A Twelve-Year-Old Boy with Left Shoulder Injury
March 21, 2012
A twelve-year-old right-handed adolescent boy was playing hockey when he was checked from behind into the boards, which resulted in a left shoulder injury. His arm position at the time of impact is unknown. However, he did recall having his arm pinned against the boards, which caused a direct impact on the anterior aspect of the shoulder. The opponent continued to check him from behind while his arm remained pinned against the boards, which created a compression-traction-type combined injury pattern to the shoulder girdle. He recalled experiencing a pop, as though his shoulder had “come out of joint,” followed by the sensation of the joint spontaneously reducing when he fell to the ice. The patient presented to the hospital with pain and numbness of the left shoulder and hand ten hours postinjury. On examination, there was swelling and bruising anteriorly in the left axillary region (Fig. 1). The radial pulse was absent; however, the hand was well perfused with normal capillary refill to all digits. Neurologic examination revealed diminished motor and sensory function of the left axillary nerve and diminished sensory function in the hand for the radial and median nerve distribution. Radiographs of the shoulder revealed a reduced glenohumeral joint with a soft-tissue density within the axillary region suggestive of a hematoma (Fig. 2). A three-dimensional computed tomography (CT) angiogram revealed a flow defect in the third part of the axillary artery with an associated avulsion of the posterior humeral circumflex artery (Fig. 3). The patient was brought to the operating room on an urgent basis for vascular reconstruction and exploration of the brachial plexus. Intraoperatively, an anterior approach was used to localize and follow the brachial artery proximally to the avulsed axillary artery, which was reconstructed with use of a reverse saphenous vein graft harvested from the ipsilateral thigh (Fig. 4). The posterior humeral circumflex artery was ligated. The axillary vein was intact. A strong radial pulse returned following vascular reconstruction. Following vascular repair, the infraclavicular region of the brachial plexus was explored in the zone of injury. The axillary nerve was avulsed from the posterior cord of the brachial plexus (Fig. 4) and appeared elongated at its avulsed end, which is characteristic of a traction-type injury. The elongated portion was trimmed back from the zone of injury until a good fascicular pattern was identified, and it was sutured to the posterior cord in an end-to-side fashion. All other nerves were intact with a normal response to electrical stimulation, except for the musculocutaneous nerve, which was grossly intact but unresponsive to stimulation. Following neurovascular reconstruction, an intraoperative examination revealed a stable glenohumeral joint. Magnetic resonance imaging (MRI) of the left shoulder and brachial plexus on postoperative day two revealed increased signal intensity of all muscles originating from the coracoid process, most evident in the short head of the biceps brachii and coracobrachialis muscles. This altered signal intensity is consistent with a strain-type injury pattern of these muscles. There was also partial avulsion of the subscapularis muscle from its origin on the scapular body and a partial subscapularis tendon tear in the region of the musculotendinous junction (Fig. 5). The glenohumeral joint showed changes consistent with a posterior labral tear with posterior subluxation of the humeral head. The results of the brachial plexus MRI were normal proximally, with no evidence of nerve root avulsion. The patient was discharged with a shoulder sling on postoperative day three. Initial follow-up examination at two weeks revealed a normal radial pulse. There was full passive motion of the shoulder; however, active shoulder abduction was limited to 30° with Medical Research Council (MRC) grade-0 power (muscle grading from 0 to 5) evident within the left deltoid muscle. There was sensory loss over the axillary nerve distribution. The findings of the remainder of the neurologic examination were normal. All joints of the shoulder girdle were stable on examination.
Neurophysiologic studies at three months postinjury were consistent with complete axonal loss of the left axillary nerve and reduced motor recruitment of the infraspinatus muscle. Wasting of the left deltoid muscle was evident. With no clinical recovery of axillary nerve function over the subsequent three months, the axillary nerve was re-explored. With use of a posterior approach, a radial-to-axillary nerve transfer procedure was performed, whereby a motor branch of the radial nerve supplying the long head of the triceps muscle was transferred to the left axillary nerve close to its entry into the deltoid muscle. At the time of follow-up at fifteen months after the original injury and nine months after the nerve transfer, there was persistent evidence of muscle atrophy involving the deltoid muscle and, to a lesser degree, within the infrascapular region. Passive and active motion of the left glenohumeral joint was nearly full and symmetric. There was MRC grade-4 power involving all three heads of the deltoid muscle, the triceps, and the external rotators of the left shoulder. The results of special tests targeting the subscapularis muscle were normal with the exception of a positive bear hug test (the hand of the affected side is placed on the contralateral shoulder, and the patient tries to resist the examiner’s attempt to pull the hand up). Sensory loss over the axillary nerve distribution remained unchanged. The remainder of the findings of the examination were normal. Repeat radiographs of the left shoulder showed unremarkable findings. Repeat MRI of the left shoulder revealed deltoid muscle atrophy, teres minor muscle atrophy, and fatty infiltration of the deltoid muscle. The remainder of the previously described injuries to the muscular and capsulolabral structures had resolved. According to the patient, he had returned to contact hockey and had not had any recurrent episodes of shoulder instability.
Proceed to Discussion >>Reference: Bois AJ, Dzus AK. Neurovascular injury following traumatic posterior shoulder dislocation in an adolescent contact athlete. A case report. JBJS Case Connect. 2011;01:e1.
Neurovascular injuries following simple shoulder dislocations are rare. Blunt trauma accounts for approximately 6% of all axillary artery injuries; simple shoulder dislocations account for less than 1% of these blunt injuries. More than 90% of reported cases of vascular injury following shoulder dislocation occur in patients over the age of fifty, and with over 200 cases reported, we are aware of only one case reported in the pediatric population. Isolated axillary nerve injuries are also infrequent. We found only one case in the literature of an isolated axillary nerve injury in the pediatric age group following a simple shoulder dislocation. Across all age groups, we believe that ours is the first case report of a combined axillary artery injury and nerve avulsion following a simple shoulder dislocation. The axillary artery is typically injured at its third segment as a result of its relatively fixed position by the circumflex humeral artery and the scapular artery. Arterial elasticity is decreased in the presence of atherosclerosis, which results in an increased risk of vascular injury following shoulder dislocation with increasing age. Axillary artery injury should be considered when there is a history of shoulder dislocation, a reduction or loss in amplitude of the radial or brachial pulse, and the presence of an expanding axillary mass. Our patient presented with a perfused hand, which was likely due to the extensive collateral circulation around the shoulder. In addition, the radial pulse was absent, there was evidence of an expanding axillary hematoma, and the patient presented with limb ischemia. Baratta et al. reported on a thirteen-year-old boy who had sustained a left axillary artery laceration following an anterior shoulder dislocation while wrestling. The patient underwent surgery in which a 3-cm thrombosed segment of the axillary artery was resected and was reconstructed with a reverse saphenous vein graft. The patient had complete shoulder motion and normal findings on a neurovascular examination at the three-year follow-up evaluation. The axillary nerve is also susceptible to traction and compression injuries following shoulder dislocation as it has a relatively short excursion distance within the axilla. In addition, the axillary nerve is tethered to the deep surface of the deltoid muscle as it courses around the surgical neck of the proximal part of the humerus. Isolated axillary nerve injuries account for a small percentage of brachial plexus injuries, but they have been reported to occur between 19% and 55% of the time following anterior shoulder dislocation. Risk factors for axillary nerve injury following simple anterior shoulder dislocation include increased age, hematoma, and an associated fracture of the proximal part of the humerus. The incidence of axillary nerve injury following posterior shoulder dislocation is unknown. Tyagi et al. reported an isolated axillary nerve injury following a shoulder dislocation in a twelve-year-old boy who was checked into the boards while playing hockey. Following six months of nonoperative management with no recovery of deltoid function, the axillary nerve was explored. The nerve was intact but surrounded by extensive scar tissue, and a neurolysis was performed. At the time of final follow-up at eighteen months, the deltoid had completely recovered to MRC grade-5 power. The resulting deltoid muscle palsy that accompanies an axillary nerve injury considerably alters the stability and function of the shoulder and upper limb. To obtain the best functional results, surgical exploration is recommended for patients with an axillary nerve injury that fails to improve in four to six months. Nerve transfer, or neurotization, can be performed for both preganglionic and postganglionic nerve injuries and involves the transfer of a functioning nerve of lesser importance to the more important denervated distal nerve. A recent meta-analysis suggests that the results of nerve transfer to regain shoulder abduction may be superior to the results obtained with tendon transfer. Neurotization procedures aimed at returning shoulder abduction have historically used single nerve transfer to the suprascapular nerve. More recent efforts combine these transfers with nerve transfers to the axillary nerve with use of the motor branch to the long head of the triceps muscle. Full recovery from an axillary nerve injury due to dislocation or fracture occurs 85% to 100% of the time with nonoperative management, and these cases likely reflect a lesser severity of neural injury. In our case, spontaneous recovery was less likely to occur despite efforts made with an end-to-side primary reconstruction because the axillary nerve had been avulsed from the posterior cord of the brachial plexus. Our patient underwent a nerve transfer procedure at six months after the original injury, with use of the motor branch to the long head of the triceps muscle, and had MRC grade-4 power of the deltoid at the fifteen-month follow-up examination. The residual external rotation weakness in our patient was likely the result of teres minor muscle dysfunction, which often accompanies proximal injury to the axillary nerve. Combined injuries to neurovascular structures around the shoulder typically result from high-energy trauma as seen in scapulothoracic dissociation (SD), which is characterized as a complete disruption of the scapulothoracic articulation with lateral scapular displacement and intact skin leading to a spectrum of musculoskeletal, neurologic, and vascular injuries. SD is a rare traumatic injury most commonly found in adults, with only a few reports in the pediatric age group. In the case reported here, our initial clinical impression was that the patient had experienced a subtype of SD, as suggested radiographically by the combined neurovascular injury and laterally displaced scapula. However, the severity of neurovascular injury alone does not warrant a diagnosis of SD, and our patient did not meet all the diagnostic criteria for SD. Our patient’s mechanism of injury involved a combination of anterior compressive forces and longitudinal-traction forces. A posteriorly directed force of the humeral head would account for the posterior labral tear. The combined compressive and tractional forces would account for tears within the associated muscles of the conjoint tendon and subscapularis musculotendinous unit as well as avulsions of the axillary artery and nerve. In children, the viscoelastic nature of their soft tissues and immature skeleton may provide protection from neurovascular and osseous injuries resulting from blunt trauma. However, our patient experienced both neurovascular and musculoskeletal injuries following a relatively low-energy shoulder injury. The majority of neurovascular injuries following shoulder dislocation in the literature have involved patients fifty years of age or older. Such injuries should be considered in children who present with neurovascular compromise following blunt shoulder trauma.
Reference: Bois AJ, Dzus AK. Neurovascular injury following traumatic posterior shoulder dislocation in an adolescent contact athlete. A case report. JBJS Case Connect. 2011;01:e1.
Short head of biceps and subscapularis
Teres minor and long head of triceps
Supraspinatus and subscapularis
Subscapularis and teres major



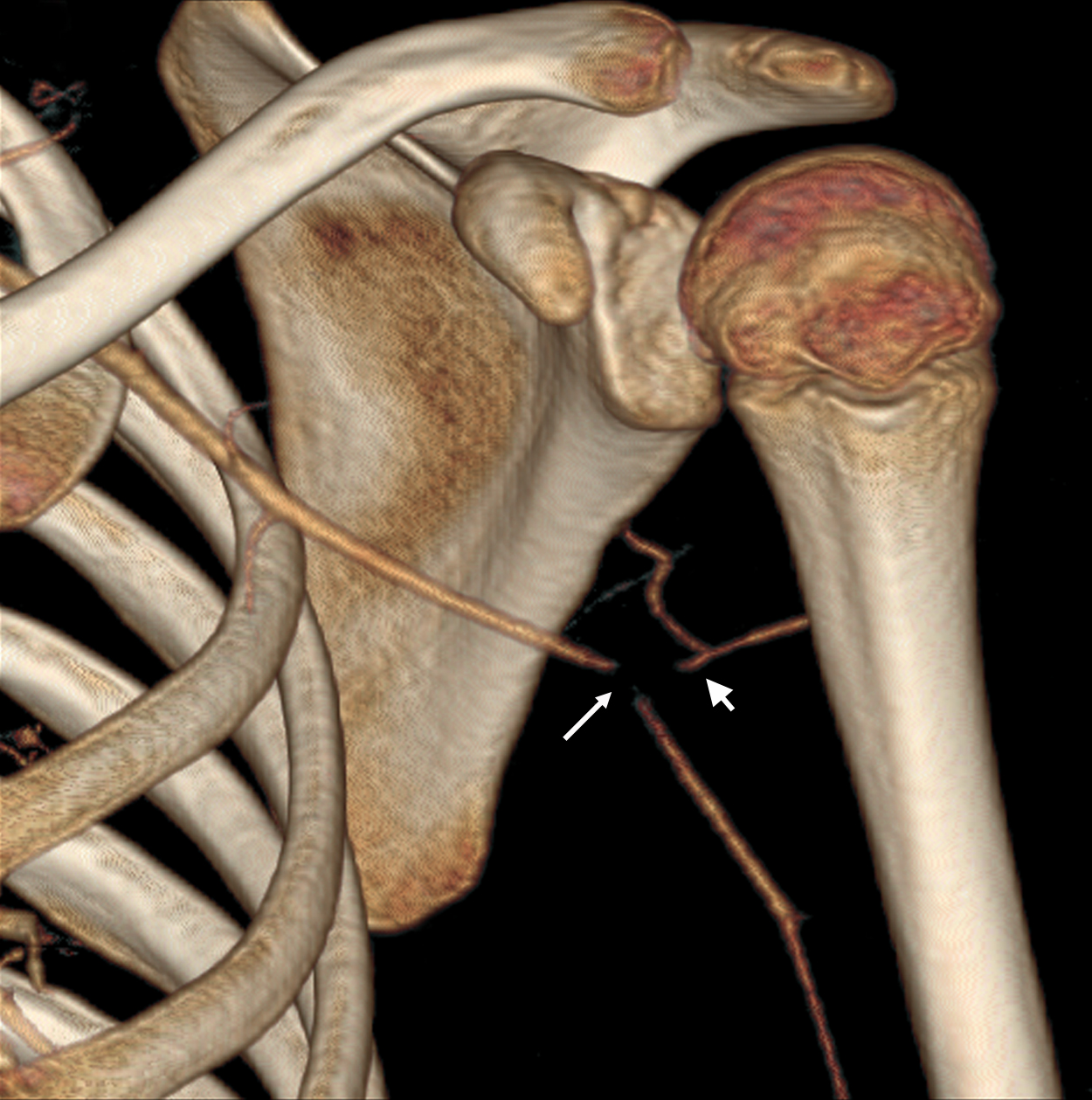


 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5