A Fifty-seven-Year-Old Woman with Itching After Hip Revision Surgery
November 19, 2014
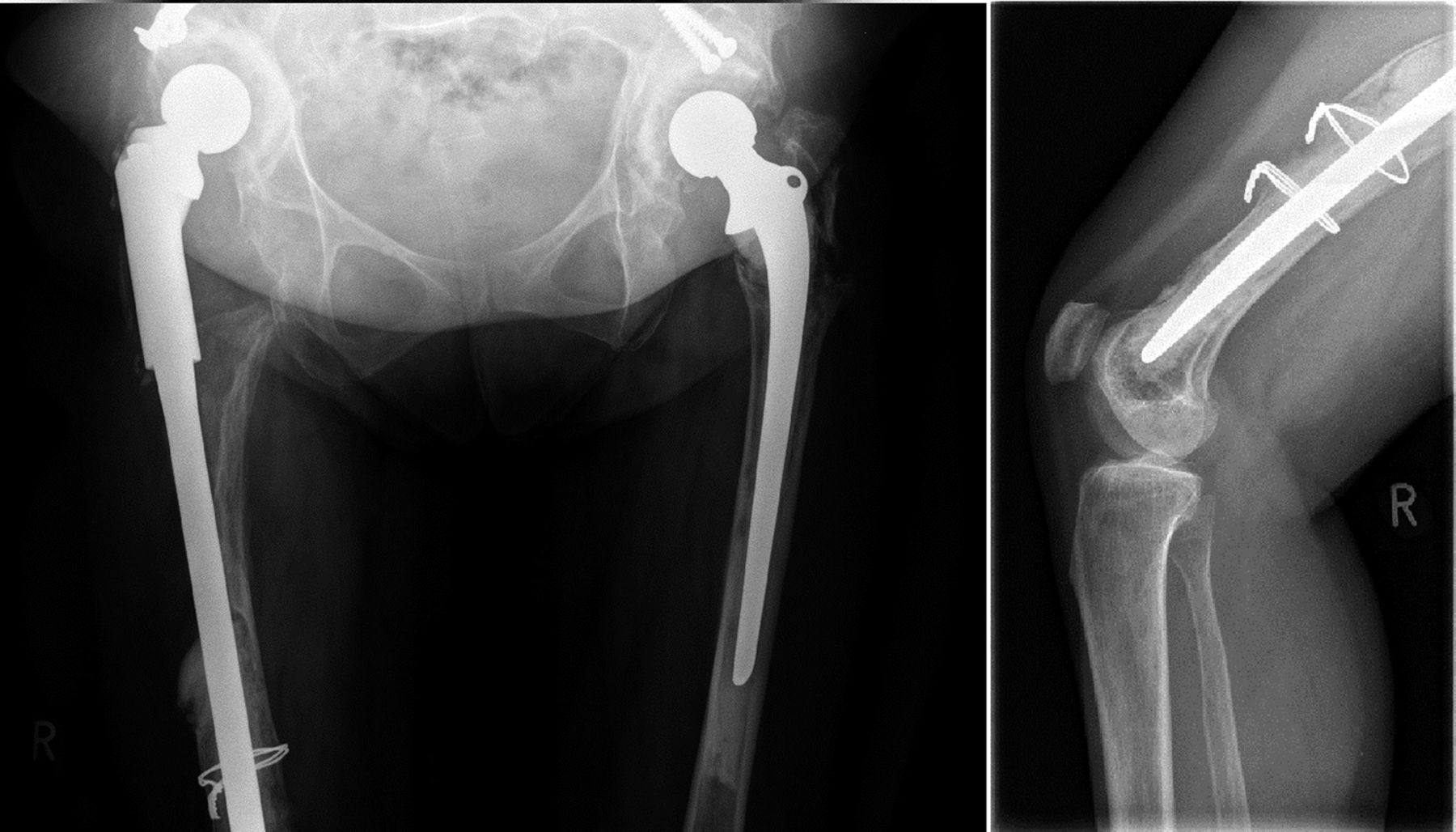
A fifty-seven-year-old woman with bilateral congenital hip dislocation underwent a fifth revision surgery on the right side, which included a long-stem femoral component with two additional distal wires to secure the implant (Fig. 1). Fixation of this long implant was performed with cement at the distal diaphysis and metaphysis. The femoral shaft was a cobalt, chromium, molybdenum (CoCrMo)-based alloy, and cerclages were made of stainless steel that contained Ni. Several weeks after surgery, itching and erythema overlying the distal part of the implant gradually developed (Fig. 2). There was no history of previous use of cerclage, as well as no history of seasonal rhinoconjunctivitis or sensitivity to jewelry (e.g., eczema upon contact with earrings or metal buttons). The patient was otherwise healthy without signs of infection (normal body temperature, white blood-cell count, erythrocyte sedimentation rate [ESR], and C-reactive protein [CRP] serum level). Therefore, she was referred for evaluation of a possible allergic reaction. To assess for metal sensitization, a patch test was performed with use of the German standard series, the metal series, and bone cement components. Furthermore, a lymphocyte transformation test (LTT) was performed. Ni, Co, and Cr salts and control stimuli were used. The proliferative response of the peripheral blood mononuclear cells was expressed as a stimulation index (SI), which represents the ratio of incorporated radioactivity in stimulated and unstimulated cultures. For the histological examination, two biopsies of the cutaneous lesion and one biopsy of uninvolved skin were taken. Staining with hematoxylin and eosin and a reverse transcription polymerase chain reaction (RT-PCR)-based molecular analysis of inflammatory mediator expression comparing lesional and uninvolved skin were performed. Upon testing with the standard series, a positive reaction to paraben mix was found; there was no reaction to Ni, Cr, or Co. The remaining patch test series, including bone cement components, showed no reaction. With use of the LTT, an elevated reactivity to Ni (SI = 2.7; normal, up to 2) was seen. Histopathological evaluation of the lesional skin biopsies revealed perivascular lymphocytic infiltrates in the upper and lower dermis, as well as discrete edema of the connective tissue. No eosinophils were noted. There was no excessive accumulation of mucin in the dermis. There were no epidermal changes, no signs of foreign material deposits, and no signs of infection (e.g., neutrophilic infiltrate) (Fig. 3). Because there could have been a hypersensitivity reaction without classical epidermal involvement (no eczema), we questioned whether the inflammatory mediator pattern contributed to the evaluation of the skin eruption. Therefore, an RT-PCR assay for cytokine expression in the lesional skin biopsy was compared with uninvolved skin (e.g., “control biopsy” from skin on the patient’s back). As shown in Figure 4, a panel of proinflammatory cytokines was expressed. In particular, interleukin (IL)-2, which is characteristic of T-lymphocyte activation, and interferon γ (IFNγ), which is a typical mediator of delayed-type reactions, were upregulated.
As a result of the diagnostic findings, we interpreted the skin changes as metal hypersensitivity mimicking periprosthetic erysipelas-like infection. As a potential underlying mechanism, we considered a local vasculitis-type hyperreactivity in association with the Ni-containing cerclage. Our patient received topical treatment with methylprednisolone aceponate 0.1% cream twice daily for two weeks, followed by prednicarbate 2.5% cream once daily for four weeks. The skin lesions and the pruritus disappeared, and at the twenty-four-month follow-up, there was full remission of the skin symptoms (Fig. 5) and the prosthesis remained stable (Fig. 6).
Proceed to Discussion >>Reference: Kulichová D, Gehrke T, Kendoff D, Summer B, Parvizi J, Thomas P. Metal hypersensitivity mimicking periprosthetic erysipelas-like infection. A case report. JBJS Case Connect, 2014 Aug 13;4(3):e65.
If a patient who has undergone multiple revision arthroplasty surgeries presents with a skin eruption overlying the implant after a recent procedure, the potential of infection must be considered. The recent article by Parvizi et al. provides the gold standard for the diagnosis of periprosthetic joint infection (PJI). In the rare cases of implant-associated dermatitis without signs of infection (e.g., fever and elevated CRP levels or ESR), a hypersensitivity reaction should be considered. Hypersensitivity reactions to orthopaedic implants are rare, but they have been reported as local or generalized skin changes, impaired wound or fracture-healing, recurrent pain, or even aseptic loosening. In view of the ongoing discussion about adverse reactions to metal debris in metal-on-metal arthroplasty, the topic of “hypersensitivity” has an increased clinical focus. The local release of metals like Ni, Co, or Cr may trigger eczema at sites overlying implants in patients with metal allergies. A similar finding was demonstrated in a patient with a known Ni and Co allergy who had pure titanium (Ti) osteosynthesis and developed eczema. After a thorough examination, it became evident that the patient had reacted to a hidden Ni release from the osteosynthetic material. It is known that CoCrMo alloys contain 0.5% (maximum, 1%) Ni; in contrast, a stainless steel (e.g., 316 L) cerclage, as used in our patient, contains a higher percentage of Ni (e.g., approximately 12% to 14%). Hyperreactivity reactions to Ti-based materials are very rare. In such cases, hidden Ni exposure should always be considered. In our case, the patient had developed local skin signs several weeks after revision surgery on the distal aspect of the femur. This, however, appeared as patchy erythema rather than eczema. There was no history of skin changes upon contact with earrings or metal buttons. There was no history of local application of any ointments (i.e., no indication of a potential external elicitor of contact dermatitis). Because the patient had no laboratory signs of infection, another etiology was considered. Differential diagnoses included reticular telangiectatic erythema (RTE), intralymphatic histiocytosis, reactive angioendotheliomatosis, Wells syndrome, and hypersensitivity presenting as pseudoerysipelas. A previously published report regarding four patients who had undergone arthroplasty investigated whether erysipelas-like rash after hip replacement may represent a distinctive form of infectious cellulitis. All of the cases presented with a localized, painless, recurrent, warm-to-touch, and sharply demarcated erythematous eruption on the thigh. There were only “moderate inflammatory blood changes,” and radiographic evaluation gave no evidence of infection in these patients. Histological analysis revealed normal epidermis, dermal edema, and an inflammatory infiltrate, which mainly consisted of neutrophils, a few lymphocytes, and occasional eosinophils. These findings and recovery after antibiotic treatment were interpreted as indicators of recurrent erysipelas. RTE is a condition with erythematous blanchable patches overlying implants, including pacemakers and orthopaedic devices. The diagnosis is based on exclusion of allergy (i.e., negative patch test), lack of signs of infection, and histology showing telangiectasia. The diagnostic criteria include erythematous blanchable reticular telangiectatic lesions over an implant, histology showing dermal telangiectasia and lymphohistiocytic infiltrate, absence of pain and infection at the surgical site, negative patch test results, and lack of response to antibiotic therapy. Thus, RTE should be included in the differential diagnosis of local erythema following implantation. Another rare but distinct benign condition is intralymphatic histiocytosis. Although it mostly presents in patients with rheumatoid arthritis, erythematous brownish plaques have also been observed in association with metal implants. Lymphatic stasis secondary to chronic inflammation or surgery has been proposed as a potential cause that leads to the histological picture of intravascular accumulation of histiocytes and neutrophils. Reactive angioendotheliomatosis presents with localized or widespread bruiselike lesions with a livedo pattern or multiple tender erythematous violaceous papules. Reactive angioendotheliomatosis may be secondary to intravascular deposits of immunoglobulins, but also may be associated with subacute infection (e.g., bacterial endocarditis). Histopathological analysis helps to exclude intravascular lymphoma. Wells syndrome or eosinophilic cellulitis may present as a solitary pruritic lesion or as a tender, warm lesion with circumscribed erythema and edema. The histopathology supports the diagnosis when eosinophil-rich infiltrate or, at a later stage, typical flame figures are found. Our patient had mild pruritus at the site of the skin lesions. She was afebrile and there were no laboratory signs of infection. The results of the patch test with implant metals were negative. Nevertheless, a hypersensitivity reaction appears most likely because of the enhanced LTT reactivity to Ni. Furthermore, the skin lesions were overlying the site of a stainless steel-based cerclage that could have been a potential source of Ni exposure. Thus, a skin biopsy for histological evaluation was taken, and lymphocytic vasculitis with no indication of infection or of the above-mentioned differential diagnoses was found. Finally, by assessing the cytokine expression in the lesion, typical signs for T-lymphocyte activation were found (e.g., IL-2, IFNγ). We concluded that the skin eruption, which presented as an erysipelas-like reaction, was related to a local vasculitis-type hyperreactivity in association with the Ni-containing cerclage. The skin lesions and the pruritus disappeared after six weeks of topical corticosteroid therapy. One possible explanation is that the anti-inflammatory treatment and a gradually diminished Ni release worked in parallel to promote peri-implant wound-healing. The presence of an inflammatory condition following insertion of an implant along with postoperatively changed pH in the peri-implant area may favor increased release of Ni that diminishes at the same time as the peri-implant “healing.” In summary, in cases of implant-associated skin eruptions, we recommend not only ruling out infection, but also considering metal hyperreactivity as a possible etiology.
Reference: Kulichová D, Gehrke T, Kendoff D, Summer B, Parvizi J, Thomas P. Metal hypersensitivity mimicking periprosthetic erysipelas-like infection. A case report. JBJS Case Connect, 2014 Aug 13;4(3):e65.
Cutaneous lymphoma
Hemosiderin dermal deposit
Metal hypersensitivity
Streptococcal cellulitis
Diffuse hemangioma



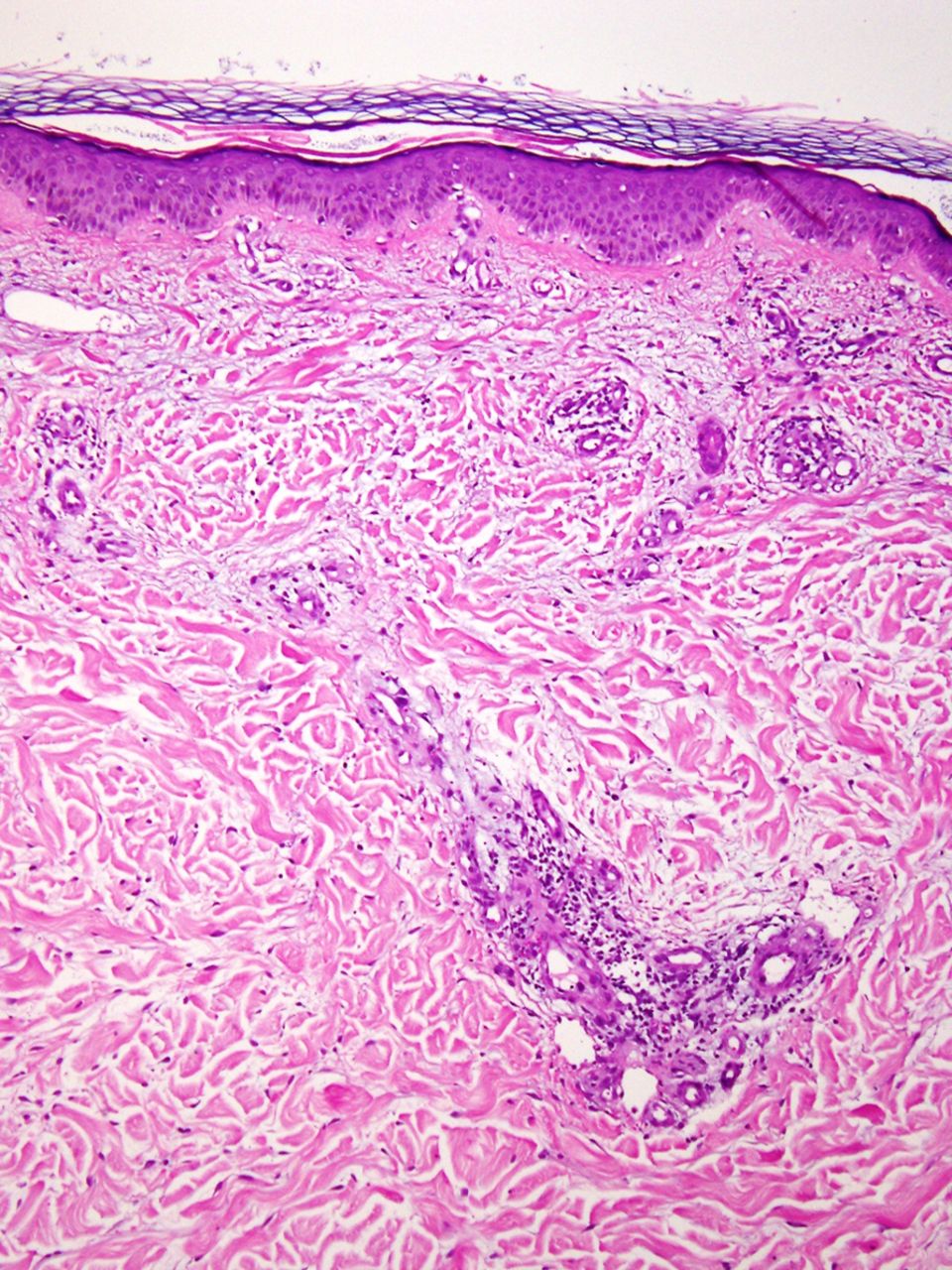
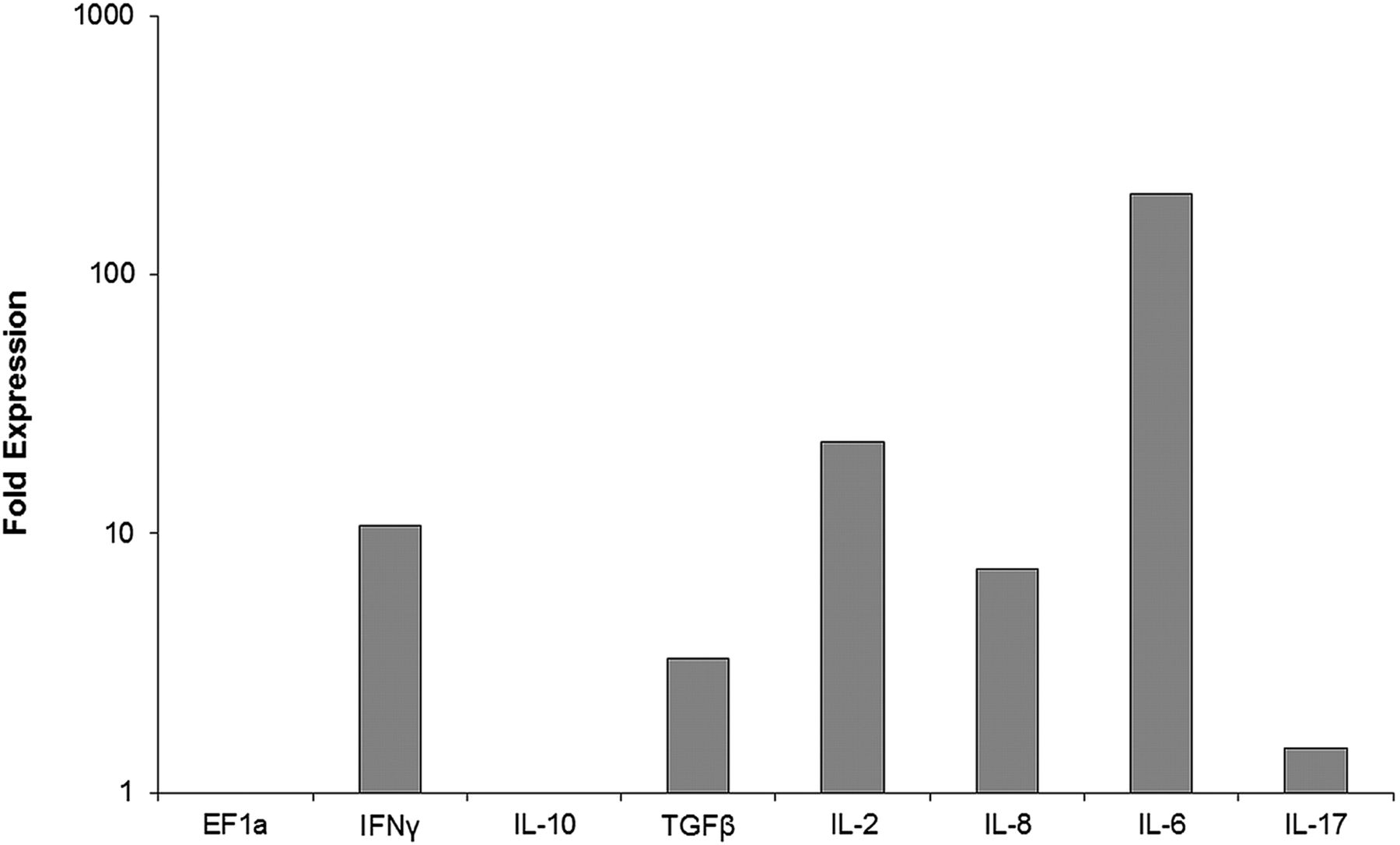
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3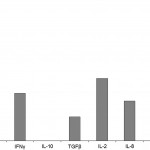 Fig. 4
Fig. 4 Fig. 5
Fig. 5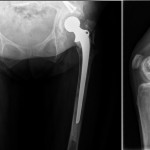 Fig. 6
Fig. 6