A fourteen-month-old boy was brought to the emergency department by his parents after he had abruptly stopped bearing weight on his left lower extremity that morning. They reported a three-day history of irritability and decreased appetite, but no history of trauma to the left lower extremity. An orthopaedic consult was requested to evaluate the child. He was born at term via cesarean section because of a breech position. Screening ultrasound shortly after birth revealed evidence of bilateral developmental dysplasia of the hip, which was treated successfully with a hip spica cast. The patient had begun walking at twelve months of age. His immunization status was deficient since he had only received his two-month immunizations. The medical history was remarkable for undescended testes. On presentation, the patient did not appear toxic and had a low-grade fever of 100.4°F (38°C). His parents stated that they had given him Tylenol (acetaminophen) and Motrin (ibuprofen) prior to coming to the emergency department. He was holding the left leg externally rotated and flexed at the hip, both while he was supine and while he was held upright by the examining physician. Additionally, he refused to extend or bear weight on the left lower limb or crawl when placed on his hands and knees. The left hip was diffusely tender, without any distinct palpable masses or skin changes. He showed minimal signs of discomfort with passive internal and external rotation of the left hip and axial loading of the left lower extremity. The passive range of motion of the left hip on the initial orthopaedic evaluation consisted of 120° of flexion, 20° of extension, 45° of abduction, 25° of adduction, 60° of internal rotation, and 80° of external rotation. Passive motion of the knee was from full extension to 140° of flexion. He had no pain on palpation of the spine or loading of the sacrum. Initial radiographic examination demonstrated symmetric hip joints with no evidence of acute osseous injury. Laboratory studies showed a peripheral leukocyte count of 16,700 cells/mL, an erythrocyte sedimentation rate (ESR) of 103 mm/hr, and a C-reactive protein (CRP) level of 4.7 mg/dL (normal, 0 to 0.49 mg/dL). Ultrasound of the left hip showed no evidence of joint effusion or capsular thickening. On reevaluation later in the day, the patient had a fever of 101.5°F (38.6°C) but still had no substantial pain or discomfort with passive motion of the left hip, although he continued to hold the lower extremity in a flexed and externally rotated position at the hip and refused to bear weight on this extremity. Given the substantial disparity between the results of the laboratory evaluation and the physical examination and imaging findings, the patient was admitted to the hospital and a magnetic resonance image (MRI) was obtained for additional evaluation (Figs. 1 and 2).
The MRI revealed undescended testes as well as T2-weighted signal abnormalities in the inguinal canal bilaterally and a left inguinal mass that raised concern about possible hernia, neoplasm, or testicular torsion (Fig. 2). General surgery and urology consultations were obtained. The patient underwent a testicular ultrasound. Following analysis of this ultrasound, he was taken urgently to the operating room by the general surgery team for a left groin exploration, left orchiectomy, and inguinal canal reconstruction. Intraoperatively, he was found to have a gangrenous, torsioned, undescended left testis with marked edema and inflammatory changes in the left inguinal canal. The patient had a benign postoperative course and was discharged home two days postoperatively. At the time of follow-up six months later, he had a normal gait and full hip range of motion and strength and he had returned to full activity without any recurrent symptoms.
Proceed to Discussion >>Reference: Napierala MA, Rush J, Possley D, Young J, Ritchie E, Alderete J. Gangrenous testicular torsion, presenting as refusal to bear weight, in a fourteen-month-old child. A case report. J Bone Joint Surg Am. 2011;93:e139. doi:10.2106/JBJS.J.01905
Torsion of an undescended testis (UDT) is a relatively rare phenomenon that is not commonly encountered by orthopaedic surgeons. However, it is a condition that requires prompt diagnosis and surgical treatment by a general surgeon or urologist. The incidence of cryptorchidism, or UDT, in full-term neonates is estimated to be 2.7% to 5.9% at birth but decreases to 1.2% to 1.8% by the age of one year. Children with a history of UDT are at an increased risk (up to tenfold) of testicular torsion. There is a high rate of necrosis of the testis in the setting of testicular torsion, with surgical salvage rates as low as 10%. Clinical symptoms include the appearance of inguinal swelling and erythema, as well as a tender, firm mass palpated in the groin region. Patients may exhibit nausea, vomiting, fever, or inconsolability or refuse to bear weight. When a toddler presents with a refusal to bear weight, potential causes include septic arthritis or transient synovitis of the hip, osteomyelitis, discitis, fracture, or neoplasm. However, there are a myriad of potential causes of this symptom. When a child presents with fever, an inability to bear weight on an extremity, elevated levels of inflammatory markers, and a hip held in flexion and external rotation, the clinician should consider septic arthritis of the hip as the most likely diagnosis. This is a serious condition that requires early intervention with operative irrigation and debridement and intravenous antibiotics. Sequelae associated with septic arthritis include systemic or persistent infection, arthritis, osteonecrosis of the proximal part of the femur, physeal closure, growth disturbance, synovitis, arthrofibrosis, and joint stiffness. Early diagnosis of septic arthritis is imperative as poor clinical outcomes have been associated with a delay in diagnosis. Clinicians have used elevated levels of inflammatory markers (CRP levels, ESR, and peripheral leukocyte count) as well as physical examination findings to assist them in differentiating septic arthritis from more benign reactive conditions, including transient synovitis of the hip. There are multiple algorithms to assist with this differentiation. Kocher et al. retrospectively studied 282 children who had been evaluated at their institution for an irritable hip. They identified four independent predictors to help differentiate between septic arthritis and transient synovitis: a history of fever (an oral temperature of >38.5°C), a history of non-weight-bearing, an ESR of >40 mm/hr, and a white blood-cell count (WBC) of >12,000 cells/mL. The predictive probability of septic arthritis of the hip was 0.2% for zero predictors, 3% for one predictor, 40% for two predictors, 93.1% for three predictors, and 99.6% for four predictors. This method was prospectively validated at the same institution in a study of 213 children between 1997 and 2002. The authors found that the predictive probability was 2% for zero predictors, 9.5% for one predictor, 35% for two predictors, 72.8% for three predictors, and 93% for four predictors. Caird et al. retrospectively studied fifty-three children who had undergone hip aspiration because of a suspicion of septic hip arthritis. They evaluated five predictors: a history of fever (an oral temperature of >38.5°C), a history of non-weight-bearing, an ESR of >40 mm/hour, a CRP level of >2.0 mg/dL, and a WBC of >12,000 cells/mL. The authors found that the predictive probability was 83% for three predictors, 93% for four predictors, and 98% for five predictors. Our case presents an interesting diagnostic dilemma. The patient exhibited all four of the criteria in Kocher’s algorithm as well as an elevated CRP level. On the basis of this information, the probability of a septic hip could have been as high as 93% to 99%. Thus, if we had used only the accepted and validated algorithm, we might have recommended hip aspiration, which involves its own inherent risks. However, this patient had several characteristics seemingly incompatible with septic arthritis. He had a minimally painful range of motion of the hip, although he did have diffuse tenderness about the hip region and held the hip in a flexed and externally rotated position. Second, no effusion was noted on ultrasound. Ultrasound is commonly used in the evaluation of septic arthritis, and a lack of effusion is commonly thought to preclude the diagnosis of septic arthritis. However, the sensitivity of ultrasound in the diagnosis of septic arthritis is not 100%; in fact, it ranges from 82% to 86%. For these reasons, an MRI was obtained; it revealed an inguinal mass later confirmed to be a necrotic testis as a result of torsion. The differential diagnosis of a child presenting with refusal to bear weight is extensive. While septic arthritis and transient synovitis are two common causes, other causes exist and must be considered, especially given a clinical picture not completely compatible with either diagnosis. Our case illustrates the seemingly endless list of potential causes of a common symptom encountered in orthopaedic practice. Furthermore, it illustrates that abdominal or genitourinary pathology can mimic hip pathology and therefore must always be considered in the differential diagnosis. While MRI is not typically in the algorithm for diagnosis of septic arthritis of the hip, it is a powerful tool, if available, with which to make sense of a confusing situation. Our case illustrates that, while clinical algorithms such as Kocher’s criteria are extremely valuable, the clinician should be careful not to use them as a "cookbook," but rather should view them as one of many tools available to utilize when making a diagnosis.
Reference: Napierala MA, Rush J, Possley D, Young J, Ritchie E, Alderete J. Gangrenous testicular torsion, presenting as refusal to bear weight, in a fourteen-month-old child. A case report. J Bone Joint Surg Am. 2011;93:e139. doi:10.2106/JBJS.J.01905
Inguinal canal abscess
Transient synovitis of left hip
Testicular torsion
Septic arthritis of left hip with localized iliopsoas abscess
Teratoma in inguinal region

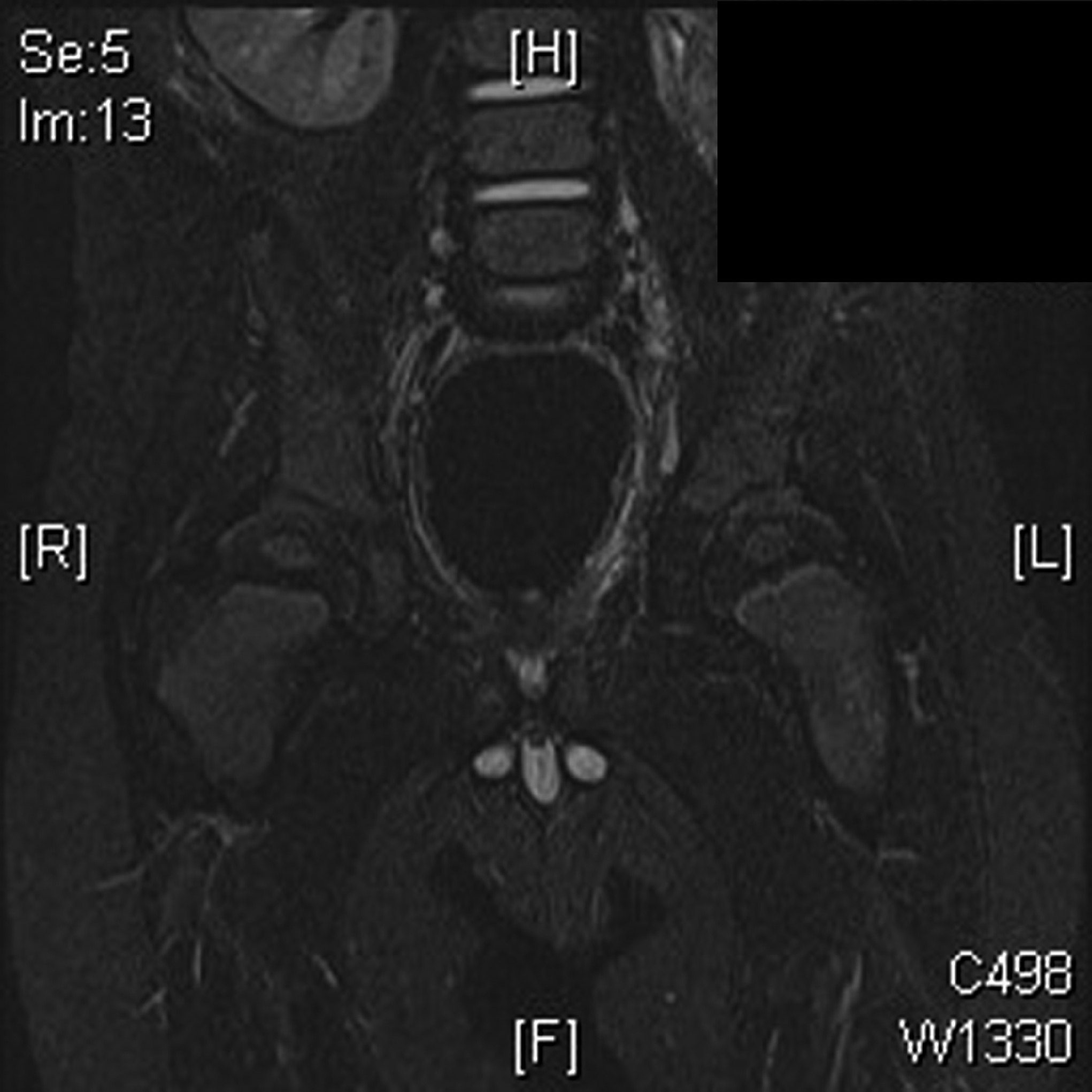
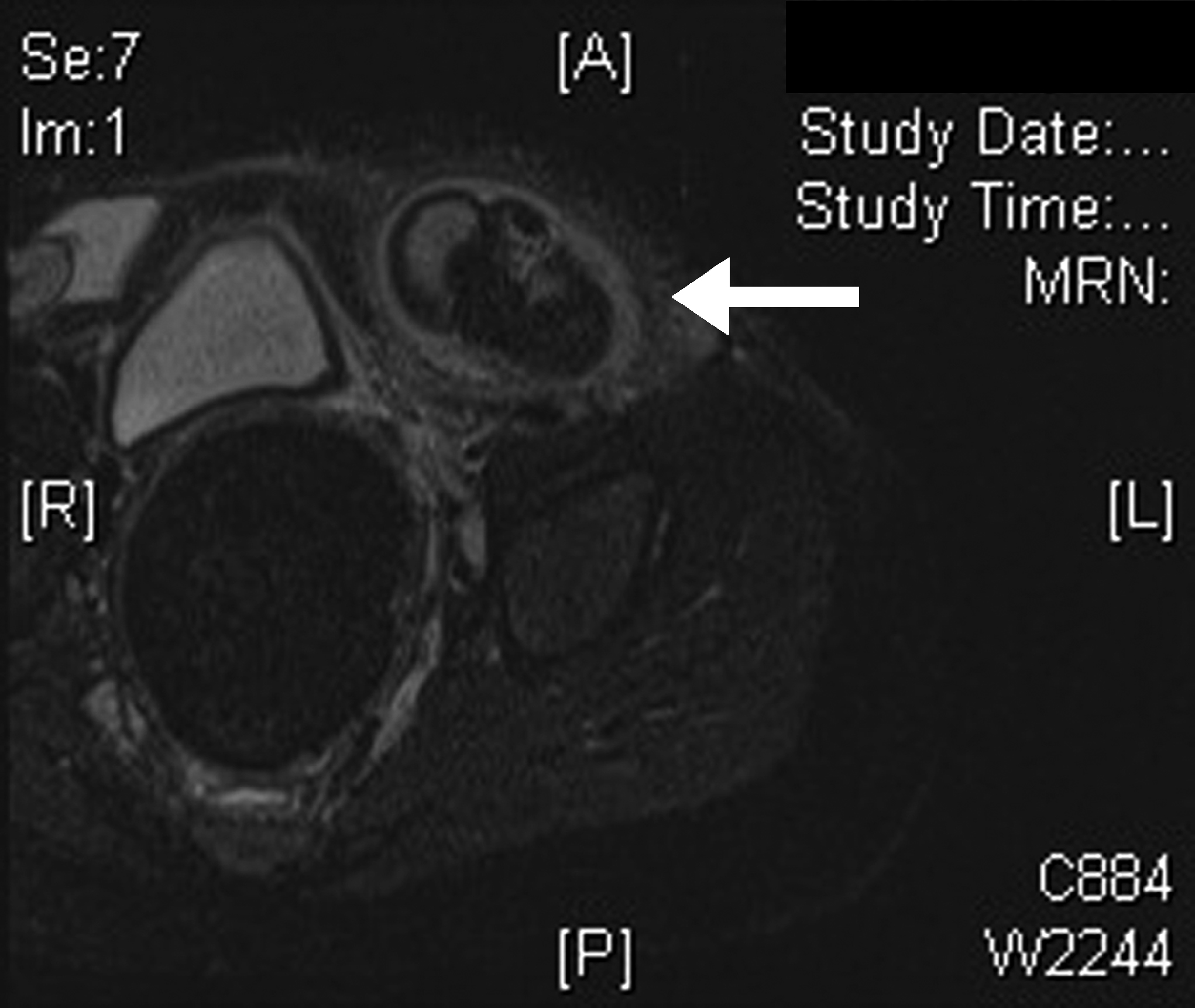
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 2
Fig. 2