A Fifty-six-Year-Old Woman with Sudden Leg Weakness
May 16, 2012
A fifty-six-year-old woman was transferred to our emergency department with a sudden onset of sepsis, with dyspnea, a stuporous mentality, and weakness of both lower extremities. She had been generally in a good state of health until two weeks previously, when she developed lower back pain. She underwent nonoperative treatment for lower back pain during those previous two weeks, and she was given antibiotic treatment (ceftriaxone) for a fever that suddenly developed twelve days after the onset of back pain and two days before arrival in our emergency room. She had had diabetes mellitus and high blood pressure for many years. She had no history of intravenous drug or alcohol abuse. There was no specific event that triggered the onset of the symptoms, and she had not had a recent respiratory or urinary tract infection or an invasive procedure on the spine. On examination, the patient’s temperature was 36.5°C, and she had tenderness in the back. The neurologic examination showed marked global weakness (grade 1 [flicker of contraction present] or grade 2 [active movement with gravity eliminated] of 5) in both lower extremities. No sphincter disturbance was found. The laboratory findings included a white blood-cell count (WBC) of 15,950 cells/mm3 (normal, 5000 to 10,000 cells/mm3), an erythrocyte sedimentation rate (ESR) of 78 mm/hr (normal, 0 to 15 mm/hr), and a C-reactive protein (CRP) level of 303 mg/dL (normal, <5 mg/dL). Radiographs of the lumbar spine revealed mild degenerative changes and generalized paralytic ileus. Chest radiographs revealed multiple round densities, several of which had central lucencies, throughout both lung fields. A contrast-enhanced computed tomography (CT) scan of the chest performed immediately after the radiography demonstrated multiple pulmonary consolidations (Fig. 1-A). The contrast-enhanced abdominal CT scan revealed multiple thrombi in the inferior vena cava, the common iliac vein, and the renal vein adjacent to a mass (Figs. 1-B, 1-C, and Fig. 1-D). Echocardiography revealed no evidence of endocarditis. Magnetic resonance imaging (MRI) with gadolinium enhancement revealed extensive psoas, retroperitoneal, and prevertebral involvement with a signal change in the L3 and L4 vertebral bodies. The MRI also revealed a mass from L2 to L5 with compression of the dural sac (Fig. 2).
We diagnosed the patient as having a septic condition with disseminated septic emboli and septic thrombosis of the vena cava and the common iliac and renal veins caused by vertebral osteomyelitis or pyogenic spondylitis of the lumbar spine. An urgent decompression consisting of L3 to L5 laminectomies was performed after an inferior vena cava filter had been placed to prevent pulmonary embolism and brain infarct. A massive amount of pus was noted in the epidural space, and culture specimens were obtained. After irrigation of the epidural space, curettage and debridement of the infected L3-L4 and L4-L5 discs was performed. Copious irrigation of the retroperitoneal space was carried out through a perforated area in the anterior longitudinal ligament of the L3-L4 disc space with use of a drainage tube made of a Nelaton catheter. The drainage tube was left in place postoperatively. After surgery, the patient had septicemia with a high fever, pulmonary edema, and acute renal failure. Methicillin-sensitive Staphylococcus aureus was grown on culture of blood and specimens of the intraoperative abscess. The patient was treated with intravenous nafcillin and clindamycin. On the eighth postoperative day, the drainage tube was removed. However, she continued to have purulent discharge at the drain site and a high fever with an elevated WBC. Another contrast-enhanced CT scan of the abdomen was performed, and it demonstrated a pseudomembranous colitis. Intravenous metronidazole, instead of clindamycin, was then administered. On the thirteenth postoperative day, irrigation and drainage of the previous drain site was performed with the patient under local anesthesia. Despite antibiotic therapy, her febrile condition, leukocytosis, and increased CRP level persisted. Thus, the treatment was changed to triple antibiotic therapy with vancomycin, imipenem, and amikacin. Because of the acute renal failure and pulmonary edema, mechanical ventilation was required, and continuous renal replacement therapy (hemodialysis) was performed on the twenty-second postoperative day. The patient’s clinical condition and symptoms gradually improved, and mechanical ventilation and the renal replacement therapy were discontinued on the thirty-first postoperative day. The wound was closed on the thirty-third postoperative day, and the antibiotic treatment was changed to parenteral moxifloxacin on the fifty-second postoperative day. The paralysis of the lower extremities gradually improved, and the patient started walking with a cane at approximately ten weeks postoperatively. She underwent vigorous rehabilitation, and she was discharged on the eightieth postoperative day. On discharge, the symptoms and clinical condition had improved greatly and the ESR and CRP level were within normal limits. The contrast-enhanced abdominal and chest CT scans obtained one year postoperatively showed complete resolution of the septic thrombi in the inferior vena cava and the common iliac and renal veins and the abscesses in the lung and soft tissue. The CT scans also showed complete regression of the epidural, prevertebral, and retroperitoneal abscesses. At the time of the latest follow-up, the radiographs of the lumbar spine showed spontaneous fusion at L3-L4 (Fig. 3). The patient had mild intermittent lower back pain and was able to walk without any walking aids.
Proceed to Discussion >>Reference: Lee JS, Kim KW. Disseminated septic emboli, septic thrombosis of the vena cava and the common iliac and renal veins, and retroperitoneal abscess secondary to pyogenic spondylitis of the lumbar spine. A case report. J Bone Joint Surg Am. 2011;93:e59.
The most common cause of septic thrombosis of the vena cava is prolonged central venous catheterization or parenteral nutrition in children, infants, or immunocompromised patients. Previous reports have shown that staphylococcal and streptococcal species as well as gram-negative and fungal organisms are the most common causes of this infection. In our case, methicillin-sensitive Staphylococcus aureus was grown on culture of both blood and abscess specimens. We were unable to identify any predisposing factors for the septic thrombosis of the vena cava, the common iliac vein, and the renal vein. We believe that the hematogenous pyogenic spondylitis led to perforation of the anterior longitudinal ligament and subsequent formation of a massive retroperitoneal abscess that ultimately extended to the adjacent vena cava, the common iliac vein, and the renal vein, resulting in suppurative thrombophlebitis and septic thrombosis. Suppurative thrombophlebitis and septic thrombosis require specific treatments for the underlying primary infectious sites in combination with prolonged systemic antibiotic therapy. If nonoperative treatment fails, then surgical thrombectomy is recommended. Low-dose streptokinase infusion in combination with antimicrobial therapy has been reported to be the appropriate treatment of infectious caval thrombosis in children. However, the role of systemic anticoagulation is unclear. Surgical thrombectomy was not performed in our patient because urgent surgical decompression of the epidural abscess and drainage of the retroperitoneal abscess were needed to treat the progression of the neurologic deficits and the septic condition. In addition, streptokinase infusion was contraindicated in our patient because of the dangers of uncontrollable hemorrhage during the emergency spinal surgery. We used a vena cava filter to prevent any embolic events during the spinal surgery. A recent study demonstrated that the “off label” use of a vena cava filter in combination with adequate antibiotic coverage is a safe and effective treatment method for patients with septic thrombosis of the vena cava for whom anticoagulation therapy is contraindicated. Fortunately, no more embolic events occurred after the surgery in our patient. The latest follow-up CT scan showed complete resolution of the septic thrombi in the inferior vena cava and the common iliac and renal veins. The choice of surgical approach for the pyogenic spondylitis is based on the location of the primary pathological entity. Most cases of pyogenic spinal infection occur in the anterior column of the spine. In most cases, an anterior surgical approach is preferable to accomplish more thorough debridement and to facilitate reconstruction of the anterior column. Combined anterior and posterior surgical approaches can also be performed, as they provide for a more rigid instrumentation construct and immediate spinal stability. However, anterior surgery was not considered for our patient because of the septic thrombi in the inflamed large veins in this area. In addition, anterior surgery was inappropriate for the decompression of the extensive epidural abscess that was located from L2 to L5. Our patient’s general condition was so critical that we were unable to perform combined anterior and posterior surgery. Therefore, we performed neural decompression and abscess drainage through the posterior approach only. The septic thrombi were unexpected findings in our patient. We were unable to identify any clinical signs of septic thrombosis of the vena cava or the common iliac and renal veins because there was no swelling in the extremities, cutaneous ecchymosis, or acute renal failure. Because of the sudden onset of dyspnea, stuporous mentality, and paralytic ileus, we performed the contrast-enhanced chest and abdominal CT scans, on which multiple septic thrombi in the large veins were identified.
Reference: Lee JS, Kim KW. Disseminated septic emboli, septic thrombosis of the vena cava and the common iliac and renal veins, and retroperitoneal abscess secondary to pyogenic spondylitis of the lumbar spine. A case report. J Bone Joint Surg Am. 2011;93:e59.
Vertebral bacterial infection
Metastatic lung carcinoma
Tuberculosis of spine and lungs
Coccidioidomycosis infection



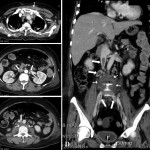 Fig. 1
Fig. 1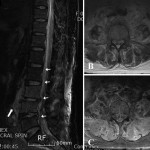 Fig. 2
Fig. 2 Fig. 3
Fig. 3