A Fifty-six-Year-Old Woman with Renal Failure and Neck Pain
March 7, 2012
A fifty-six-year-old woman with end-stage renal disease, secondary to kidney cysts, had been treated with maintenance hemodialysis for two years prior to presentation to us. She had developed neck pain, radiating into the right arm, which slowly worsened over a period of six months. One month prior to presentation, she developed a progressive spastic gait disturbance and motor dysfunction. Neurological examination demonstrated right deltoid and biceps muscle weakness (3/5 on manual muscle testing [MMT]), decreased sensation to pinprick in both upper extremities, hyperreflexia in both lower extremities, and a Hoffmann reflex bilaterally. Lateral cervical spine flexion-extension radiographs demonstrated cervical spondyloarthropathy with vertebral body degeneration, and a dynamic spondylolisthesis at the C4-C5 level (Fig. 1-A and Fig. 1-B). T2-weighted sagittal magnetic resonance imaging (MRI) showed spinal cord compression at the C4-C6 level (Fig. 1-C).
Circumferential reconstructive cervical spinal surgery, consisting of posterior stabilization of the C4-C6 spinous processes with polyethylene tape and anterior C5 corpectomy and fusion with use of an iliac crest autograft, was performed. The patient received 1 g of intravenous cephazolin sodium preoperatively and for forty-eight hours after surgery. She remained intubated in the intensive care unit (ICU) after the operation. She was moved out of the ICU after successful extubation on postoperative day one. On postoperative day two, she began oral feeding and walking with physical therapy. Immediately after surgery, the patient experienced marked improvement in her hand numbness and gait disturbance as well as complete resolution of her neck pain. However, on postoperative day four, she began to experience abdominal pain and mild diarrhea. Unfortunately, Clostridium difficile titers were not obtained. She had neither fever nor emesis. Laboratory studies revealed leukocytosis, with a white blood cell (WBC) count of 20,610 cells/mm3. A computed tomography (CT) scan of the abdomen and pelvis demonstrated mucous-membrane thickening and edema of the entire colon (Fig. 2). A colorectal surgeon was consulted; since the diagnosis was uncertain, conservative management was recommended. However, the patient's condition changed suddenly on the night of postoperative day four. She developed hypotension (blood pressure, 69/42 mm Hg), tachycardia (heart rate, 120 bpm), and an elevated WBC count (47,480 cells/mm3). Despite aggressive medical therapy and supportive care, her condition deteriorated rapidly. She developed septic shock and respiratory failure that required intubation, and she died on postoperative day five. The family consented to an autopsy, which revealed widespread pseudomembranes in the colon (Fig. 3-A and Fig. 3-B). Histological examination showed extensive, severe, acute pseudomembranous colitis with acute cryptitis, crypt abscesses, and mucosal ulceration, consistent with C. difficile colitis (Fig. 3-C). The findings on polymerase chain reaction (PCR) testing of DNA extracted from mucosal debris were positive for C. difficile toxin B (Fig. 4).
Proceed to Discussion >>Reference: Ohba T, Ebata S, Ando T, Ichikawa J, Clinton D, Kondo T, Haro H. Fulminant Clostridium difficile colitis after surgical treatment of cervical destructive spondyloarthropathy. A case report. JBJS Case Connect. 2011;01:e2.
Destructive spondyloarthropathy in the cervical spine was, we believe, first reported as a serious complication of hemodialysis by Kuntz et al. in 1984. The radiographic characteristics of destructive spondyloarthropathy include intervertebral disc-space narrowing with destructive changes involving the adjacent vertebral end plates or vertebral bodies, in the absence of substantial osteophyte formation. Destructive spondyloarthropathy occurs most commonly in the cervical spine. This often results in progressive instability and neurological deficits, requiring surgical decompression and stabilization. There is a paucity of publications on the surgical outcomes in patients with destructive spondyloarthropathy complicated by chronic hemodialysis. On review of the literature, we identified eighteen deaths after ninety-nine surgical procedures for cervical spondyloarthropathy in hemodialysis patients. Eight patients died within the first postoperative month from various complications: cardiovascular arrest (four patients), hypocoagulation disorders (hematoma, bleeding) (two patients), acute pulmonary edema (one patient), and sepsis (one patient). To the best of our knowledge, this is the first case of fulminant C. difficile colitis (FCDC) in a patient who underwent orthopaedic spinal surgery. The risk of mortality is high after surgery for destructive spondyloarthropathy of the cervical spine complicated by chronic hemodialysis. Additionally, as occurred in our case, an unexpected coexisting illness can develop in the perioperative period. C. difficile is an anaerobic, gram-positive bacillus that can produce two exotoxins (Fig. 3-A and Fig. 3-B) and can cause pseudomembranous colitis in susceptible patients. Over the past few years, there has been an increase in the incidence of C. difficile infection (CDI). This has been attributed to an increasingly complicated patient population with multiple comorbidities, more frequent use of broad-spectrum antibiotics, and the presence of new hypervirulent strains of C. difficile. The three major risk factors for infection with C. difficile include antibiotic exposure, advanced age, and hospitalization. A recent study suggested that hemodialysis and ICU admission are also risk factors for CDI. Our patient received 1 g of intravenous cephazolin sodium preoperatively and for forty-eight hours after surgery to prevent surgical infection. She had additional risk factors for developing CDI, including her ICU admission and treatment with chronic hemodialysis. The clinical presentation of CDI varies, ranging from mild diarrheal illness to FCDC, which leads to multiple organ failure and requires prompt surgical intervention and intensive therapy. It is estimated that CDI occurs in up to 8% of hospitalized patients; up to 1% to 3% of these patients progress to FCDC. Although progression to FCDC is an uncommon occurrence, it accounts for the most serious complications, including bowel perforation and toxic megacolon, and is associated with a high mortality rate. Recent reports have indicated that leukocytosis (WBC >16,000 cells/µL), recent operative treatment, and a history of inflammatory bowel disease are risk factors for the development of FCDC; our patient had all of these risk factors. In the treatment of CDI, it is crucial to identify patients early in their disease course before they progress to FCDC and organ failure. It is generally accepted that development of abdominal signs with evidence of C. difficile titers warrants emergency surgery. Our case taught us that it is necessary to suspect CDI in this situation and to obtain C. difficile titers immediately if a hemodialysis patient develops diarrhea or abdominal symptoms.
Reference: Ohba T, Ebata S, Ando T, Ichikawa J, Clinton D, Kondo T, Haro H. Fulminant Clostridium difficile colitis after surgical treatment of cervical destructive spondyloarthropathy. A case report. JBJS Case Connect. 2011;01:e2.
Hemodialysis
Occult tuberculosis disc infection
Vertebral osteomyelitis from gram-negative organism
Degenerative disc disease from old compression fracture secondary to osteoporosis

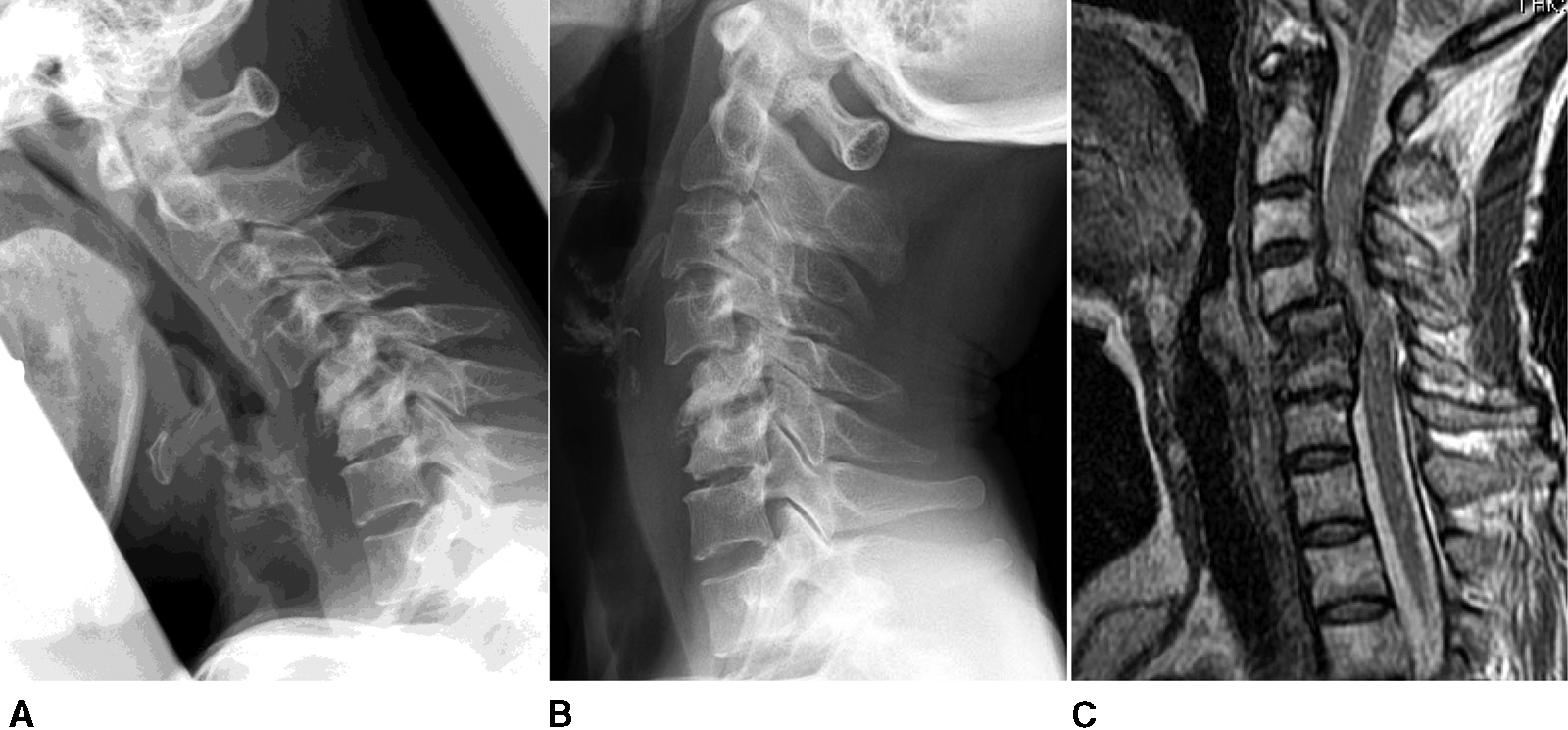
 Fig. 1
Fig. 1 Fig. 2
Fig. 2![Fig. 3 Fig. 3 Autopsy specimen of the entire colon (Fig. 3-A) and close-up view (Fig. 3-B) revealed widespread pseudomembranes in the colon (arrow). Histological findings (hematoxylin and eosin [HE] stain) revealed extensive, severe, acute pseudomembranous colitis with acute cryptitis, crypt abscesses, and mucosal ulceration, consistent with C. difficile colitis (Fig. 3-C).](https://quiz.jbjs.org/wp-content/uploads/2012/03/iqmar12-1_fig3-5-150x150.jpg) Fig. 3
Fig. 3 Fig. 4
Fig. 4

