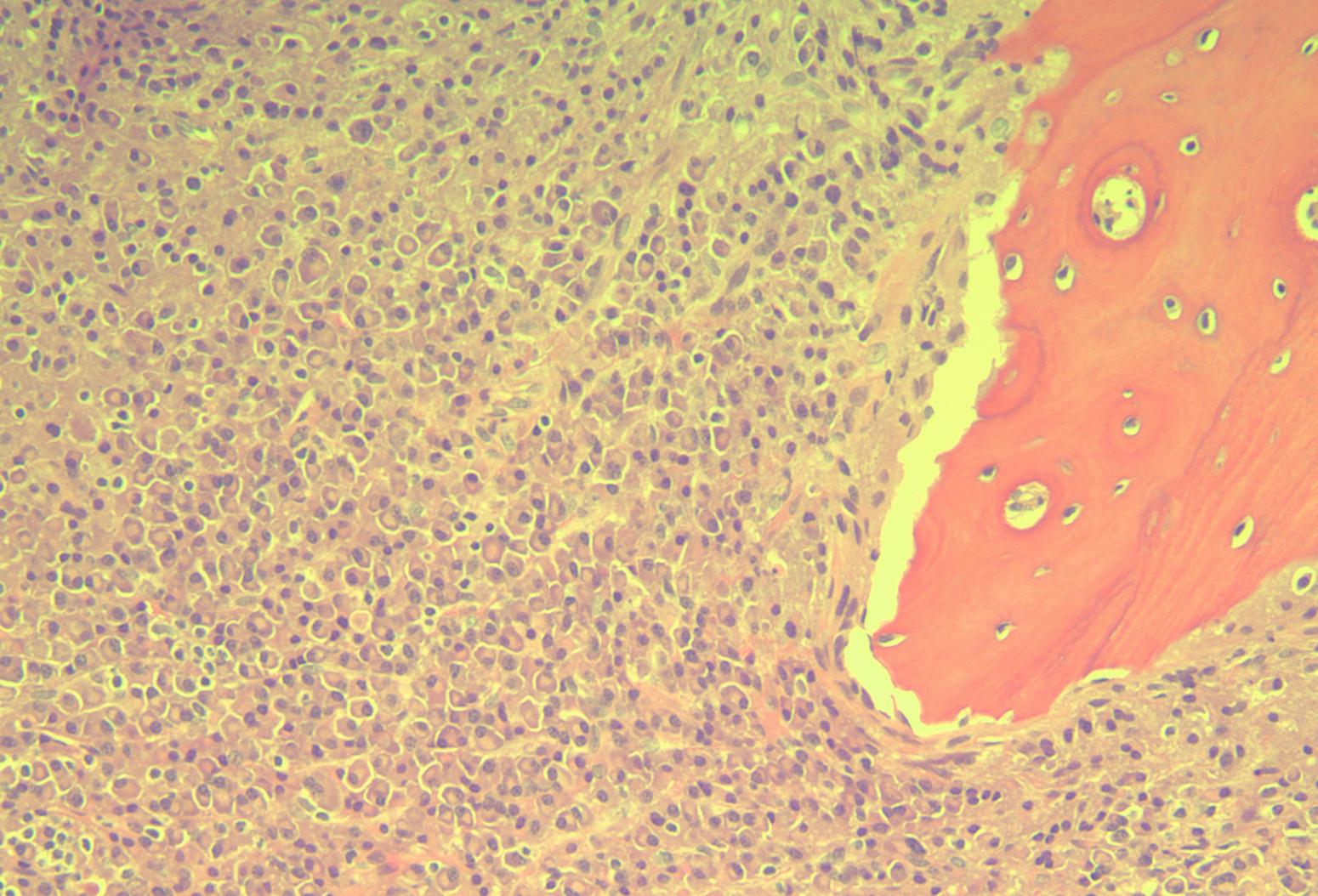
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6-A
Fig. 6-A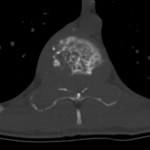 Fig. 6-B
Fig. 6-B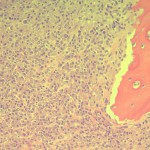 Fig. 7
Fig. 7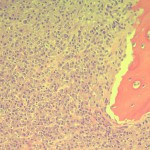 Fig. 7
Fig. 7