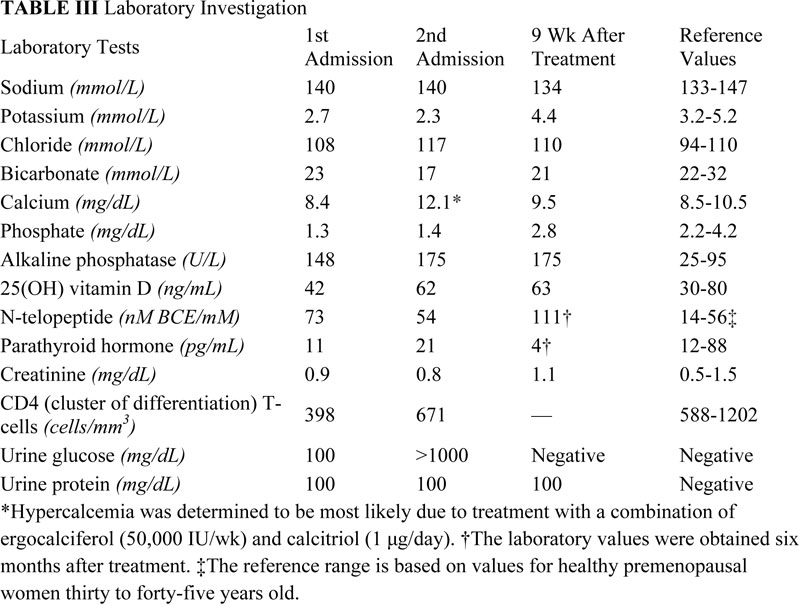
A fifty-four-year-old transgender woman with HIV infection presented with right hip pain after falling at her home. She had experienced increasing difficulty walking for one month and had recently begun using a cane. The medical history included HIV infection and osteoporosis. The HIV infection was well controlled with HIV medications, with normal CD4-positive T-helper cell counts and low-range viral load (<48 copies HIV RNA/mL). In addition to tenofovir and lamivudine/zidovudine for HIV infection, the patient's medications were calcium carbonate, vitamin D, and alendronate (weekly) for osteoporosis. The patient had been taking alendronate for approximately three years prior to this presentation and had not received hormone replacement therapy for over twenty years. Hip examination was painful, but no gross deformity was evident. The contralateral hip was pain-free. Radiographs showed a right basicervical femoral neck fracture (Fig. 1-A). On admission, laboratory findings included hypophosphatemia (phosphate level, 1.3 mg/dL), hypokalemia (potassium level, 2.7 mmol/L), mild hypocalcemia (calcium level, 8.4 mg/dL), and an elevated alkaline phosphatase level (148 U/L) (Table I). Closed reduction and internal fixation of the hip fracture with an intramedullary nail (Trochanteric Fixation Nail; Synthes, West Chester, Pennsylvania) was performed (Fig. 1-B). The patient tolerated the procedure well and was discharged home three days after surgery. Bone mineral density (BMD) evaluation following the fracture revealed a T-score of −3.0 at the lumbar spine. Because the patient had sustained a fragility fracture while on bisphosphonates, it was recommended that she begin teriparatide treatment after her metabolic condition had stabilized (at approximately six weeks following surgery). Approximately two weeks after surgery, the patient had a sudden onset of left hip pain, which progressively worsened over six weeks. The patient denied having had a fall or sustaining trauma preceding the onset of the left hip pain. Clinical symptoms related to the previous right hip fracture had resolved, and postoperative radiography performed at eleven weeks showed a healed fracture in that hip. The patient also described generalized bone pain and severe fatigue that had been progressive for the past four months. She now required the use of a walker to walk. She also noted a 20-lb (9-kg) weight loss since her last hospital admission with decreased appetite, dysphagia, and several episodes of oral thrush. The patient was maintained on medications from the previous admission, with changes made by her primary care physician to increase serum calcium levels with use of ergocalciferol (vitamin D2), 50,000 IU/wk, and calcitriol (active vitamin D3), 1 µg/day. On physical examination, the patient was cachectic with a body mass index (BMI) of 14 kg/m2, exhibited temporal wasting, and was ill-appearing. Examination of the left hip was painful but there was no gross deformity, and her neurovascular status was intact. Radiographs showed no evidence of acute fracture of the left hip (Fig. 2-A). Because of the history of chronic left hip pain for six weeks, magnetic resonance imaging (MRI) of the left hip was done. The T2-weighted MRI showed a hypointense line extending through the intertrochanteric region of the left femur with increased marrow edema, consistent with a complete nondisplaced left intertrochanteric femoral fracture (Fig. 2-B). The T2-weighted MRI study also showed a hyperintense signal at the sacrum without any fracture line, compatible with a left sacral insufficiency fracture, as well as stress reactions within the pubis. The patient was treated for a left intertrochanteric femoral fracture with internal fixation with placement of an intramedullary nail (Trochanteric Fixation Nail) (Fig. 2-C). Following the procedure, laboratory studies revealed a hyperchloremic metabolic acidosis, decreased serum potassium and phosphate levels, and increased urinary losses of glucose and protein (Table II), findings indicative of proximal renal tubular dysfunction, consistent with Fanconi syndrome. Further evaluation for acquired forms of Fanconi syndrome revealed negative findings.
It was determined that none of the patient’s other medications were nephrotoxic and that tenofovir was the most likely cause for her clinical symptoms. The patient remained hospitalized for postoperative rehabilitation and for treatment of Fanconi syndrome. Treatment with the tenofovir was discontinued and replaced with lopinavir/ritonavir. Intravenous repletion of phosphate was initiated and then replaced with oral supplementation. Amiloride use was initiated for hypokalemia, and a high-phosphate diet was recommended. Once tenofovir treatment was discontinued, the patient’s symptoms rapidly improved, with resolution of generalized bone pain and fatigue. The patient responded to electrolyte repletion and was able to walk without any assistive devices. She also had increased weight gain and improved nutritional status. After four weeks of follow-up, the patient had no hip pain. As a result of the patient’s fragility fracture while she was on bisphosphonate (alendronate) therapy, that therapy was stopped, and the patient was started on teriparatide to manage the osteoporosis and to enhance fracture-healing. After approximately nine weeks of follow-up, the electrolyte laboratory values were normal (Table III). After approximately two years of postoperative follow-up, the clinical symptoms were resolved, radiographs showed healed fractures in both hips, and the patient had returned to the functional status that she had had prior to the hip fractures.
Proceed to Discussion >>Reference: Rebolledo BJ, Unnanuntana A, Lane JM. Bilateral pathologic hip fractures associated with antiretroviral therapy. A case report. J Bone Joint Surg Am. 2011;93:e78(1-6).
Patients with HIV infection are at increased risk for osteoporosis and fracture. Brown and Qaqish showed that HIV infection is associated with a 3.7-fold increased risk of osteoporosis compared with noninfected controls, as is fracture prevalence. When the bone remodeling process is shifted toward bone resorption, the result is an imbalance of bone turnover that causes bone loss and patient predisposition to fracture. Yin et al. reported that the association between HIV infection and decreased BMD is mediated by increased bone turnover. While patients with HIV infection exhibit an increased risk of fracture, adverse reactions to commonly prescribed antiretroviral medications can also contribute to fracture risk. Tenofovir, an antiretroviral medication, is classified as a nucleotide reverse transcriptase inhibitor that prevents the action of the enzyme reverse transcriptase needed for HIV viral production. Tenofovir has been associated with an adverse reaction known as Fanconi syndrome, which can lead to osteomalacia. While growing evidence shows an association between tenofovir and abnormalities of bone metabolism, the pathogenesis remains unknown. Tenofovir has been linked to BMD loss, but similar results have been shown with other antiretroviral medications. Low BMD is common in untreated HIV patients, although greater BMD losses are seen in patients on continuous antiretroviral medication. A study by Gallant et al. suggested that antiretroviral treatment with tenofovir can lead to substantial decreases of BMD at the lumbar spine. However, the decrease in BMD at the lumbar spine was not consistent with BMD loss at the hip when compared with that in patients taking other antiretroviral medications. In addition, Calmy et al. showed that, while levels of bone turnover markers were markedly elevated in patients treated with tenofovir, BMD was not significantly decreased after adjustment for HIV-independent risk factors. Tenofovir can lead to renal dysfunction and impaired reabsorptive capacity of the proximal tubules, which can result in severe electrolyte abnormalities. Clinical symptoms of Fanconi syndrome include polyuria, weight loss, anorexia, muscle weakness, and generalized bone pain associated with osteomalacia. Diagnosis is prompted by laboratory detection of hypophosphatemia, hypokalemia, and urinary losses of glucose and electrolytes in the setting of hyperchloremic metabolic acidosis (Table IV). Tenofovir-associated Fanconi syndrome is confirmed by laboratory investigation as well as by reversibility once the medication is stopped. In addition to complications related to Fanconi syndrome, tenofovir may also exert direct effects on bone metabolism. Grigsby et al. proposed a mechanism for tenofovir-associated bone loss by alteration in the regulatory gene expression profiles of osteoclasts and osteoblasts, leading to disruption of the balance between bone resorption and formation, resulting in bone loss. Tenofovir is a phosphonate, structurally comparable with bisphosphonates (diphosphonates), and, by a similar mechanism, could selectively target bone. However, in contrast to bisphosphonates, which prevent bone resorption by osteoclast inhibition, osteoclast uptake of tenofovir could target the cell nucleus, leading to a disruption of DNA synthesis that ultimately affects gene expression and leads to increased bone resorption. Tenofovir-associated Fanconi syndrome remains a rare complication. However, since the first report was published in 2002, a growing number of cases have emerged linking the commonly prescribed antiretroviral medication to renal dysfunction. According to previous reports, the duration of tenofovir treatment prior to development of Fanconi syndrome ranges from four to twenty-six months. However, our patient developed Fanconi syndrome approximately five years after starting tenofovir treatment. She presented to the hospital with a right basicervical femoral neck fracture after a low-energy fall. Diagnosis of tenofovir-associated Fanconi syndrome was delayed until the patient presented again two months later with an occult fracture of the left hip. Clinical symptoms and laboratory investigation indicating severe renal wasting prompted further workup for a secondary cause of fracture. We believe that tenofovir was the causative agent in the development of the Fanconi syndrome that led to fracture complications in this patient. Cessation of tenofovir treatment resulted in rapid alleviation of clinical symptoms and gradual improvement in laboratory values. The patient was not taking any other nephrotoxic medications at the time. On the basis of her low BMD (a lumbar spine T-score of −3.0), we postulated that the fractures were a result of combined osteoporosis and osteomalacia. Although the patient was maintained on bisphosphonate therapy for osteoporosis, the efficacy of alendronate in nonvertebral fracture risk reduction was shown to be 27% after three years of treatment. In addition, approximately 15% of patients taking alendronate do not respond to that therapy despite adherence to treatment for over two years. While estrogen treatment has been shown to increase BMD in male-to-female transgender patients, the patient in this report was not maintained on hormone replacement therapy. The lack of sex hormones in transgender male-to-female patients not maintained on hormone replacement therapy may result in hypogonadal states. As previously reported, the effects of male hypogonadism have been shown to cause bone loss. We acknowledge that osteoporosis likely contributed to both hip fractures in this patient. The development of osteoporosis was likely multifactorial, related to the HIV infection, hypogonadal state, and antiretroviral treatment, which could have all contributed to bone loss. However, the symptomatic drug reaction causing Fanconi syndrome, which led to hypophosphatemic osteomalacia, further increased the risk of fragility fracture. A limitation of this report is that no bone biopsy was performed to confirm the diagnosis of hypophosphatemic osteomalacia. Similar to previous reports of tenofovir-associated Fanconi syndrome, a diagnosis was made based on clinical and laboratory features consistent with hypophosphatemic osteomalacia. While no bone biopsy was performed, MRI preceding the second surgery also demonstrated sacral insufficiency fractures and stress reactions within the pubis, which are changes consistent with osteomalacia. To our knowledge, this is the first report to describe bilateral pathologic hip fracture secondary to tenofovir treatment. Previous cases of tenofovir-associated Fanconi syndrome with reported bone abnormalities have included symptoms of generalized bone pain and multiple microfractures. Brim et al. described an HIV-positive patient with multiple atraumatic rib fractures and pelvic fracture due to tenofovir-associated Fanconi syndrome. In all previous reports, the development of hypophosphatemic osteomalacia and renal tubular dysfunction secondary to tenofovir was reversed after the medication was stopped. Wanner et al. described preexisting renal damage and concomitant therapy with other antiretroviral medications as possible mechanisms of nephrotoxicity linked to tenofovir-associated Fanconi syndrome. While clinical trials have demonstrated long-term safety with tenofovir treatment, incidental findings of increased alkaline phosphatase levels and hypophosphatemia have been noted. Factors that place the HIV-positive patient at higher risk for tenofovir-associated Fanconi syndrome include low BMI, concurrent use of nonsteroidal anti-inflammatory drugs (NSAIDs), and combination therapy with other antiretroviral medications, such as ritonavir, which may increase renal toxicity. Patients with HIV infection typically present to orthopaedic surgeons with an acute fracture. While management in the acute setting may include surgical and nonsurgical treatment, comprehensive evaluation of these patients is also important to prevent subsequent fracture. Awareness of antiretroviral drug complications is important to prevent conditions that can lead to metabolic bone disease. In combination with a clinical history, monitoring of serum calcium, phosphate, bicarbonate, creatinine, glucose, and 25(OH) vitamin-D levels should be included in the evaluation of all HIV patients taking antiretroviral medications. Measurement of bone turnover markers should also be considered, with the goal of maintaining levels within a normal reference range. Urinalysis also aids in the detection of early renal tubular reabsorption abnormalities in tenofovir-treated patients. As patients with HIV infection continue to live longer with use of currently available medication regimens, the complications of antiretroviral medications may continue to increase in prevalence. Careful evaluation of patients with HIV infection and awareness of adverse drug complications can help in the evaluation and prevention of fractures in these patients.
Reference: Rebolledo BJ, Unnanuntana A, Lane JM. Bilateral pathologic hip fractures associated with antiretroviral therapy. A case report. J Bone Joint Surg Am. 2011;93:e78(1-6).
Alendronate
Excessive vitamin D
Tenofovir
Excessive calcium carbonate

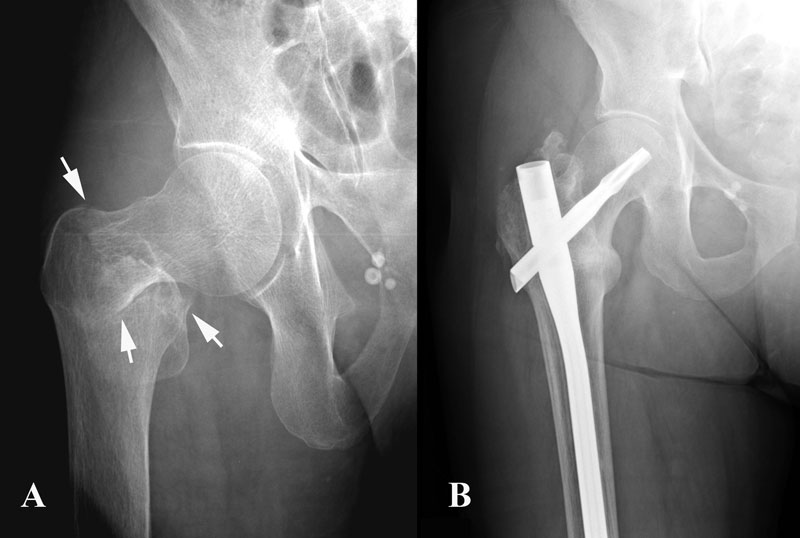
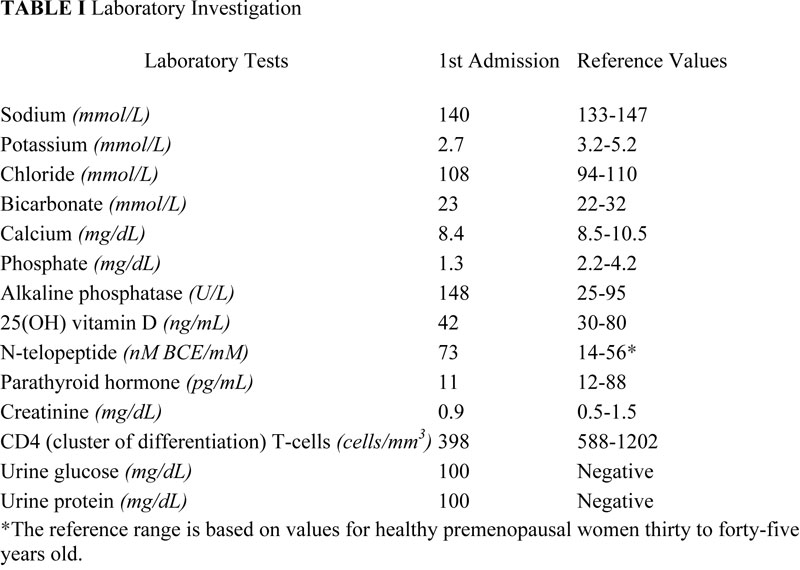

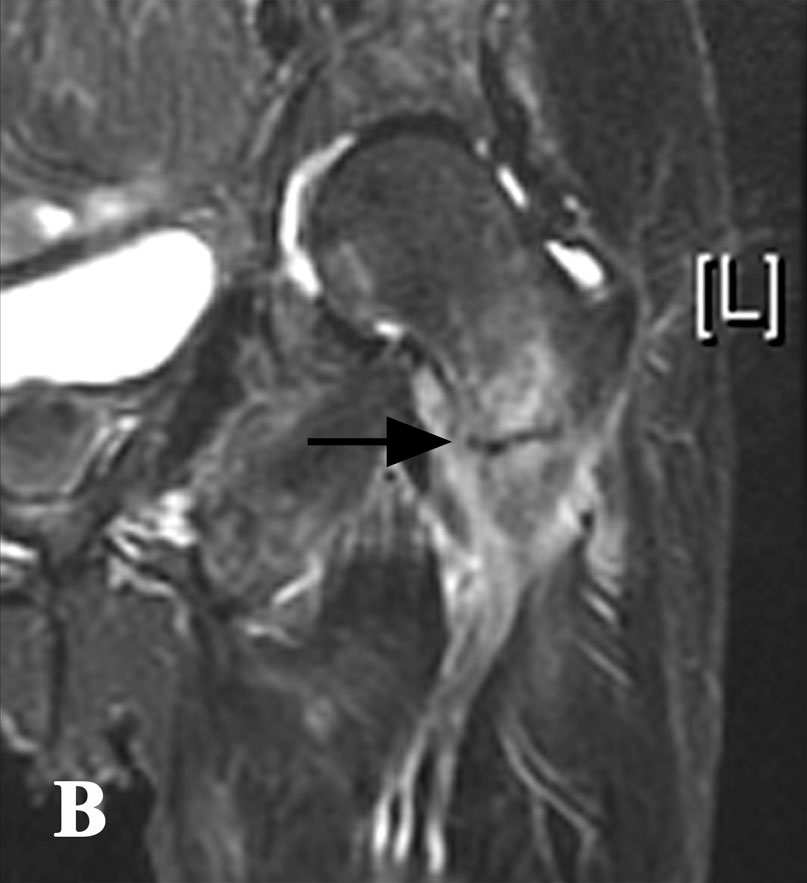

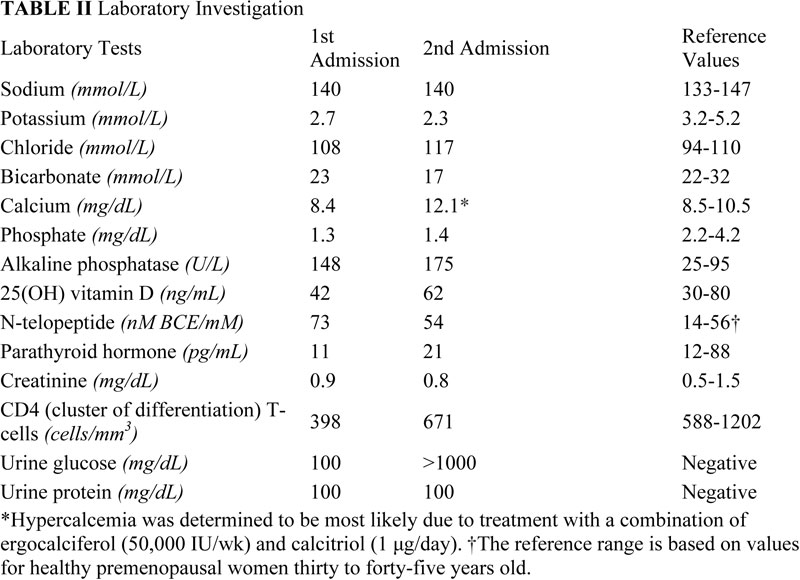
 Fig. 1
Fig. 1 Table I
Table I Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 2-C
Fig. 2-C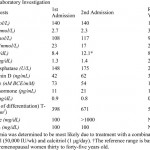 Table II
Table II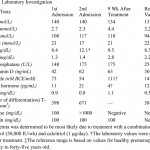 Table III
Table III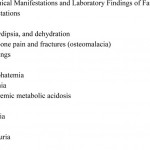 Table IV
Table IV