A Nine-Year-Old Girl with Left Shoulder Pain and Fever
April 15, 2015
A nine-year-old, right-hand-dominant, female patient presented to the emergency department after having experienced atraumatic left shoulder pain, fevers, and night sweats for one week. Over the course of seven days, the left shoulder pain had progressed to the point of pseudoparalysis and was characterized as a deep, dull, persistent ache without radicular symptoms. The patient did not report any numbness or paresthesia of the left upper extremity. There was no history of arthralgias, cutaneous skin infections, cyclic fevers, or recent travel. No family members had experienced any recent illnesses.
The patient’s only medical history was attention deficit hyperactivity disorder (ADHD), for which she took Adderall (amphetamine and dextroamphetamine). She had no history of any surgical procedures, nor was there a family history of immunodeficiency disorders or bone tumors.
The patient was born in the United States; her parents, both Puerto Rican, had migrated to Pennsylvania fifteen years prior. She lived at home with both parents and three siblings. All of her vaccinations were up-to-date. She was a fourth-grade student at her local elementary school. She reported that she did not use tobacco, alcohol, or illicit drugs, or have any history of physical abuse.
On initial evaluation in the emergency department, the patient was febrile to 41.1°C, with heart rate, 144; blood pressure, 98/48; and oxygen saturation, 97% on room air. An examination of the left upper extremity demonstrated no erythema, induration, or palpable masses about the shoulder girdle. There was diffuse tenderness to palpation over the posterior aspect of her shoulder and scapula. Abduction of the shoulder of >5° was not possible secondary to substantial discomfort. Sensation was intact to light touch over the axillary, median, ulnar, and radial nerve distributions. Motor function of the hand was intact. The patient had a palpable 2+ radial pulse.
Laboratory results showed an elevated white blood-cell count of 21,200/mm3 (21.2 × 109/L) (normal, 4500 to 14,500/mm3 [4.5 to 14.5 × 109/L]), with 84% neutrophils, 5% lymphocytes, 7% monocytes, and 0.0% eosinophils and basophils. Erythrocyte sedimentation rate was 91 mm/hr (normal, 0 to 20 mm/hr) and C-reactive protein, 16.74 mg/dL (normal, 0.05 to 1.00 mg/dL). Blood culture specimens were obtained on the day of presentation and were ultimately negative.
Radiographs of the left shoulder showed no osseous abnormality (Figs. 1 and 2). MRI (magnetic resonance imaging) of the left upper extremity demonstrated a 4.5 × 3.4 × 9.0-cm fluid collection in the subscapular region with multiple septations (Figs. 3 through 6). A smaller 2.5 × 1.2 × 1.0-cm fluid collection superficial to the scapular body was also identified. There was no extension into the chest cavity. There was no bone marrow enhancement, osseous erosion, or mass of the scapula or humerus.
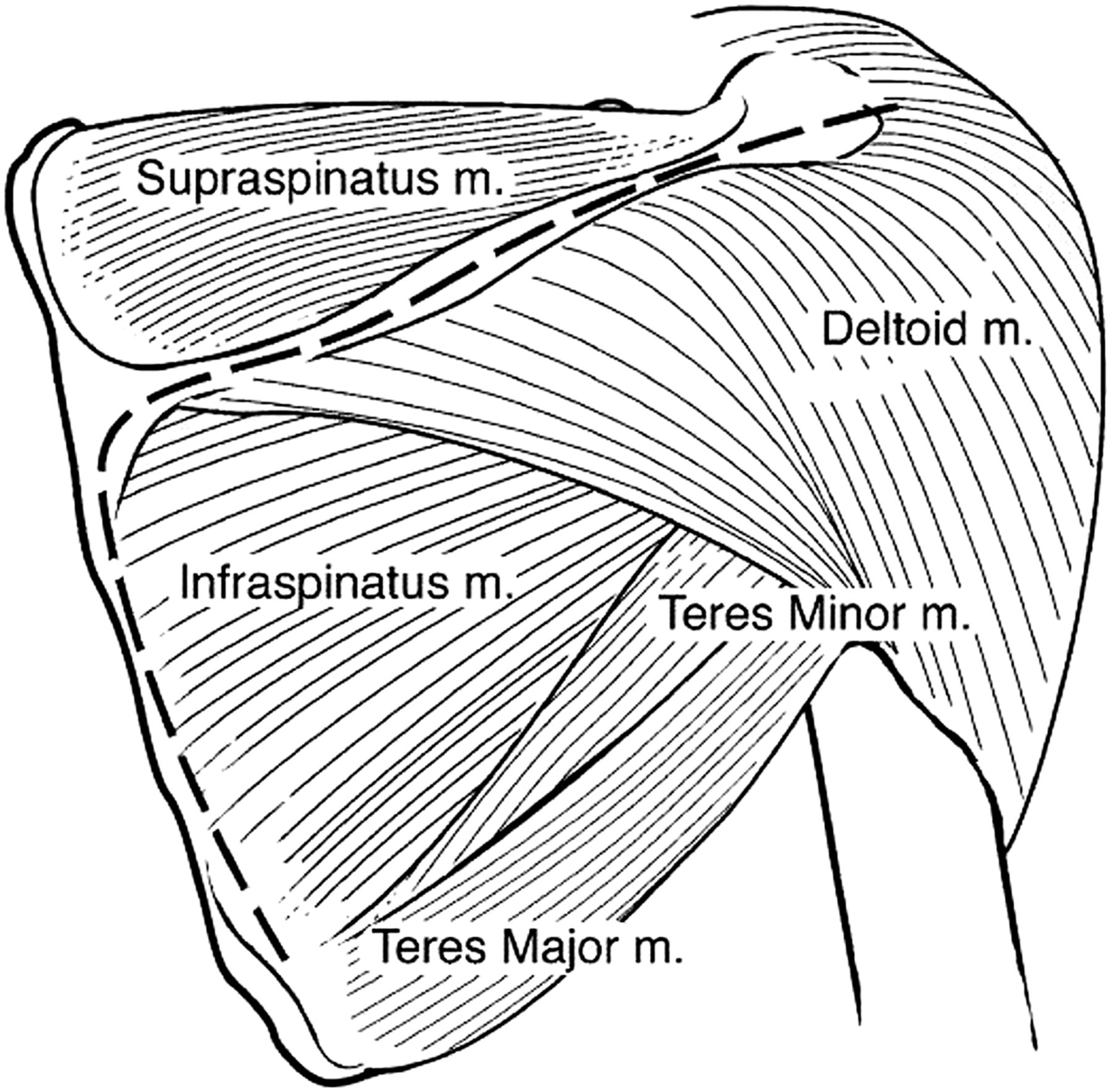
The patient was taken urgently to the surgical suite for irrigation, debridement, and decompression of the periscapular fluid collections. The patient was placed in a lateral decubitus position on her right side. A modified Judet approach to the scapula was utilized. Starting from the posterior lateral aspect of the acromion, an incision was made medially along the scapular spine and then curved 90° in a caudal direction following the medial aspect of the scapular body (Fig. 7). On the inferior aspect of the medial scapular body, 3 cm of the rhomboid major muscle was detached from its insertion (Fig. 8). A curved Kelly clamp was inserted carefully along the anterior aspect of the scapular body through the created window into the subscapular region. A large, 30-mL rush of malodorous, purulent, white, thick fluid was expressed, and a sample was sent for culture. The surgeon’s finger was used to manually debride the remaining loculations of the subscapular fluid collection. The smaller suprascapular abscess was decompressed with a Kelly clamp, and 10 mL of the same purulent fluid was expelled. The area was irrigated with 3 L of bacitracin-injected Ringer lactate solution. A Hemovac drain was placed in the subscapular region. The rhomboid was repaired with PDS (polydioxanone) suture, and the skin was closed with nylon. The patient was extubated and taken to the postoperative care unit in stable condition. Postoperative chest radiograph showed that the patient did not have a pneumothorax and the chest cavity had not been violated during the procedure.
The patient was admitted to the hospital from the recovery room. She was started on vancomycin empirically while culture results pended. Her drain was removed on postoperative day 3. On postoperative day 4, she was noted to have recurrent fever to 39.0°C and continued pseudoparalysis of her left shoulder. In light of these clinical findings, a CT (computed tomography) scan of her left upper extremity was made (the patient refused repeat MRI), and it showed evidence of the reaccumulation of fluid. The patient returned to the operating room, where debridement was repeated with use of the prior incisions. No further purulent fluid was noted, only coagulated hematoma. A Penrose drain was left in place and removed forty-eight hours later with the first dressing change.
Methicillin-resistant Staphylococcus aureus (MRSA) that was sensitive to clindamycin was identified on cultures. Anaerobic and fungal culture results were negative. While common osseous findings of osteomyelitis were not appreciable on MRI, the notable pyomyositis and inflammatory changes surrounding the scapula presented concern for osteomyelitis and appropriately influenced antibiotic selection. A peripherally inserted central catheter was placed, and a twelve-week, intravenous clindamycin regimen was recommended. The patient was discharged to home in stable condition.
By the three-month follow-up, the patient’s symptoms had completely resolved. She had no recurrence of fevers, night sweats, or chills. Her incisions were well healed. She had full, painless range of motion of the left shoulder, and she had returned to her prehospital activity level. All of her inflammatory markers had returned to normal levels.
Proceed to Discussion >>Reference: Giugale JM, Bosch PP, Grudziak JS. Subscapular abscess in a nine-year-old female patient: a case report. JBJS Case Connect. 2015 Feb 11;5(1):e13.
While soft-tissue and skin infections are prevalent, the development of a subscapular abscess is extremely rare, especially in an otherwise healthy pediatric patient. A review of current literature led us to only five other reported cases across all age groups.
In Turkey, a seven-year old male patient presented with fever and shoulder pain three weeks after having fallen off his bike onto his affected extremity. A subscapular abscess was identified on MRI after four days of empiric antibiotics for presumed occult shoulder septic arthritis, despite there being no growth on culture after aspiration. The fluid that had collected was surgically drained. No bacteria could be isolated on intraoperative cultures. The patient went on to complete a three-week parenteral antibiotic course with ceftriaxone and vancomycin and made a full recovery.
Nowinski and Duchene reported a case of a spontaneous subscapular, methicillin-sensitive S. aureus abscess in a fifty-three-year-old male patient who was otherwise healthy. He, too, made a full recovery after ten days of parenteral vancomycin followed by eleven days of oral dicloxacillin (for a twenty-one-day regimen).
Handorf reported the case of a nineteen-year-old male patient who presented to the hospital one week after being struck in the shoulder with a baseball bat. This patient was septic on presentation. S. aureus was identified on sputum, blood, and glenohumeral aspirate cultures. Despite a vigorous intravenous antibiotic regimen, the patient experienced cardiac arrest, was resuscitated, but was pronounced brain dead four days later. An autopsy revealed a large, subscapular abscess of 300 cc.
A subscapular abscess has been found in a patient as young as fifteen months. This patient had a palpable axillary mass. After failed needle aspirations, the patient underwent formal operative debridement and was found to have an 8 × 5-cm abscess deep to the fascia of the axilla extending into the subscapular area. Interestingly, Haemophilus influenzae type B was the causative bacteria.
In Australia, a forty-two-year-old male with poorly controlled diabetes and a history of thoracic-spine osteomyelitis presented with septicemia and, later, was diagnosed with a subscapular abscess after spine MRI acquired while looking for an epidural abscess depicted a 6 × 6-cm loculated fluid collection in the subscapular region. This was surgically drained, and S. aureus was identified on cultures. His antibiotic regimen was narrowed from vancomycin and meropenem to rifampicin and flucloxacillin, for a total six-week antibiotic course. The patient recovered from the illness.
Only two of the above cases occurred spontaneously in the pediatric population. Three of the five cases involved an isolated S. aureus organism. However, the case we present is, to our knowledge, the only spontaneous, pediatric case of a subscapular abscess caused by S. aureus. The diagnosis in this case was confirmed promptly. We describe an effective, safe surgical approach to adequately decompress the subscapular area, which, in combination with an antibiotic regimen tailored to the susceptibilities of the speciated Staphylococcus organism, resulted in the patient’s full recovery within two months.
Several points can be drawn from these reports. First, the differential diagnosis of shoulder pain in a febrile patient should be kept broad. The subscapular region can hold a relatively large amount of fluid and be clinically hidden from a medical provider. MRI is an important tool for diagnosis and preoperative planning. It allows the defining of boundaries of fluid collection and the identification of the extent of periarticular infection for adequate decompression intraoperatively. Second, prompt diagnosis and surgical and medical management can lead to successful outcomes. There is no standard antibiotic regimen for this pathology. Isolating the bacteria and identifying antibiotic sensitivities allows providers to narrow antibiotic coverage appropriately. Lastly, as our case demonstrates, a modified Judet approach provides a safe exposure for thorough debridement of the subscapular region.
Reference: Giugale JM, Bosch PP, Grudziak JS. Subscapular abscess in a nine-year-old female patient: a case report. JBJS Case Connect. 2015 Feb 11;5(1):e13.
What is the diagnosis?
Subscapular bacterial abscess
Rhabdomyosarcoma involving the subscapularis muscle
Hydatid disease of the subscapular space
Subscapular mycobacterial abscess
Tumoral calcinosis



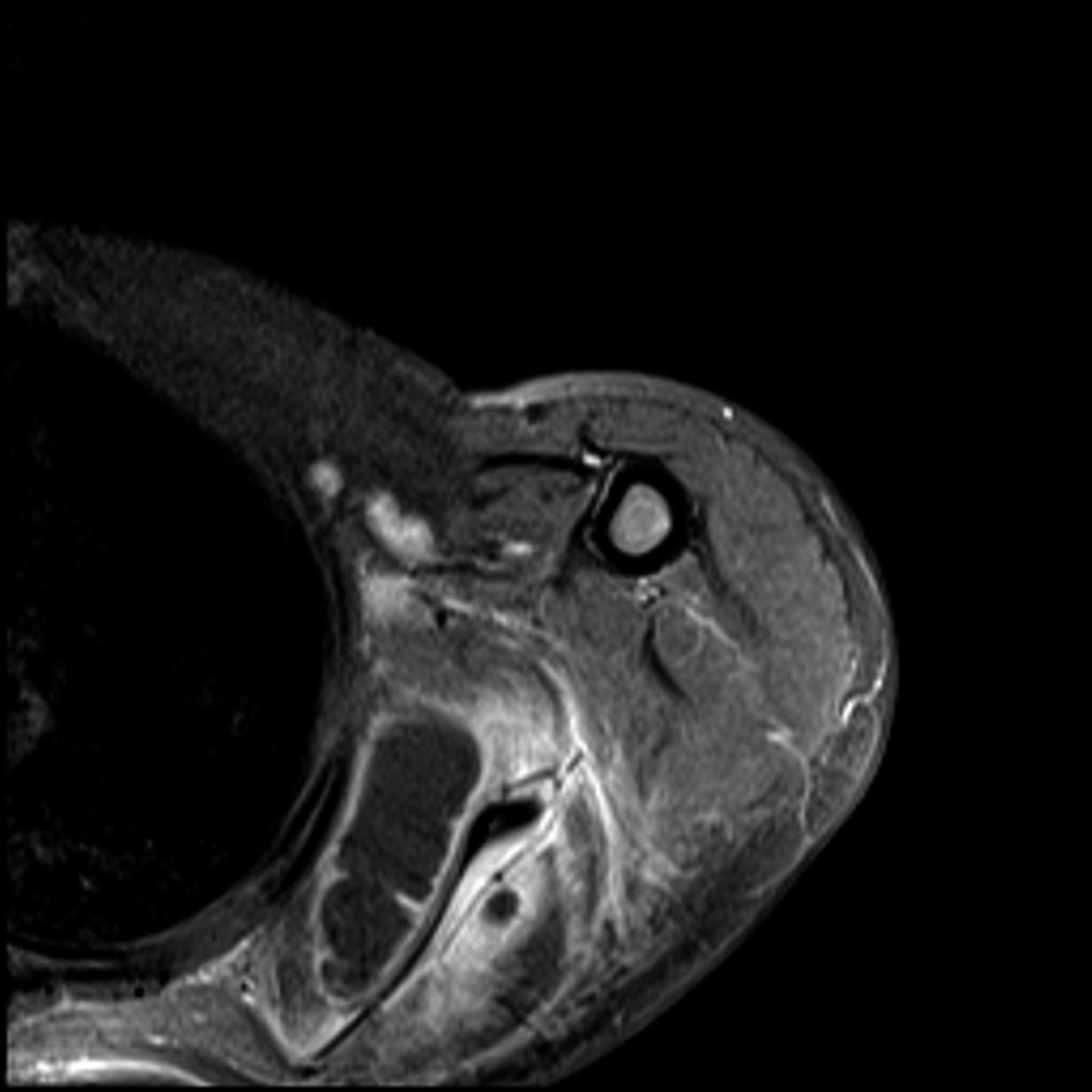

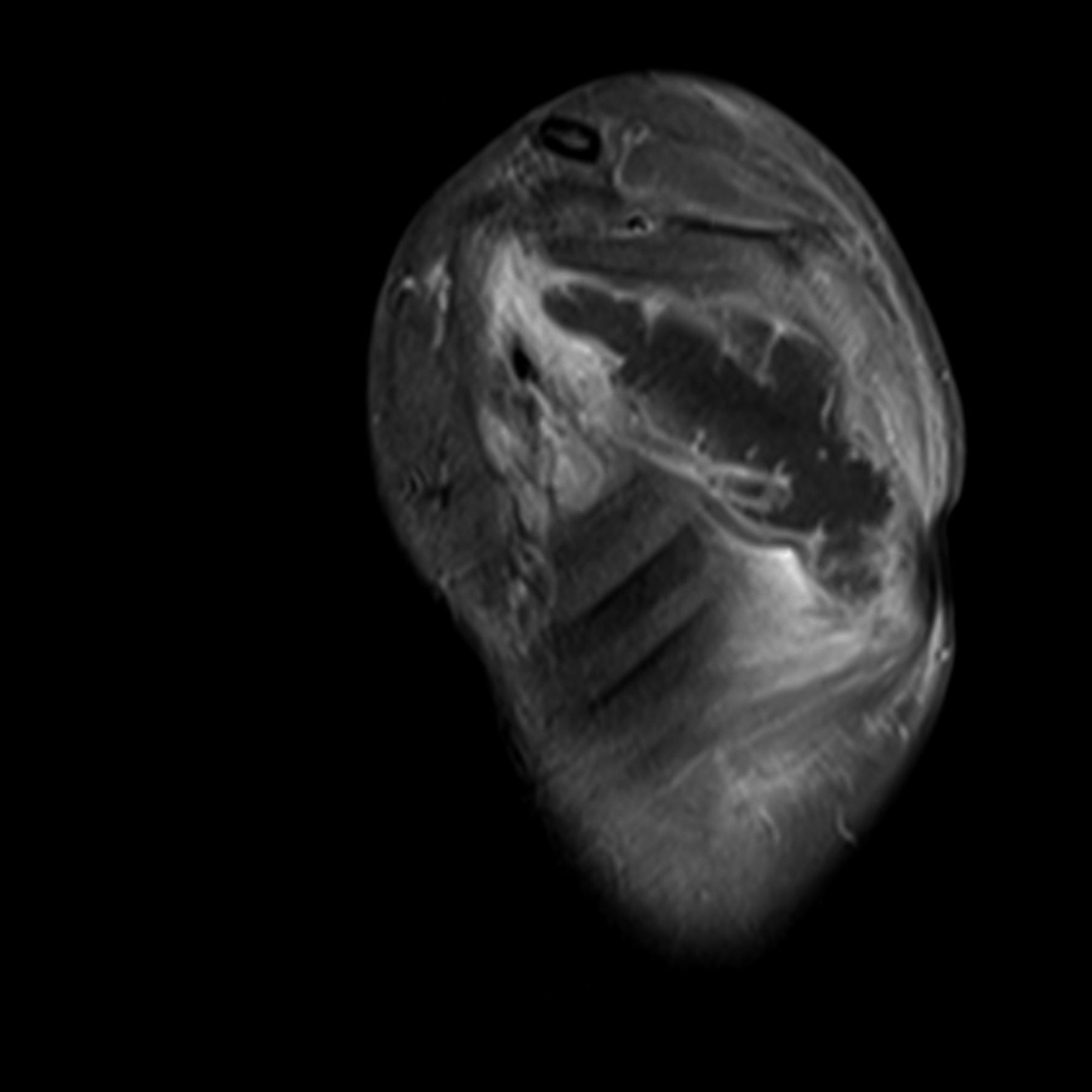
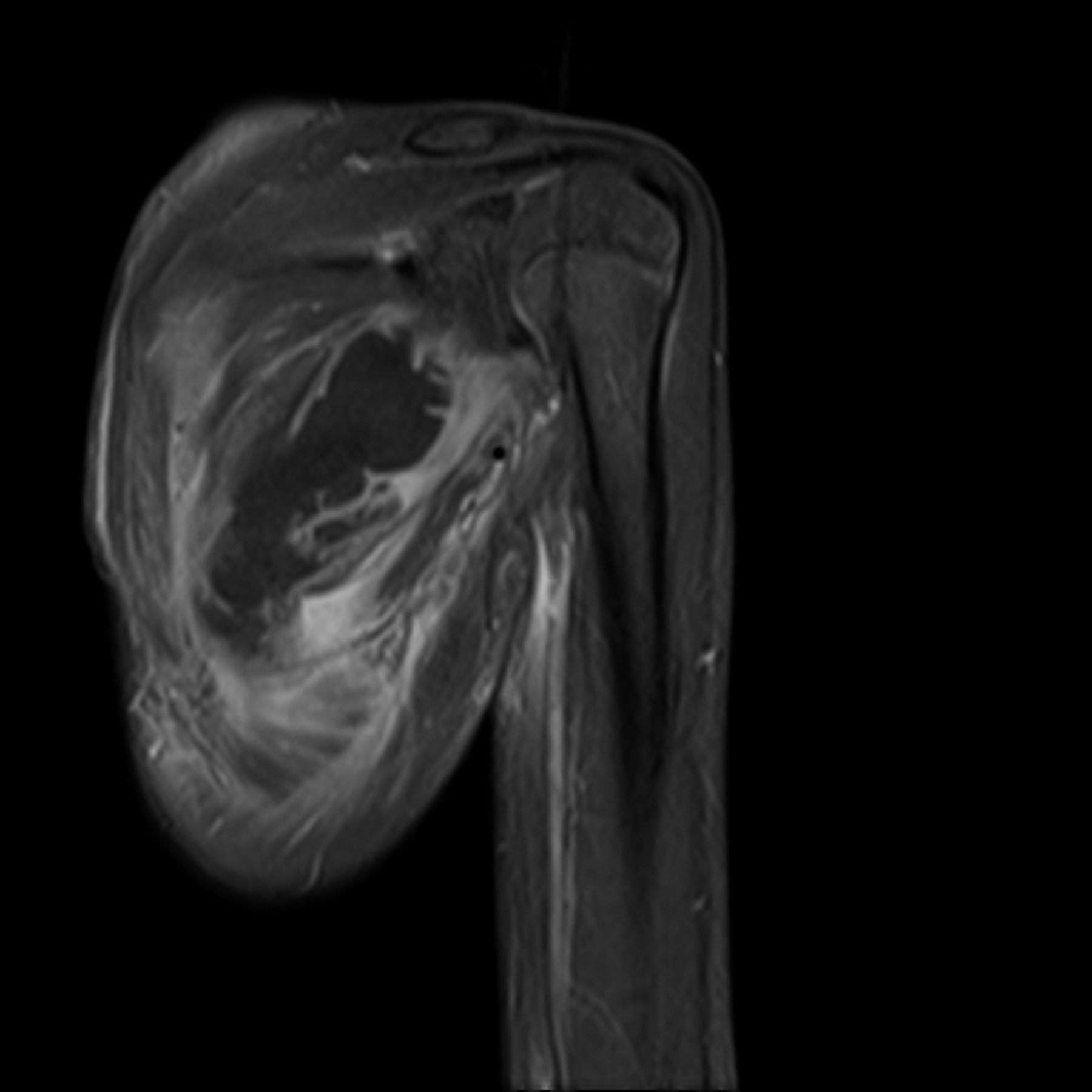
 Fig. 1
Fig. 1 Fig. 2
Fig. 2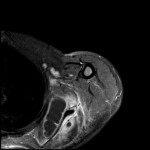 Fig. 3
Fig. 3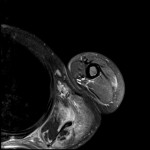 Fig. 4
Fig. 4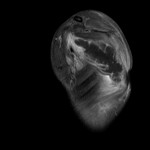 Fig. 5
Fig. 5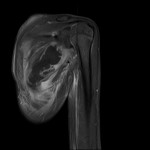 Fig. 6
Fig. 6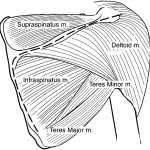 Fig. 7
Fig. 7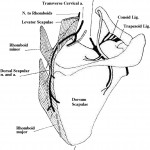 Fig. 8
Fig. 8