A Sixty-four-Year-Old Woman with Acute Knee Swelling
May 2, 2012
A sixty-four-year-old woman with a history of hypertension had marked right knee pain, for which a right total knee arthroplasty was recommended. Her preoperative right knee radiograph demonstrated osteoarthritis (OA), as well as calcification of the lateral meniscus (Fig. 1-A). Two days after the total knee arthroplasty, she began rehabilitation therapy. Thirteen days postoperatively, she developed a fever of 38.4°C. The right knee was swollen and warm to the touch, but the surgical wound was free of drainage and was healing well. She had no pain in the right knee and was not taking nonsteroidal anti-inflammatory drugs (NSAIDs). Both the C-reactive protein (CRP) level (22.5 mg/L; normal: <3 mg/L) and the erythrocyte sedimentation rate (ESR) (29 mm/h; normal: <10 mm/h) were elevated. The total white blood-cell count and neutrophil count were 6.4 × 108/L and 4.9 × 108/L, respectively. She walked with a cane and had a knee range of motion from 0° to 110°. There was no radiographic evidence of loosening of the prosthesis (Fig. 1-B). The patient also had an upper respiratory tract infection and had been started on cefcapene pivoxil (CFPN-PI) (100 mg three times a day). The fever persisted for two days, and serum tests demonstrated a marked increase in the CRP level to 49.6 mg/L and further elevation in the ESR to 41 mm/h; the serum procalcitonin level was 0.09 ng/mL (normal: <0.5 ng/mL in sepsis). Arthrocentesis of the knee yielded 15 mL of bloody joint fluid. A Gram stain of the knee aspirate did not detect bacteria, but morphonuclear leukocytes were identified. Microscopy demonstrated calcium pyrophosphate dihydrate (CPPD) crystals in the aspirate fluid.
With the diagnosis of pseudogout as the likely cause of the knee swelling, antibiotic therapy was discontinued, and loxoprofen sodium (an NSAID) therapy was started. The patient’s temperature returned to normal on the next day. One week after the start of the loxoprofen sodium therapy, the serum inflammatory marker levels returned to normal. She was discharged from the hospital two weeks after the onset of the pseudogout attack. A review of the medical history revealed no prior episode of crystal arthropathy. The patient reported no additional episodes of pseudogout at the time of follow-up one year later. There was no radiographic evidence of loosening of the prosthesis (Fig. 1-C), and the CRP level and ESR were normal.
Proceed to Discussion >>Reference: Koyama K, Ohba T, Sato H, Haro H. Pseudogout mimicking infection following total knee arthroplasty. A report of two cases. JBJS Case Connect. 2012;e3. doi:10.2106/JBJS.CC.K.00049
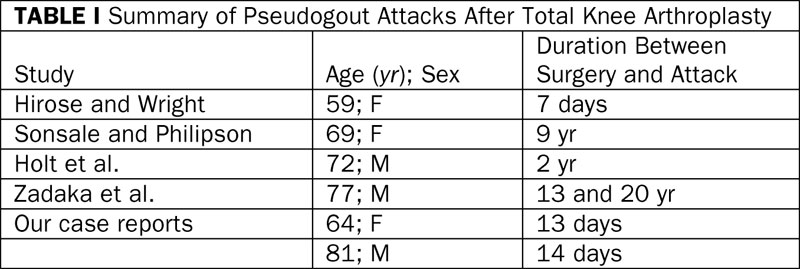
A diagnosis of pseudogout is established by the presence of CPPD crystals in synovial fluid or articular tissue (synovium, articular cartilage, and menisci), along with characteristic intra-articular calcific deposits in the synovium, articular cartilage, or menisci. CPPD crystals in synovial fluid can be detected and identified under light microscopy by their rod or rhomboid shapes, weak birefringence, and positive elongation. In a study of 102 patients with OA, CPPD crystals were detected in 53% during total knee arthroplasty; only one patient was aware of calcium deposits in the knee. Acute pseudogout attacks may mimic septic arthritis because both can present with joint pain, swelling, fever, and elevated serum inflammatory marker levels. Inflammatory marker levels, including CRP, ESR, and interleukin-6 (IL-6), are helpful for diagnosing septic arthritis, but these markers also can be elevated during a pseudogout attack. These points of resemblance between the two diseases can increase the difficulty of making an accurate diagnosis, especially during the early postoperative period. Of the four reported cases of pseudogout mimicking infection following total knee arthroplasty, only one occurred in the early postoperative period (Table I). The treatment of pseudogout consists mostly of local cooling and the use of NSAIDs. Our two patients had not used NSAIDs after the arthroplasty surgery. Pseudogout may often occur in patients who avoid the use of NSAIDs after arthroplasty surgery, although additional studies are needed to clarify this possible relationship. The use of NSAIDs before the attack of pseudogout was not described in the previous reports. The serum procalcitonin level has been reported as a helpful diagnostic marker for more reliable differentiation of infection from noninfectious causes of fever after orthopaedic surgery and for discrimination between septic and nonseptic arthritis. The sensitivity of the procalcitonin level was over 85% and 100% at the cutoff value of 0.1 ng/mL. In our two patients, the serum procalcitonin levels were 0.09 ng/mL and 0.07 ng/mL, respectively, at the time of the pseudogout attack. Three cases of pseudogout as a complication of unicondylar knee arthroplasty have been reported. Preoperative radiographs did not visualize calcific deposits in these three cases. In conclusion, acute crystal arthritis should be included in the differential diagnosis of septic arthritis after total knee arthroplasty because an incorrect diagnosis could lead to inappropriate debridement, unnecessary component removal, and antimicrobial chemotherapy. In particular, we believe that acute crystal arthritis should be ruled out before the prosthesis is removed. In order to distinguish pseudogout from postoperative septic arthritis, we recommend measuring the serum procalcitonin level and determining whether the use of NSAIDs was avoided following arthroplasty.
Reference: Koyama K, Ohba T, Sato H, Haro H. Pseudogout mimicking infection following total knee arthroplasty. A report of two cases. JBJS Case Connect. 2012;e3. doi:10.2106/JBJS.CC.K.00049
Broad-spectrum antibiotics, followed by specific antibiotics after culture results
Surgical irrigation and debridement of knee with broad-spectrum antibiotics
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Loading dose of allopurinol, followed by daily maintenance dose



 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Table I
Table I