A fifty-nine-year-old man was involved in a motorcycle crash when he lost control and struck a utility pole. He sustained multiple injuries, including a Gustilo-Anderson grade-II open right femoral fracture, a Gustilo-Anderson grade-IIIA open left femoral fracture (Figs. 1 and 2), a Schatzker-I closed right tibial plateau fracture, and a closed left stellate patellar fracture. He was seen in the emergency department of our academic medical center and was resuscitated according to Advanced Trauma Life Support (ATLS) guidelines. The on-call orthopaedic surgery resident was present for the evaluation of the above-detailed injuries. Prophylactic cefazolin and gentamicin were given in the emergency department, but no tetanus toxoid was administered as the patient had received a tetanus toxoid booster within the previous five years. Once the patient was deemed medically stable to undergo surgery, he underwent debridement of the right and left open femoral fractures in the operating room. Contamination of the proximal fracture fragment of the left femur was noted intraoperatively, and three million units of penicillin were given. The right femoral fracture was treated with retrograde intramedullary nail fixation (Synthes USA, West Chester, Pennsylvania). Given the bone contamination of the left femur, the left femoral fracture was preliminarily treated with external fixation. The tibial plateau and patellar fractures were not addressed surgically in the initial operative setting. Postoperatively, the patient was monitored in the step-down intensive care unit by the multidisciplinary trauma surgery team. He received intravenous (IV) cefazolin and gentamicin for forty-eight hours postoperatively. On the second postoperative day, the surgical dressing was removed and external fixator pin care was instituted according to hospital protocol. The orthopaedic trauma service formulated a plan of delayed treatment of the right tibial plateau fracture and left patellar fracture as well as removal of the left femoral external fixator and conversion to intramedullary fracture fixation. Eight days later, the patient returned to the operating room for planned definitive treatment of all fractures. Once sutures around the pin sites were removed, purulent drainage was noted. The plan for intramedullary fixation of the left femoral fracture was abandoned at that time, and excisional debridement of the pin tracks was performed. Culture specimens were obtained, and the antibiotics were changed to vancomycin, piperacillin/tazobactam, and levofloxacin for broad-spectrum prophylaxis. A repeat debridement was performed forty-eight hours later. Forty-eight hours after the second debridement, the patient returned to the operating room for planned definitive treatment. There was no evidence of active infection in any wound. The external fixator was removed, and the left femur was reamed with the Reamer/Irrigator/Aspirator (RIA) (Synthes USA). A retrograde, locked intramedullary nail (Synthes USA) was placed. We then treated the left patellar and right tibial plateau fractures using open reduction and internal fixation. The immediate postoperative course was uncomplicated, and antibiotic therapy was discontinued forty-eight hours after the final surgical procedures. Three days after the last surgical procedures, the patient developed diplopia and, one day later, he started to develop dysphagia, which worsened to the point of no oral intake. A fiber-optic endoscopic evaluation of swallowing (FEES) was performed by a speech-language pathologist and revealed “severe oropharyngeal dysphagia characterized by reduced tongue base retraction, delayed swallow initiation, reduced pharyngeal squeeze, laryngeal excursion, epiglottic inversion, and UES [upper esophageal sphincter] function.” Given these findings, we requested a consultation from our neurology service. Additional findings on neurological review included hoarse voice, dry mouth, and mild right arm weakness. The patient was not observed to have any autonomic instability. Neurological examination revealed an inability to fully abduct the eyes, mild facial and neck flexor weakness, and moderate tongue weakness. He had mild weakness of the deltoid muscle bilaterally (more on the right than on the left); otherwise, arm strength was normal. Deep tendon reflexes were normal in the arms and trace at the knees. The results of sensory examination of the upper extremities were normal. Given the recent trauma, a dissection of the vertebrobasilar system was considered; however, the results of magnetic resonance imaging (MRI)/magnetic resonance angiography (MRA) were unrevealing. Electromyography and nerve conduction studies (EMG/NCS) were performed. Motor amplitudes were normal. With repetitive nerve stimulation (RNS) at a slow rate (3 Hz), there was a mild decrement in the area of the facial nerve (14.8%; normal, 10%) following one minute of exercise. Movement artifact obscured results when RNS was done at fast rates in the facial nerve. The results of RNS of the radial nerve at slow rates were normal. There was no increment in the facial compound muscle action potential following ten seconds of exercise. Single-fiber EMG (SFEMG) of the orbicularis oculi showed a modest increase in the mean jitter (40.80 µsec; normal for age, 38 µsec).
The results of these tests were consistent with a neuromuscular junction disorder, although not clearly with a presynaptic disorder. The consulting neurologist thought that, although the results of the EMG/NCS testing were somewhat equivocal, the clinical picture fit best with wound botulism. A review of the intraoperative cultures, which had incubated for eight days, showed “Clostridium species, not perfringens” on both anaerobic specimens. Negative inspiratory force (NIF) on the day of the EMG was −30 cm H2O (normal, more than −80 cm H2O). Our working diagnosis at this point was wound botulism with resulting weakness of cranial nerve-innervated muscles and muscles of respiration and mild proximal arm weakness. After consultation with our infectious diseases department, the patient was treated with heptavalent botulinum antitoxin obtained from the Centers for Disease Control and Prevention (CDC). Once the antitoxin had been administered, antibiotic treatment was restarted with piperacillin/tazobactam. Over the course of the following days, the patient’s symptoms stabilized but were not resolving. NIF a week following the administration of the antitoxin was −50 cm H2O. A percutaneous endoscopic gastrostomy (PEG) tube was placed for nutrition, and he was transferred to an inpatient rehabilitation unit for continued therapy. After a two-week course of intensive rehabilitation, he was transferred to a transitional care unit for continued physical and occupational therapy for an additional three weeks prior to discharge home. At the time of writing, the patient was doing well. He had full cranial nerve function and normal vision. He had resumed a normal diet, and his PEG tube had been removed. He continued to progress in outpatient physical therapy. Radiographs obtained six months after surgery demonstrated healed fractures in the right femur, right tibial plateau, and left patella. There was some concern about the delayed union of the left femur, but interval fracture callus formation was seen radiographically. The patient had no symptoms in the left thigh.
Proceed to Discussion >>Reference: Reynolds KA, Young DR, Bariola JR, Stacy A. Rudnicki SA, Gruenwald JM. Bilateral open femoral fracture complicated by wound botulism. A case report. JBJS Case Connect. 2011;01:e3.
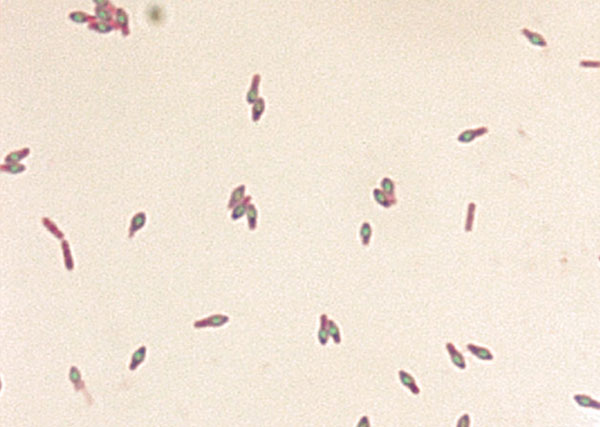
C. botulinum (Fig. 3) is a spore-forming, gram-positive bacillus that grows in anaerobic conditions. It is frequently found, along with other Clostridium species, in soil, but it is most commonly considered a contaminant of poorly sterilized canned foods. C. botulinum produces a potent neurotoxin that results in the presynaptic blockade of acetylcholine. This results in paralysis of both the respiratory and the skeletal muscles. The pattern of paralysis usually begins in the cranial nerves and progresses to involve skeletal muscle. Parasympathetic blockade may result in dry mouth, bowel and bladder dysfunction, tachycardia, and hypotension. Foodborne botulism is caused by the consumption of the toxin, often from contaminated canned goods. Likewise, infantile botulism may be associated with neurotoxin consumed through honey or other contaminated foods. In many cases of infantile botulism, a source is never definitively identified. Wound botulism is unique in that the toxin is formed by bacterial spores that infect the wound and is released after bacterial cell death. Wound botulism is rarely associated with trauma or surgery; it is more commonly seen with parenteral and intranasal drug abuse. Regardless of the mechanism of infection, the clinical effects can be devastating. The most recent data released by the CDC detailed 121 cases of botulism reported in 2009. Of these cases, eleven were foodborne, eighty-four were infantile, twenty-three were wound botulism, and three were due to an unknown etiology. Further review of these statistics shows that twenty-one of the twenty-three cases of wound botulism were caused by injection drug use and were all located along the Pacific Coast. Review of the data from 2005 to 2009 revealed 141 total cases of wound botulism reported to the CDC. Only seven of those cases were not related to IV drug abuse. Interestingly, there were no cases of wound botulism reported in our state, Arkansas, between 2001 and 2009. Shapiro et al. cited the transition to the use of black tar heroin produced in Mexico as a cause for the increase in wound botulism in IV drug abusers. Of the two cases of wound botulism in 2009 not associated with IV drug use, one was associated with abdominal surgery and one was from an unknown cause. There are seven toxin serotypes, which are labeled A through G, produced by C. botulinum. The genetic information is found on the bacterial chromosome for serotypes A, B, E, and F, on bacteriophages for serotypes C and D, and on plasmids for serotype G. The toxins bind to hemagglutinins, which may explain their resistance to degradation by human digestive enzymes. The toxins act on peripheral nerves by blocking the release of acetylcholine at the neuromuscular junction, and on autonomic nerves at synaptic ganglia and motor end plates. According to the CDC, the most common serotypes causing the clinical picture of botulism in the United States are type A and type B, with type A most commonly seen west of the Mississippi River and type B seen east of the Mississippi River. The clinical picture of wound botulism can be delayed due to an incubation period of four to fourteen days. This can be prolonged by wound debridement. The cranial nerves are affected first, with bulbar symptoms and vision changes seen as the hallmark symptoms of wound botulism, with dysarthria and dysphagia developing later. Respiratory failure requiring ventilator support is less common with wound botulism than it is with other forms of botulism, but it does occur. Reduced pupil reaction and generalized weakness and lethargy are also frequently seen. These symptoms can often be confused for stroke or other, more common, central nervous system disease processes, including Guillain-Barré syndrome, myasthenia gravis, Lambert-Eaton syndrome, or various intoxications. The diagnosis of wound botulism is often based on the clinical scenario. Cultures of wound specimens can take weeks to months to become definitively positive. Many clinical laboratories may not be able to definitively identify a Clostridium species as C. botulinum, and assistance may be required from state health departments or other organizations such as the CDC. The presence of botulinum toxin in blood, with the subsequent identification of C. botulinum in culture media, is a confirmatory test but remains unreliable. The most common electrophysiologic finding in botulism is reduction of the baseline compound muscle action potential amplitude (found in up to 85% of patients). Also reported, although less consistently, is a decremental response to RNS at slow rates, an incremental response to RNS at fast rates, an increment in the amplitude of the compound muscle action potential following brief exercise, and increased jitter and blocking on SFEMG. Our patient demonstrated only some of these features, which shows that swift recognition of the clinical symptoms of wound botulism in the appropriate patient population remains the best means of diagnosis. Penicillin remains the standard for treatment of C. botulinum infections; however, it will not reverse the symptoms of botulism caused by the neurotoxin. Antitoxin is available, but it is usually administered only in the early phase of the disease. Currently, a heptavalent antitoxin is available from the CDC, but it has not been approved by the U.S. Food and Drug Administration (FDA). Clostridial infections, although rare, can play an important role in open fractures and must remain in the forefront of the orthopaedic surgeon’s mind. Empiric antibiotic regimens for these patients should include appropriate coverage for Clostridium species and other anaerobic and environmental pathogens that may contaminate open wounds. Our case of a patient with bilateral open femoral fracture and subsequent wound botulism from infection of the left thigh wound with C. botulinum reinforces the need for a high level of clinical suspicion for this morbidity from contaminated wounds.
Reference: Reynolds KA, Young DR, Bariola JR, Stacy A. Rudnicki SA, Gruenwald JM. Bilateral open femoral fracture complicated by wound botulism. A case report. JBJS Case Connect. 2011;01:e3.
Botulism
Guillain-Barré syndrome
Psychiatric illness
Myasthenia gravis



 Fig. 1
Fig. 1 Fig. 2
Fig. 2![Fig. 3 Fig. 3 C. botulinum spores stained with malachite green. With this staining technique, the toxin-producing endospores stain green, whereas the C. botulinum bacilli stain purple. (Image obtained from CDC Public Health Image Library. Image credit: CDC/Courtesy of Larry Stauffer, Oregon State Public Health Laboratory [PHIL #1932], 2002.)](https://quiz.jbjs.org/wp-content/uploads/2012/04/iqapr12-2_fig3-150x150.jpg) Fig. 3
Fig. 3