A Forty-four-Year-Old Man with Abdominal Pain After a Gunshot-Induced Femoral Fracture
January 28, 2011
A forty-four-year-old African-American man sustained a gunshot wound to the right thigh, resulting in a fracture of the mid-diaphysis of the femur. The entrance wound was on the lateral side of the thigh, with the projectile fracturing the femur and then fragmenting in the soft tissues. There were no vascular or nerve injuries documented during the initial admission. The initial hemoglobin level was 9.8 g/dL (98 g/L) (normal range, 14 to 18 g/dL [140 to 180 g/L]) after the intravenous administration of two liters of normal saline solution in the emergency department. The ankle-brachial systolic blood-pressure indices were symmetric at 1.0 each. The bullet wound was treated with irrigation and minor debridement of the bullet path. He underwent uncomplicated closed intramedullary nailing of the femoral fracture approximately five hours after admission. Initial radiographs showed a good reduction of the fracture with retained bullet fragments in the femoral shaft and soft tissues of the thigh (Figs. 1-A and 1-B). The estimated operative blood loss was 200 mL. He received two units of packed red blood cells in transfusion. The hemoglobin level was 13.4 g/dL (134 g/L) on the second postoperative day. The patient was able to walk with the aid of crutches after he had been mobilized with physical therapy. He proceeded postoperatively with uncomplicated weight-bearing and became fully weight-bearing by twelve weeks after surgery. By six months, the fracture was united radiographically. Approximately twenty-one months after the injury, the patient was evaluated for abdominal pain in the emergency department on five separate visits over a one-month period of time. His main symptom was stabbing, cramping abdominal pain, and he also had been having chills and nausea. The pain, as indicated by the patient during these visits, was located in the right upper and lower quadrants of the abdomen or, alternately, was epigastric and in the lower part of the chest, with radiation to the back. The patient also had two short admissions for further evaluation in conjunction with the emergency department visits. He was admitted briefly by general surgery for evaluation of an acute abdomen. An abdominal computerized axial tomographic scan with contrast was performed, demonstrating possible "early obstruction or adynamic ileus." The pain resolved after treatment with milk of magnesia, and the patient was started on a regular diet. He also had a second brief admission for the performance of an esophagogastroduodenoscopy to evaluate the upper gastrointestinal tract. A biopsy specimen that was taken from the gastrointestinal lining was found to be normal stomach tissue. After the procedure, the patient was given a diagnosis of erosive gastritis. During these visits, he did not complain of thigh pain. The patient reported a history of cannabis, narcotic, and cocaine use. The patient's hemoglobin level was <8 g/dL (<80 g/L) at all emergency department presentations. Peripheral blood smears at all emergency department visits showed a microcytic anemia with basophilic stippling. At the time of the last emergency department visit, the patient was admitted and orthopaedic surgery was consulted after it was also noted that the patient had a 10 × 15-cm mass at the anteromedial aspect of the distal portion of the thigh. Physical examination showed diffuse abdominal tenderness. The right thigh mass was mildly tender. Auscultation of the mass demonstrated no bruits. Thigh circumference at the center of the mass measured 52 cm for the affected side and 50 cm for the unaffected side. Hip and knee range of motion were grossly symmetric. The posterior tibial and dorsalis pedis pulses were present and symmetric in both extremities. Anteroposterior and lateral radiographs of the femur (Figs. 2-A and 2-B) showed union of the fracture and the presence of retained bullet fragments near the fracture site. Two main bullet fragments were present; one was more radiodense than the other, suggesting that the less radiopaque fragment was of a nonlead material. Compared with the initial postoperative radiographs, the location of the oval, radiopaque area on the anteromedial side of the fracture site indicated that the fragments had moved. The fragment edges were also blunted in comparison with their appearance on the initial postoperative radiographs. Serum chemistries for potassium, sodium, carbon dioxide, and glucose were all within normal limits. The blood urea nitrogen level was 11 mg/dL (3.93 mmol/L), and the serum creatinine level was 1.2 mg/dL (106 µmol/L). On the day of admission, the patient's complete blood-cell count showed a hemoglobin value of 7.1 g/dL (71 g/L) (normal, 14 to 18 g/dL [140 to 180 g/L]), a mean corpuscular cell volume of 66.8 fL (normal range, 80 to 100 fL), and a mean corpuscular hemoglobin of 20.8 pg/cell (normal range, 26 to 34 pg/cell). The peripheral blood smear again showed basophilic stippling. The serum level of iron was normal at 114 µg/dL (20.4 µmol/L; normal range, 45 to 182 µg/dL [8.1 to 32.6 µmol/L]); the total iron binding capacity was normal at 262 µg/dL (46.9 µmol/L; normal range, 250 to 425 µg/dL [44.8 to 76.1 µmol/L]); and the percentage of iron saturation was normal at 44% (normal range, 15% to 50%).
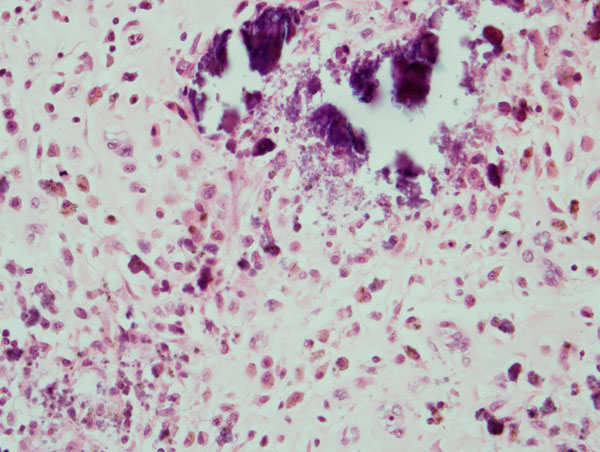
The whole-blood lead concentration was 306 µg/dL (14.68 µmol/L). A twenty-four-hour urine lead concentration was 6519 µg/L (31.4 µmol/L; normal range, 0 to 23 µg/L [0 to 0.11 µmol/L]). Free erythrocyte protoporphyrin was also elevated at 101 µg/dL (1.81 µmol/L; normal, <20 µg/dL [<0.36 µmol/L]). The zinc-complexed protoporphyrin level was 608 µg/dL (10.94 µmol/L; normal, <60 µg/dL [<1.08 µmol/L]). A computerized axial tomographic scan showed a large mass, measuring 8 × 5 cm in the anterior-posterior plane and 12 to 13 cm in craniocaudal length, lying within the anteromedial aspect of the thigh. Internal Hounsfield unit values were between 50 and 70, which suggested a complex fluid or soft-tissue collection. The superficial femoral artery was obscured by artifact for approximately 2 cm of its length near the adductor hiatus. Because of the proximity to the major vessels, computerized axial tomography angiography was also done, showing the vessels to be intact, although the adventitia of the femoral artery may have been involved in the mass. To complement this study, an ultrasound evaluation was performed to assess vascular anatomy. The superficial femoral artery was found to pass as close as 1 cm to the posteromedial side of the mass, but it did not have obvious communication with or vascular flow within the mass, which appeared nearly completely anechoic. There was no evidence of an arteriovenous malformation or detectable blood flow within the cyst. After admission, the patient's mental status changed over the course of one day. Initially, he was able to walk and was oriented to person, place, and time. He had appropriate conversations with health-care providers. He then became agitated and combative and required restraints. He became delirious, which was manifested by rambling incoherent speech and hallucinations. He then displayed a reduced level of consciousness and was intubated. The patient was diagnosed with lead poisoning and was started on chelating agents of intramuscular dimercaprol (British anti-Lewisite [BAL], 100 mg/mL solution) at a dosage of 4 mg/kg every four hours. Edetate calcium disodium (calcium-ethylene diamine tetra-acetic acid [Ca-EDTA], 200 mg/mL) was then started four hours after the initial dimercaprol dose and continued for five days. Four days after the diagnosis of lead toxicity, after radiographic evaluations of the limb, the patient was taken to the operating room. A 14 × 8-cm mass was removed through an anteromedial incision. There was approximately 1200 mL of turbid yellow fluid within the mass, as well as remnants of the bullet's lead core and jacketing. The lead core was smooth and oval in shape. Microbiological cultures of the fluid were obtained. The wall of the cyst contained gray particles similar to the lead color of the bullet. Postoperative radiographs demonstrated removal of the radiopaque material present earlier in the anteromedial aspect of the thigh. A sodium rhodizonate test was done to confirm the presence of lead in the cyst wall. This is a standard test used by forensic scientists to confirm the presence of lead. It is a qualitative test used most commonly to detect lead gunshot residue on clothing or skin in forensic cases. It is both very specific and sensitive for the detection of lead. Our test confirmed the presence of lead in unstained, deparaffinized sections of the cyst wall. The test result was negative when biopsy tissue from the patient's stomach was prepared in a similar manner. Postoperatively, the patient's mental status improved. He required less sedation, was less agitated and combative, and responded to commands. He was then extubated, did not report hallucinations, and spoke in a coherent manner. He quickly improved and was transferred to a general inpatient floor, without interventional monitoring, for the remainder of the hospitalization. The cultures showed no growth of either aerobic or anaerobic organisms at seventy-two hours after surgery. On the day of surgery (three days after the initiation of chelation therapy) the whole-blood lead concentration had dropped to 66 µg/dL (3.19 µmol/L). By the second postoperative day, the whole-blood lead concentration dropped even more, to 25 µg/dL (1.21 µmol/L), and it was 43 µg/dL (2.08 µmol/L) by the seventh postoperative day. He was given oral Chemet (succimer) for nineteen days (500 mg three times a day for five days, and then 500 mg twice a day for fourteen days), as well as zinc, iron, calcium, and multivitamin nutritional supplements. The whole-blood lead concentration was 57 µg/dL (2.75 µmol/L) at five weeks after surgery, and it was the same when measured at ten weeks. The surgical wound healed uneventfully. The patient declined subsequent chelation therapy, but he did not have the mental status changes or abdominal pain that was present preoperatively. The patient was questioned on multiple occasions about other sources of lead, including the ingestion of paint or illegal distillery products or other illicit drug use. The patient's responses to all of these questions were negative. The patient was seen for follow-up at five, eight, and eleven months postoperatively. He was again asymptomatic for the mental status changes and abdominal pain that he had displayed preoperatively. His affect was normal, and he engaged in an appropriate conversation with the health-care provider. He walked with a mild limp. At the eight-month follow-up visit, the patient had a whole-blood lead concentration of 38 µg/dL (1.84 µmol/L).
Proceed to Discussion >>Reference: Dougherty PJ, van Holsbeeck M, Mayer TG, Garcia AJ, Najibi S. Lead toxicity associated with a gunshot-induced femoral fracture. A case report. J Bone Joint Surg Am. 2009;91:2002-8.
Formation of cysts in association with gunshot wounds has occurred with joint, spine, and bone injury. Dissolution of bullet fragments within the cyst or the joint, creating a "lead arthrogram," has been associated with increased serum lead concentrations. This case is unusual in that a cyst formed in an extra-articular location as the result of the residual gunshot fragments. Dissolution of the lead fragments occurred in the cyst fluid or through phagocytosis by the macrophages, allowing lead to be absorbed into the bloodstream. Lead toxicity due to retained bullet fragments is unusual, particularly for patients with extra-articular wounds of the extremities. In general, extra-articular gunshot fragments cause a small increase in the blood lead concentration. McQuirter et al. surveyed 502 patients who sustained gunshot wounds and attempted to follow the patients for two years. At one year, 309 patients were available for follow-up. The authors found that blood lead concentrations increased for as much as three months. Risk factors for increased blood lead concentration included the presence of a fracture, a large number of retained fragments, and the presence of fragments near a bone or joint. The authors set a criterion of ≥10 µg/dL [≥0.48 µmol/L] as a threshold for increased blood lead concentration, noting that 2.1% of the patients met this criterion on the first day after injury and 38.1% had blood levels that were over this threshold at three months. The percentage of patients with blood levels that were over this threshold declined after this time period. The authors recommended that, for patients with gunshot wounds, the blood lead concentration should be determined monthly for three months and then again at one year after injury. Nguyen et al. compared the blood lead levels of 120 adults who had an extra-articular gunshot wound in an extremity with 120 age and sex-matched patients who had no gunshot wound. The authors found a significant increase in the average blood lead concentration when they compared the control group with the gunshot wound group (3.16 µg/dL [0.15 µmol/L] compared with 6.71 µg/dL [0.32 µmol/L], respectively). Five of the patients with a gunshot wound had a blood lead concentration in excess of 20 µg/dL (0.97 µmol/L), whereas none in the control group did. Fluid-filled cysts surrounding a bullet have been described in association with gunshot wounds of the chest wall. Linden et al. described two such patients. One presented with a soft-tissue abscess three months after injury, and the other presented with an uninfected cyst four years after injury. The second patient was noted to have a blood lead concentration of 67 µg/dL (3.24 µmol/L). Weinrach et al. described a patient in whom a cyst-encased bullet fragment, proximal to the elbow, had been present for twenty-eight years. This patient differed from ours in that the radiographs showed no evidence of dissolution of the bullet or a radiopaque lining of the cyst. The authors also did not report lead toxicity. The bullet was removed because of a rapidly increasing size of the cyst. Modern handgun bullets are constructed with a thin metal jacketing surrounding the core, which usually consists of lead and 1% to 1.5% antimony, which is used to harden the lead. The jacketing that surrounds the lead core consists most often of copper and zinc alloy. The bullet may be deformed or fragmented as it passes through tissue. The bullet and its fragments then tend to become walled off within a fibrous capsule, and therefore will not dissolve over time. The routine removal of bullet fragments for gunshot wounds of extremities has not been recommended because of the associated morbidity that accompanies surgery; thus, patients often retain bullet fragments for long periods of time after injury. Lead toxicity can occur as a result of retained bullet fragments. Lead becomes soluble in organic acids, such as synovial fluid, which is why increased blood lead concentrations are seen with intra-articular injuries. In the case of our patient, a cyst developed, most likely as the result of chronic irritation. Lead was dissolved in the fluid milieu. Additionally, macrophages may have put the lead into circulation via phagocytosis. The cyst had lead particulates in its wall, which had vascular communications to the surrounding soft tissues. Photomicrographs also showed the presence of macrophages surrounding the cyst and the presence of particles undergoing phagocytosis within the cyst wall (Fig. 3). The radiographic appearance of the bullet itself changed over the course of time as the bullet developed smooth edges and decreased in size. Lead is stored in bone, blood, and soft tissues. Approximately 90% to 95% of it is stored in bone, where it takes the place of calcium in the calcium hydroxyapatite. The half-life of lead in bone is twenty to thirty years. The half-life of lead in blood is approximately thirty days, and excretion is via the biliary and renal systems. A hypermetabolic state can mobilize bone stores and increase the blood lead concentration, causing a patient to become symptomatic. Hypermetabolic states can occur with pregnancy, infection, hyperthyroidism, Paget disease, neoplasia, or with medicinal or recreational drug use. Additional metabolic stressors that may increase lead mobilization include fractures, surgery, and diabetic ketoacidosis. Surgeons should be aware of the symptoms of lead toxicity. The symptoms are vague, and multiple target organs can be affected. Because of this, the diagnosis of lead toxicity is often delayed. Patients with lead toxicity most often present with symptoms such as fatigue, malaise, abdominal complaints (pain, nausea, vomiting, constipation), headache, or joint pain. Patients can also have difficulty with memory, attention span, and behavior. Signs of lead toxicity include microcytic and/or hypochromic anemia, encephalopathy, peripheral nerve changes due to demyelination of motor axons, and chronic renal failure. Encephalopathic conditions that can occur later in the disease include cerebral edema and seizures. Treatment of lead toxicity is based on symptoms and the results of laboratory tests, particularly the results for blood lead concentration. "Acceptable" levels of lead are somewhat controversial. In their recent review article, Gracia and Snodgrass cite Occupational Safety and Health Administration (OSHA) standards as being a blood lead concentration of <40 µg/dL (<1.93 µmol/L) in adults and <10 µg/dL (<0.48 µmol/L) in children. Others have indicated that a concentration of >20 µg/dL (>0.97 µmol/L) is abnormal for adults and that potential harm to children can occur even when concentrations are <10 µg/dL (<0.48 µmol/L). It is recommended to remove an adult from the occupational exposure if the blood concentration of lead is >40 µg/dL (>1.93 µmol/L). The recommendations for women who are pregnant are much lower than that because of the potential for decreased physical and neurological development of the fetus in the perinatal period, as well as the increased risk of maternal hypertension; pregnant women should avoid occupational exposure that would lead to a blood lead concentration of >5 µg/dL (>0.24 µmol/L). These levels are based on chronic exposure and may not apply to the setting of gunshot wounds. Removal of the lead bullet and/or fragments in patients with intra-articular involvement is recommended because of the mechanical damage that occurs to the articular cartilage over time and also because lead solubility in the synovial fluid can lead to lead absorption. There are no strict guidelines available about when patients with gunshot wounds should be tested to determine blood lead concentration. McQuirter et al. and Nguyen et al. both reported that blood lead concentration was very low in patients with extra-articular gunshot wounds. McQuirter et al. recommended that baseline blood lead concentration levels should be determined at the time of initial treatment and that a second level should be determined before the time of discharge from the hospital or at two weeks after the injury; after that, levels should be assessed monthly until three months after the injury, with a final surveillance performed at one year after the injury. Chelation therapy is done to reduce the concentration of lead in the bloodstream. This treatment may also mobilize stores of lead in bone. The chelating agents bind the lead and allow for excretion of the lead chelation moiety through the renal and biliary systems. The most commonly used chelating agents are dimercaprol, edetate calcium disodium, and succimer. Dimercaprol is the primary chelating agent for patients with encephalopathy or severe symptoms of lead toxicity. Patients with glucose-6-phosphate dehydrogenase deficiency should not receive dimercaprol due to the risk of hemolysis. Edetate calcium disodium is also a very effective lead chelating agent and is administered in a dosage of 1 to 1.5 g/m2 per day intravenously. This medication may cause redistribution of lead to the central nervous system and should only be initiated four hours after the administration of dimercaprol. Succimer is an analog of dimercaprol.
Reference: Dougherty PJ, van Holsbeeck M, Mayer TG, Garcia AJ, Najibi S. Lead toxicity associated with a gunshot-induced femoral fracture. A case report. J Bone Joint Surg Am. 2009;91:2002-8.
Serum amylase and lipase
Liver function tests
Serum lead level
Serum drug-level screen for narcotics
Indium-labeled white-blood-cell nuclear scan





 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3
Fig. 3